Protecting All Children's Teeth: Common Oral Pathology
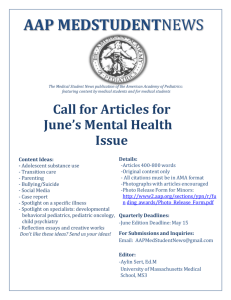
advertisement

Protecting All Children’s Teeth Common Oral Pathology 1 www.aap.org/oralhealth/pact Introduction Mouth pain is a common presenting complaint in the primary care office. It is imperative that pediatric health care professionals feel comfortable in the proper diagnosis, management, and triage of common oral pathology. 2 www.aap.org/oralhealth/pact Learner Objectives Upon completion of this presentation, participants will be able to: 3 Recall the common causes, bacterial flora, management, and possible sequelae of dental abscesses. Describe the common clinical signs, symptoms, and management options of Temperomandibular joint (TMJ) disorders. Define and discuss the term referred pain as it relates to the mouth. Discuss the clinical presentation, causative agents, diagnosis, and management of primary gingivostomatitis, herpangina, hand-foot-mouth disease, and thrush. List the 2 common conditions that cause "strawberry tongue.” Abscess A dental abscess is a collection of purulent fluid caused by a bacterial infection. The most common cause of a dental abscess is extension of the dental caries process into the pulp of the tooth. 4 Used with permission from Miller Medical Illustration & Design www.aap.org/oralhealth/pact Abscess, continued Abscesses can also be caused by trauma to the tooth that allows bacteria to enter the pulp. An abscess limited to the tooth structure (pulpitis) will often present with tooth pain from the increased pressure on the nerve endings within the pulp. This pain is often worsened with heat or cold exposure. 5 Used with permission from Melinda B. Clark, MD; Associate Professor of Pediatrics at Albany Medical Center www.aap.org/oralhealth/pact Abscess Progression If the infection in the pulp extends beyond the tooth, a periapical abscess will develop. Used with permission from Noel Childers, DDS, MS, PhD; Department of Pediatric Dentistry, University of Alabama at Birmingham 6 The pressure caused by the expanding area of necrosis and inflammation causes visible swelling and may lead to slight extrusion of the tooth from the socket (as shown in the x-ray to the left). www.aap.org/oralhealth/pact Abscess Progression, continued As the abscess expands, the pus will spread to contiguous surfaces along the path of least resistance to form a fistula to the maxillary, mandibular, or palatal mucosa. Used with permission from Noel Childers, DDS, MS, PhD; Department of Pediatric Dentistry, University of Alabama at Birmingham 7 www.aap.org/oralhealth/pact Cellulitis If the infection remains unchecked, an abscess can progress to facial, submandibular, or sublingual cellulitis. Facial cellulitis presents clinically with swelling, warmth, and tenderness to palpation along the jaw. A child with facial cellulitis should be referred for immediate ER evaluation or admitted to the hospital for IV antibiotics. 8 Used with permission from Noel Childers, DDS, MS, PhD; Department of Pediatric Dentistry, University of Alabama at Birmingham www.aap.org/oralhealth/pact Symptoms of an Abscess Patients with abscess may present with the following symptoms: Headache Fever Periorbital edema or pain Cranial nerve abnormalities. This infection can be life-threatening and must be addressed emergently. 9 www.aap.org/oralhealth/pact Abscess Treatment First-line empiric antibiotic therapy for dental abscesses is penicillin or amoxicillin and clindamycin for penicillin-allergic patients. Suspicion of a dental abscess requires urgent referral to a dentist for definitive care. 10 www.aap.org/oralhealth/pact Abscess Treatment, continued Efforts must be made to locate the site of infection, incise and drain the pus collection, and collect a specimen for culture and sensitivities. An abscessed tooth often must be extracted. Antibiotic therapy is also required, especially in cases of contiguous spread of the infection. 11 www.aap.org/oralhealth/pact Temporomandibular Joint Disorders The temporomandibular joint (TMJ) is the area directly in front of the ear on either side of the head where the upper jaw (maxilla) and lower jaw (mandible) meet. Temporomandibular joint disorders include a range of problems related to this joint. 12 www.aap.org/oralhealth/pact Signs of TMJ Signs of TMJ disorders include: Bruxism Wear of the occlusal surfaces of the teeth due to tooth grinding Joint sounds (clicking and crepitus) Limited mandibular opening Pain, including TMJ pain or headache, may occur but is not always present. 13 www.aap.org/oralhealth/pact TMJ Treatment Referral to a dentist or other professional knowledgeable in treating TMJ disorders is appropriate. Treatment is usually initiated when pain is present. Options include: • Non steroidal anti-inflammatory medication • Soft diet • Warm compresses • Occlusal bite guards • Counseling • Physical therapy 14 www.aap.org/oralhealth/pact Referred Pain Referred pain is felt in an area innervated by a nerve different from that which innervates the primary site of pain. Dental pain can refer to other teeth, the head, ear, eye, periorbital region, or jaw. 15 www.aap.org/oralhealth/pact Referred Pain, continued The following non-oral conditions can cause pain felt in the teeth or mouth: 16 Acute maxillary bacterial sinusitis or acute otitis media Temporomandibular Joint Atypical facial pain Trigeminal neuralgia Migraine headaches Psychogenic Neoplasia, such as leukemia www.aap.org/oralhealth/pact Primary Herpetic Gingivostomatitis Primary Herpetic Gingivostomatitis is caused primarily by herpes simplex virus type 1. Used with permission from Rama Oskouian 17 The primary infection is most severe and usually seen in children younger than 6. www.aap.org/oralhealth/pact Primary Herpetic Gingivostomatitis The clinical syndrome of HSV gingivostomatitis lasts 10-14 days. Diagnosis is usually based on clinical history and exam findings. Clinical presentation includes: Fever and malaise (precede the anorexia, oral findings, and cervical lymphadenopathy) 18 Significant lip and gum swelling, erythema, and bleeding Vesicles on the lips, tongue, and cheeks, which then ulcerate www.aap.org/oralhealth/pact Treatment for Primary Herpetic Gingivostomatitis Treatment is mainly supportive with hydration maintenance and pain control. The acyclovir family of antiviral medications may be used for immunosuppressed patients. The infection is life-long, and recurrences occur as “cold sores” (herpes labialis), usually at times of stress or infection. Used with permission from Rama Oskouian 19 Herpes Labialis www.aap.org/oralhealth/pact Coxsackie Viral Infections Herpangina Coxsackie viral infections include Herpangina and Hand-Foot-Mouth Disease. Fever, malaise, sore throat, and anorexia precede appearance of the vesicles. Cervical lymphadenopathy is also present. Used with permission from the AAP Red Book Symptoms last 7-10 days. 20 Treatment is supportive care. www.aap.org/oralhealth/pact Oral Candidiasis White plaques or pseudomembranes are noted on the surface of the tongue and/or the buccal, labial, and gingival mucosa. Used with permission from Noel Childers, DDS, MS, PhD; Department of Pediatric Dentistry, University of Alabama at Birmingham 21 Removal of the plaques shows underlying raw, red, bleeding mucosa. Oral surfaces may become painful, which can interfere with feeding. Oral Candidiasis is common in infants, but triggers for all age groups include systemic antibiotic use, inhaled steroids, diabetes, xerostomia, and poor oral hygiene. www.aap.org/oralhealth/pact Oral Candidiasis, continued Oral Candidiasis can be treated with topical antifungal agents, such as Nystatin or Clotrimazole. Used with permission from ANZ Photography 22 If symptoms persist or recur shortly after discontinuation of the antifungal agent, consider reinfection from bottles, pacifiers, or breastfeeding (with maternal breast colonization) or resistance to antifungal medication. www.aap.org/oralhealth/pact Strawberry Tongue Strawberry Tongue refers to an inflamed tongue. It presents as either a diffusely erythematous tongue with prominent fungiform papillae or a tongue covered by a white membrane except for the fungiform papillae that appear red. 23 Used with permission from the AAP Red Book www.aap.org/oralhealth/pact Strawberry Tongue, continued Strawberry Tongue is associated with Group A Beta Hemolytic Strep and Kawasaki syndrome. Group A Beta Hemolytic Strep causes erythematous and enlarged tonsils with white exudates, anterior cervical lymphadenopathy, and fever. Clinical presentation of Kawasaki syndrome is 5 days of fever associated with other clinical criteria, including oral mucosal findings such as a strawberry tongue. 24 www.aap.org/oralhealth/pact Question #1 Which of the following signs is not expected to be seen in a Temporomandibular Joint (TMJ) disorder? A. Swelling and erythema over the joint B. Clicking of the joint C. Wearing of the occlusal surfaces of the teeth D. Limited jaw opening E. Crepitus over the joint 25 www.aap.org/oralhealth/pact Answer Which of the following signs is not expected to be seen in a Temporomandibular Joint (TMJ) disorder? A. Swelling and erythema over the joint B. Clicking of the joint C. Wearing of the occlusal surfaces of the teeth D. Limited jaw opening E. Crepitus over the joint 26 www.aap.org/oralhealth/pact Question #2 What is the most common cause of a dental abscess? A. Trauma to the tooth B. Ludwig's angina C. Extension of the dental caries process into the pulp of the tooth D. Bruxism E. Facial cellulitis 27 www.aap.org/oralhealth/pact Answer What is the most common cause of a dental abscess? A. Trauma to the tooth B. Ludwig's angina C. Extension of the dental caries process into the pulp of the tooth D. Bruxism E. Facial cellulitis 28 www.aap.org/oralhealth/pact Question #3 Which of the following conditions can cause pain in the teeth or mouth? A. Migraine headaches B. Acute maxillary bacterial sinusitis C. Leukemia D. Acute otitis media E. All of the above 29 www.aap.org/oralhealth/pact Answer Which of the following conditions can cause pain in the teeth or mouth? A. Migraine headaches B. Acute maxillary bacterial sinusitis C. Leukemia D. Acute otitis media E. All of the above 30 www.aap.org/oralhealth/pact Question #4 Which of the following statements about Oral Candidiasis is not true? A. The same fungus causes angular cheilitis B. It should be treated with antiviral medication C. Re-infection from bottles or pacifiers is possible D. It can be triggered by antibiotic use E. It is common in infants 31 www.aap.org/oralhealth/pact Answer Which of the following statements about Oral Candidiasis is not true? A. The same fungus causes angular cheilitis B. It should be treated with antiviral medication C. Re-infection from bottles or pacifiers is possible D. It can be triggered by antibiotic use E. It is common in infants 32 www.aap.org/oralhealth/pact Question #5 Which of the following statements is true when treating an abscess? A. The first step is to locate the site of infection B. In severe cases, intravenous antibiotics are necessary and hospitalization may be required C. An abscessed tooth often must be extracted D. In cases limited to pulpitis, a root canal may be performed to salvage the tooth E. All of the above 33 www.aap.org/oralhealth/pact Answer Which of the following statements is true when treating an abscess? A. The first step is to locate the site of infection B. In severe cases, intravenous antibiotics are necessary and hospitalization may be required C. An abscessed tooth often must be extracted D. In cases limited to pulpitis, a root canal may be performed to salvage the tooth E. All of the above 34 www.aap.org/oralhealth/pact References 1. Avcu N, Gorduysus M, Omer Gorduysus M. Referred dental pain. The Pain Clinic. 2003; 15(2): 173-178. 2. Ferretti GA, Cecil JC. Kids Smile: Oral Health Training Program Lecture Series. Sponsored by the Kentucky Department for Public Health and the University of Kentucky College of Dentistry. 3. Handbook of Pediatric Dentistry. 2nd ed. Cameron AC, Widmer RP (Eds). Mosby; 2003. 4. Krol DM, Keels, MA. Oral Conditions. Pediatr Rev. 2007; 28(1): 15-22. 5. Okeson JP, Falace DA. Nonodontogenic toothache. Dental Clinics of North America. 1997; 41(2): 367-83. 6. Oral Pathology: Clinical Pathologic Correlations. 4th ed. Regezi JA, Sciubba JJ, Jordan RCK (Eds) WB Saunders, St Louis Mo. 2003. 7. Pediatric Dentistry: Infancy through Adolescence. 4th ed. Pinkham JR, Casamassimo PS, Fields HW, McTigue DJ, Nowak AJ (Eds). WB Saunders, St Louis, Mo. 2005. 35 www.aap.org/oralhealth/pact