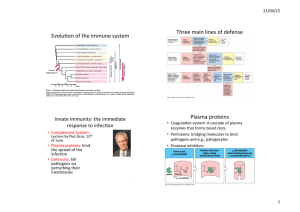
IMMUNOLOGY – INTRODUCTION
advertisement

Elements of the Immune System • Cells of the Immune System • Chemical Mediators – Cytokines, Chemokines, Complement, Eicosanoids • • • • • Apoptosis Acute Phase Response Inflammation Fever Innate/Specific Immunity Cells of the Immune System • Cells of the Immune System (white blood cells [WBCs], leukocyte) • Hematopoietic stem cells to: – Myeloid cell line • Monocytes/macrophages, neutrophils, eosinophils, basophils, megakaryocytes, • erythrocytes (red blood cells [RBCs]) – Lymphoid cell line • B lyphocytes , T lymphocytes, natural killer (NK) cells Cells of the Immune System Hematopoietic cell differentiation; Fig 11-1 Cells of the Immune System • White blood cells distinguished by – Morphology/stain – Function – Cell surface markers • Clusters of differentiation (CD) – Major histocompatibility complex (MHC) antigens » MHC I (CD8) on all nucleated cells » MHC II (CD4) on antigen presenting cells Cells of the Immune System Lymphoid Organs • Primary lymphoid organs (sites of hematopoiesis) – Bone marrow – Thymus – T cell maturation • Secondary lymphoid organs (sites of T cell activation) – – – – Lymph nodes Peyer’s patches Tonsils Spleen Cells of the Immune System • Polymorphonucleocytes (PMNs) or granulocytes refers to neutrophils, eosinophils and basophils. Howerver, term “PMN” generally refers to the most abundant of these, neutrophils • Neutrophils = PMNs = segmented neutrophils (“segs”) – – – – – Take up hemotoxylin (basic) and eosin (acid) (H&E) stains = pink multilobed 50-70% of circulating WBCs Professional phagocytic cell (Immature) band (unsegmented) forms to mature segmented neutrophils • Bacterial infection = mobilization = increased number of neuts with some bands = shift to the left – In blood 7h, in tissues 3 days • 1st line defense against bacteria but short lived Cells of the Immune System • Neutrophils: continued – Granules = lysosomes • Primary (azurophilic) – O2-independent = Elastase, lysozyme, defensins, – O2-dependent = myeloperoxidase • Secondary (specific) – O2-independent = lactoferrin, lysozyme – O2-dependent =NADPH oxidase cofactors Cells of the Immune System • Neutrophils: continued – Receptors for recognition of microbes by neutrophils • Receptors for opsonins – Receptors of complement (C’) proteins – Receptors for Fc portion of Abs • Toll-like receptors (TLRs) • Seven-transmembrane alpha helical receptors; stimulate migration – for bacterial peptides – for chemokines Cells of the Immune System • Mononuclear phagocytes – Monocytes in blood (3-8% of WBC) differentiate into macrophages in tissues – Macrophages (Macs) • Professional phagocytic cells like neutrophils • Terminology: Kupffer cells (liver), histiocytes (CT), microglial cells (brain), osteoclasts, alveolar Macs • “Reticular Endothelial System” (RES) old term referring to all monocytes and macrophages Cells of the Immune System • Macrophages : continued – Contribute to both innate and adaptive immunity – Monocytes in blood for 1 day; Macs live months/years in tissues – Unlike neutrophils, macs proliferate – Antigen-presenting cell (APC) • other APCs = B cells and dendritic cells (DCs) – Respond slower than PMNs but live longer in tissues – Secrete many cytokines: shock – Activated (angry) Macs better killers than neutrophils • Phagocytize more vigorously, use more O2, more enzymes, Cells of the Immune System • Macrophages: continued – Recognition of microbes by macrophages • Receptors for opsonins – Receptors for C’ proteins – Receptor for Fc portion of Abs • Toll-like receptors • Mannose receptors – Bind terminal mannose & fucose on bacterial glycolipids and gl-proteins • Seven-transmembrane alpha helical receptors; stimulate migration – for bacterial peptides – for chemokines Cells of the Immune System • Toll-like receptors (TLRs): from Drysophila “toll” protein = family of membrane proteins on PMNs, Macs, and dendritic cells that recognize microbial molecules. – Stimulate innate immune responses by these cells – TLR receptors on humans cells (TLR-1 – TLR-13) • Recognize pathogen-associated molecular patterns (PAMPs) – LPS, peptidoglycan, teichoic acid, lipoarabinomannan, flagellin, fungal glycans, unmethylated cytosine-guanosine DNA, RNA2, other – Some TLRs need second signal; TLR-4 recognized LPS-CD 14 Cells of the Immune System • Receptors and responses of phagocytes Cells of the Immune System • Phagocytosis/killing of microbes by neutrophils and Macs – Phagocytosis • • • • Phagocytosis = >0.5 um; pinocytosis for smaller particles Microbes adhere to surface receptors which deliver signals Cytoskeleton-dependent process of engulfment Cup-shaped membrane projects around microbe – If projected membranes don’t meet properly, get coiling phagocytosis? • Vacuole “zips-up” and pinches off = phagosome • Phagocytosed microbes (hopefully) killed by neuts and Macs • Phagocytosed microbial peptides presented in surface MHC II molecules of Macs (not neutrophils) Cells of the Immune System • Coiling phagocytosis Cells of the Immune System • Phagocytosis/killing of microbes by neutrophils and Macs – Killing • Phagocytes must be activated to kill – Neuts activated by surface receptors TLR, Fc, C’ receptor – Macs activated by those, mannose receptor, and receptor for IFN-g • Phagosome fuses with lysosome = phagolysosome = killing site • Oxygen-dependent killing by neutrophils and Macs – Phagocyte oxidase in phagolysosome membrane reduces O2 into reactive oxygen intermediates (ROIs) such as superoxide with NADPH – Superoxide dismuted to H2O2 – Neuts - myeloperoxidase converts H2O2 + Cl ions to hypochlorous ions – Macs – inducible nitric oxide synthase (iNOS) catalyses conversion of arginine to citrulline, releasing diffusible NO gas. NO + H2O2 or O2- = toxic radicals • Oxygen-independent killing by neutrophils – enzymes from granules kill Gram negative organisms by disrupting membranes and other mechanisms Cells of the Immune System • Neutrophils vs Macrophages – – – – – – – – Both are professional phagocytic cells Neutrophils move to insult first Macrophages (but not neutrophils) proliferate Macrophages (but not neutrophils) contribute to adaptive immunity Macrophages (but not neutrophils) are APCs Neutrophils (but not macrophages) produce myeloperoxidase Macrophages (but not neutrophils) produce nitric oxide Macrophages are major producers of cytokines • Over-production of Mac cytokines = shock Cells of the Immune System • Mast Cells – Derived from marrow – Relatively large (10-13 um), tissue-residents cells • Connective tissue: skin, lung alveoli, GI mucosa, nasal mucosa – Receptors: (1) IgE antibody (2) TLRs (3) complement – ~100 densely packed metachromatic granules contain Histamine, TNFa, other preformed inflammatory mediators – Activate receptors = degranulation and release of mediators • Inflammation • Immediate hypersensitivity with cross-linking of IgE Cells of the Immune System • Basophils – Similar to mast cells but circulating, different lineage, and small (5-7 um) – Least common circulating WBC - <0.3% – Takes up hematoxylin (basic) stain – blue – High affinity IgE receptors; triggered when Ag binds to IgE – Late phase of IgE-associated allergic reactions in tissues Cells of the Immune System • Eosinophils – Take up eosin = red – 1-6% of circulating WBCs – Granules with phosphatase, peroxidase, basic proteins – Receptors for IgE, IgG, and IgA – Allergic reactions and parasitic infections • Release reactive proteins some toxic to parasitic worms – Phagocytic cell ??? Cells of the Immune System • Megakaryocyte – Large (50-100 um diam) WBC with lg nucleus • Neutrophils have a diameter of 12-15 um – In bone marrow – Produces ~3000 platelets per cell • Platelets are anucleate cytoplasmic fragments • Smallest circulating blood cells (2 um diam) – Erythrocyes 6 um diam with 2 um thickness • 10 day life span in circulation • Form blood clots and release mediators from granules Cells of the Immune System • Dendritic Cells (DCs) = an antigen presenting cell (APC) – Myeloid origin primarily – Terminology • Precursor DCs in circulation • Immature DCs in tissues: capture Ag but do not present; to nodes – Have sticky, octopus-like arms (dendrites) » Fc receptors, mannose receptors, Toll-Like Receptors (TLRs) – Langerhan’s cells in skin • Mature DCs in T-cell zones of lymph nodes; present Ag – Fewer receptors but more MHC-I and II molecules on surface Cells of the Immune System • Lymphocytes: smaller than myeloid leukocytes; lg nucleus and agranular cytoplasm – B cells: APCs; antibody production (plasma cells); memory cells • Surface with Igs, MHC II, C’ receptors – T cells: helper T cells and cytotoxic T cells • 60-80% of blood lymphocytes • Surface with TCR, CD3, CD4, CD8 – NK (natural killer) cells; lg granular • Fc receptors for ADCC • Recognize and kill virally infected cells Cells of the Immune System • Natural Killer (NK) cells – – – – – Large granular lymphocyte (not B or T cells; no surface Ig or TCR) 5-20% of monocytes in blood Stimulated by INFa, INFb, from virally infected cells Stimulated by TNF and ILs from TH1 cells and activated Macs and DCs Granules with perforin, granulysin (creates pores) and granzyme (induces apoptosis) • Like cytotoxic T cells (but cytotoxic T cells = adaptive immunity) – Kills cells with reduced MHC I expression – Activates Macs by secreting INFg – No specific immunity or memory • Similar to neutrophils and Macs in this respect – Also IgG Fc receptors for antibody dependent cell cytotoxicity (ADCC) • adaptive immunity (induced apoptosis) Cells of the Immune System – Activation of responses: How PMNs, Macs, NKs recognize bugs • Macs and PMNs – Opsonin receptors – Receptors for bacterial carbohydrates (mannose) - Macs – Toll-like receptors (TLRs) • Natural Killer cells – Altered surface of virally infected cells » Reduced expression of MHC I antigen » - MHC I on cells inhibits NK cell activation – Receptor for IgG Fc component » For ADCC Cytokines / Chemokines • Cytokines = proteins secreted by immune cells in response to microbes or other antigens (Ags) or other cytokines that mediate inflammatory and immune reactions. Major communicators between immune cells • Chemokines = family of structurally homologous lowmolecular weight cytokines that stimulate movement of leukocytes to tissues Cytokines Interferons (INFs) Type I = mediate innate response to viral infections – INF-a = family of related peptides produced by monocytes – INF-b = single protein produced by fibroblasts and other cells – Although structurally different, bind to same receptor, same responses » paracrine action: virally infected cells secrete to non-infected cells » induce enzymes that interfere with transcription of viral RNA/DNA » increase expression MHC I molecules Type II / INF-g = innate/adaptive response to intracellular infections – Produced by T cells, NK cells – Activates macrophages Cytokines Tumor necrosis factor alpha (TNF-a) - sometimes referred to as “cachectin” (induces weight loss) - produced mainly by activated monocytes / macrophages - NK cells, mast cells, activated T cells also - Recruit and activate neutrophils and monocytes/macrophages to sites - Induce macrophages to secrete chemokines - Stimulate vascular endothelial cells to express adhesion molecules - Low conc = local inflammation - Large conc to circulation: induce fever and promote acute phase response TNF-b – like TNF-a but produced by T cells Cytokines • Interleukins – “made by leukocytes and act on leukocytes” – Interleukin-1 (IL-1) = similar to TNF • Made by activated Macs, neutrophils, endothelial cells, epithelial cells – IL-2 - produced by activated T cells; act in autocrine manner on T cells – IL-3 - multilineage colony stimulating factor; Produced by T cells and promotes expansion of marrow progenitor cells of blood cells. – – – – – IL-4 – produced by T cells; Stimulate IgE production by B cells IL-5 - Produced by T cells; stimulate growth and activation of eosinophils IL-7 - Produced by bone-marrow stromal cells; stimulate B and T cells IL-10 - Produced by activated Macs; inhibits Macs; homeostatic control IL-12 – produced by activated monocytes; stimulates interferon gamma production by T and NK cells; mediator of innate response Chemokines • Chemokines (chemotactic cytokines) = lg family of structurally homologous cytokines produced by various cells in response to inflam mediators that stimulate leukocyte movement and regulate leukocyte migration from blood to tissues. – Alpha chemokines = C-X-C chemokine • Two cysteines separated by one amino acid – Beta chemokines = C-C chemokine • Receptor = seven-transmembrane alpha helical receptor Complement • Complement (C’) = 35 proteins, primaily in plasma – Nomenclature = numbers and letters • “a” usually designates small soluble peptide • “b” usually designates peptide that binds to cell surface – 3 pathways to produce C3 convertase (C3 into C3a and C3b) • Classical: discovered first; activated by Ag/Ab complexes – IgM, IgG1, and IgG3 are isotypes that “fix” C’ • Alternative: activated by bacterial surface compents (LPS) • Lectin: activated by mannose binding lectin (MBL) – C3b + C3 convertase = C5 convertase which cleaves C5 – C5b modifies C6, C7, C8, C9 to membrane attack complex (MAC) Complement • Classical pathway – – – – • IgM>IgG “fix” C1q which activates C1r to cleave C1s Activated C1s cleaves C2 (C2a, C2b) and C4 (C4a, C4b) C4bC2b = C3 convertase C4bC2b binds to C3b = C5 convertase Lectin pathway – Mannose-binding protein (MBP) binds to mannose on cell surface polysaccharides – MBP then binds to MBP associated protein -1 & MASP -2 – MASP-1 and MASP-2 cleave C2 and C4 = C4bC2b = C3 convertase • Alternative (properdin) pathway – – – – – – C3 in plasma spontaneously splits into C3a and C3b; become inactive If C3b binds to bacterial surface component (LPS), becomes stable C3b binds factor B = C3bB Factor D cleaves B from C3bB to C3bBb = C3 convertase Factor P (properdin) stabilizes C3bBb C3bBb binds to another C3b = C3b3bBb = C5 convertase Complement • Complement pathways Complement • C’ products perform multiple functions: – Chemotactic factors: C5a recuit leukocytes – Anaphylatoxins: C3a, C5a promote acute inflammation by causing release of vasoactive mediators from mast cells. – Opsonins: C3b adheres to bacterial cells • Complement receptor CR1 on PMNs, Macs, and B cells • Facilitates phagocygtosis – Membrane Attack Complex: C5b,6,7,8,9 [(C5b,6,7,8)1 (C9)n] C7 is hydrophobic and inserts into lipid bilayers Gram negative bacteria have lipid outer membrane C9 polymerizes at C5-C8 to form pores Water enters cell = swelling and rupture Calcium also enters cells which induces apoptosis Eicosanoids • Eicosanoids = arachidonic acid (AA) metabolites – AA derived from 20 carbon FA in membrane phospholipids – AA produced from membrane with phospholipase A2 • Action of enzyme inhibited by glucocorticoids – – – – Prostaglandins, leukotrienes, thromboxanes Local “hormones” produced by mast cells and other cells Mediator in inflammation after infection or injury Cyclooxygenase pathway - prostoglandins and thromboxanes • Inhibited by aspirin and other NSAIDS – Lipoxygenase pathway – leukotrienes, lipoxins Eicosanoids • Eicosanoid metabolism Eicosanoids • Eicosanoids = arachidonic acid (AA) metabolites – Prostaglandins: • Prostaglandin D2 (PGD2) – binds to receptors on smooth muscle cells and acts as a vasodilator and bronchoconstrictor – Chemotaxis of neutrophils in inflammation – Leukotrienes • Leukotriene C4 (LTC4), LTD4, LTE4 bind to receptors on smooth muscle, causing prolonged bronchoconstriction – asthma • Lipoxins A4 (LXA4) and LXB4 are anti-inflammatory mediators Apoptosis • Apoptosis = DNA cleavage, membrane blebbing, changes in membrane lipid distribution, detachment of cells – Apoptosed cells express molecules recognized by neutrophils • Damaged cells removed cleanly as apposed to necrosis where damaged cells release contents in environment. – Important for eliminating unwanted lymphocytes – Induction by activation/cleavage of series of 14 caspases which cleave cellular elements. Caspases activated by • Intrinsic: mitochondrial membrane of inactive lymphocytes leak; products activate caspase = programmed cell death or death by neglect • Extrinsic: repeatedly activated T cells up-regulate FasL; reacts with Fas on same or adjacent cell • NK cell and cytotoxic T cell release perforin, granulysin and granzyme Acute Phase Response • Acute Phase Response = production of proteins by liver in response to infection, trauma, inflammation, malignancies – Within hrs of event but remain elevated during chronic insults – From IL-1, TNF, INFg, etc by monocytes, Macs, endothelial cells – Unique proteins: • C-reactive protein (CRP) = reacts with C polysaccharide of pneumococci • serum amyloid A (SAA) – – – – Elevated “normal” proteins: C’ components, fibrinogen etc. Other liver protein synthesis reduced: albumin; anemia of chronic disease? Objective evidence for disease in occult infections or diseases Tests • CRP measurement (ELISA) • Erythrocyte sedimentation rate (ESR) increased Erythrocyte sedimentation rate • The erythrocyte sedimentation rate (ESR), also called a sedimentation rate, is the rate at which RBCs precipitate in a period of 1 hour. It is a non-specific measure of inflammation. To perform the test, anticoagulated blood is placed in an upright tube, and the rate at which the RBCs fall is measured and reported in mm/h. • The ESR is governed by the balance between prosedimentation factors, mainly fibrinogen, and those factors resisting sedimentation, namely the negative charge of the erythrocytes (zeta potential). When an inflammatory process is present, the high proportion of fibrinogen in the blood causes red blood cells to stick to each other. The red cells form stacks called 'rouleaux' which settle faster Inflammation • Inflammation = complex reaction to microbes & necrosis – – – – – – Vascular responses, migration/activation of leukocytes, systemic Destroy, dilute, wall off injury Injured tissue replaced by fibrous tissue = scarring and repair Mediated by chemical factors Terminated when insult eliminated and by anti-inflam mechanisms Types of inflammation • Acute = rapid onset (seconds or minutes), short duration (hrs, days) with exudate and neutrophils • Chronic = slow onset with long duration and characterized by macrophages and lymphocytes, new blood vessels, fibrosis, (granulation tissue), tissue necrosis Inflammation • Acute Inflammation – Vessel dilation, leaky microvasculature, emigration of cells & fluid – Fluid migration from circulation to tissues: • Transudate = normal, low protein content, sp gravity < 1.012 • Exudate = with inflammation; high protein, cells – Edema = fluid but few cells – Purulent (pus) = lost of cells, mostly neutrophils – Stimuli • • • • Infections Trauma, tissue necrosis, foreign bodies Chemical agents Hypersensitivity reactions Inflammation • Acute inflammation: continued – Vasodilation induced by histamine, NO on vascular sm muscle – Leaks due to endothelial gaps in venules • Histamine, leukotrienes – Primarily from mast cells – rapid contraction of cytoskeletal proteins • IL-l, TNF, INFg = delayed, endothelial cell retraction – Extravasation of leukocytes • Margination of leukocytes with slowing of blood flow • Rolling = leukocyte transient adherence to endothelial cells – Adherence due to up-regulation of selectins, integrins, other – Mediated by histamine, platelet activating factor (PAF), TNF, IL-1, • Pavementing = leukocytes firmly adhere to endothelial cells • Diapedesis = movement of leukocytes thru vascular wall to tissues Inflammation • Leukocyte migration from blood vessels; Robbins Fig 2-6 p 53 Inflammation • Acute inflammation: continued – Chemotaxis = migration of leukocytes to site of injury • MOA – “chemotactant” binds to specific receptor on leukocyte – Action of second messengers result in polymerization of actin – Pseudopodia extension and fusion • “chemoattractants” = chemokines, C5a, leukotriene B4, bact. proteins – Termination of response • Stimulus ends, mediators short-lived • Anti-inflammatory cytokines – Lipoxins LXA4 and LXB4 – Transforming growth factor B (TGF-B) from Macs Inflammation • Chronic inflammation = simultaneous inflammation, tissue destruction and attempts to repair – Causes: • Persistent infection - tuberculosis • Prolonged exposure to toxic agent – Exogenous = silicosis – Endogenous = arthrosclerosis • Autoimmunity – Morphological features • Infiltration with mononuclear cells (Macs, lymphocytes, plasma cells) • Tissue destruction from agent and inflammatory cells • Attempts to heal by connective tissue replacement Inflammation • Chronic inflammation: continued – Mononuclear cell infiltration • Macrophages are the major player – blood monocytes live 1 day, tissue Macs live months to years – Overtake neutrophils as predominant cell type by 48h – Macrophages proliferate (unlike neutrophils) • Lymphocytes - recruited by IL-1, TNF, and chemokines from Macs – Secrete INFg which activates Macs (bidirectional interaction) • Eosinophils: for IgE mediated reactions – parasitic infections Inflammation • Chronic inflammation: continued – Granulomatous inflammation – granuloma formation • Persistent infection or stimulus • Aggregation of macrophages that are transformed into epithelium-like cells (epitheloid cells) – Giant cells = epitheloid cells that fuse together • Focus surrounded by collar of lymphocytes (and some plasma cells) • Older granulomas develop rim of fibroblasts and CT – Note – different from granulation tissue which is the tissue of early repair (24 h after injury) characterized by angiogenesis and fibroblast proliferation Fever • Fever = pyrexia = > 1oC – Neural pathways for thermoregulation in hypothalmus – Cytokines of innate immune system (TNF, IL-1 = endogenous pyrogens) bind to receptors on vascular endothelial cells in hypothalmus. Endothelial cells then produce prostagland PGE2, and other eicosanoids that reset hypothalmic thermoregulatory center. • LPS, other products = exogenous pyrogens (stimulate leukocytes to release cytokines) • NSAIDS inhibit cyclooxygenase; block prostaglandin synthesis – Fever of unkown origin (FUO) = >101F for 3 weeks • Caused by infections, rheumatic fever, sarcoidosis, neoplastic diseases, drugs – Note: pyogen = pus pyrogen = fever Innate Immunity • Protection against infection that relies on mechanisms that exist before infection – First line of defense • Barriers – Skin (epidermis and dermis) – Mucous membranes: respiratory, GI, genitourinary tracts – Lacrimal apparatus: tears – Saliva – Epiglottis • Chemical – Sebum: acids – Perspiration: lysozyme – Gastric juice – Urine – transferrin Innate Immunity • Protection against infection that relies on mechanisms that exist before infection – Second line of defense • • • • • Phagocytosis Inflammation Fever Complement Intererron Adaptive Immunity - Protection that develops after exposure to an agent and is specific for that agent - Humoral immunity – for intracellular and extracellular pathogens • antibodies (Abs) – Prevent reinfection and spread – Eliminate agent » opsonization; ab interacts with both agent and host cell) » Fix complement (C’) (opsonization, bactericidal Ab) – Large number (polyclonal) ; non-self – Surface receptors on B cells - Cell-mediated immunity (CMI) • Up-regulated Macs • Cytotoxic T cells