Prenatal Development
advertisement

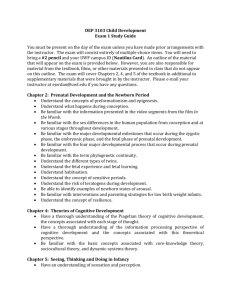
Germination Stages of Prenatal Development Genetics Inherited Diseases Neonates Germination Humans start off as a single cell organism: Gametes: The male/female reproductive cells Zygote: Formed an hour after the sperm enters the ovum when the two gametes fuse Genes: Blueprints for creating a person 25,000 of them Composed of DNA molecules _______________________________________________________________ Deoxyribonucleic Acid: (DNA) Located along 46 chromosomes which are organized in 23 pairs. Each parent provides 23 chromosomes. Possible combinations are limitless. Nearly all of the cells of the body will contain the same 46 chromosomes as the zygote. Prenatal Development Typically divided into Trimesters: First: Conception to 3 months Second: 3 to 6 months Third: 6 to 9 months The division of pregnancy into trimesters is arbitrary and has no significance with regard to prenatal development. Prenatal Development Conception Occurs the moment a sperm cell fertilizes the ovum (egg cell), forming a single-celled zygote. Prenatal Development Three Stages of Prenatal Development: Germinal (2 weeks) Begins with conception. Takes place in one of the fallopian tubes. Zygote travels to the uterus and attaches itself to the uterine wall. Rapid cell division occurs Once the zygote is successfully attached the germinal stage is over. Embryonic (6 weeks) Developing embryo forms all the major body systems, organs, and structures. Lasts from the beginning of week 3 through week 8. Begins when the zygote attaches itself to the uterine wall. Ends when the first bone cells form. 1 inch long and weighs 1/7 of an ounce. Embryo already resembles a human being. Fetal (38 weeks) Lasts from week 9 (when first bone cells form) until birth. Experiences rapid growth and further development of body structures, organs, and systems. Prenatal Development Teratogen (any agent that causes birth defects): Drugs (prescription, nonprescription) Alcohol, tobacco Environmental pollutants Infectious diseases Nutritional deficiencies Maternal stress Advanced age of a parent Severity of damage to the unborn depends on: Dose Time of exposure Genetic susceptibility Teratogens and Timing of Their Effects on Prenatal Development Zygote 1 2 3 Embryonic period (wks) 4 5 6 7 Fetal Period (wks) 8 9 16 32 Central nervous system Heart Most serious damage from teratogens in first 2-8 wks Arms Eyes Legs Ears Teeth Period of susceptibility to structural defects Period of susceptibility to functional defects Palate External genitalia 38 Prenatal Development Fetal alcohol syndrome: Abnormalities in newborn due to mother’s heavy use of alcohol in pregnancy Abnormalities include: Facial deformities Defective limbs, face, heart Most are below-average intelligence Some are mentally retarded Moderate drinkers during pregnancy have babies who were less attentive and alert even at 4 years of age. Prenatal Development Maternal smoking can cause: Respiratory problems SIDS ADHD Low birth weight Prenatal Development Illegal drugs that harm during pregnancy: Cocaine (norcocaine) Marijuana Heroin Incompatible blood types (Rh factor) Environmental hazards exposure to radiation or chemicals STDs, HIV infection, AIDS Mother to child transmission of HIV is a serious issue in Africa today. Multiple Births Less than 3% of all cases result in twins Any more is far less Two types of twins: Monozygotic (Maternal twins): Identical Dizygotic (Fraternal): Completely different individuals Mothers carrying multiple children run a higher risk of premature delivery and birth complications. Is it a boy or a girl? 23 matched pairs of chromosomes: 22 of them copy their pair. 23rd chromosome: Determines sex XX: females (Two matching, relatively large chromosomes) XY: males Female contributes an X chromosome. Male can contribute either an X or a Y. If the father contributes a Y chromosome then the infant will be male. Father who determines the sex of the child. Genetics Genetics and Traits: Dominant: Expressed trait when two competing traits are present. Recessive: Trait within an organism that is present, but is not expressed. Examples: Eye color, skin tone, and cleft pallet Genotype: Underlying combination of genetic material present. Not physically visible Phenotype: Observable trait The trait that is actually seen. Genetics Homozygous: Inheriting from parents similar genes for a given trait. Heterozygous: Inheriting from parents different forms of a gene for a given trait. Polygenic inheritance: Inheritance in which combination of multiple gene pairs is responsible for the production of a particular trait. X-linked genes: Genes that are considered recessive and located only on the x chromosome. Human Genome Project Reached in 2001: When molecular biologists succeeded in mapping the specific sequence of genes on each chromosome. Most important moment in the history of genetics. Discovered that 99.9% of the gene sequence is shared by all humans. Behavioral Genetics: Studies the effects of heredity on behavior and psychological characteristics Inherited Diseases Down Syndrome: Disorder produced by the presence. of an extra chromosome on the 21st pair. Most frequent cause of mental retardation. Fragile X Syndrome: Produced by injury to a gene on the X chromosome. Producing mild to moderate mental retardation. Inherited Diseases Sickle-cell Anemia: Blood disorder Gets its name from the shape of the red blood cells. Symptoms: Poor appetite, stunted growth, swollen stomach, and yellowish eyes. Most sever form of the disease rarely live beyond childhood. Affects one African-American in 400. Inherited Diseases Tay - Sachs Disease: Produces blindness and muscle degeneration prior to death No treatment. Usually causes death before its victims reach school age. Klinefelter’s Syndrome: Presence of an extra x chromosome. Produces underdeveloped genitals, extreme height, and enlarged breasts. Inherited Diseases Genetic Counseling: Discipline that focuses on helping people deal with issues relating to inherited disorders. Prenatal Testing Ultrasound Sonography: High-frequency sound waves scan the mother’s womb to produce an image of the unborn baby. Size and shape can be addressed. Chorionic villus sampling: (CVS) Finds genetic defects. Involves taking samples of hair like material that surrounds the embryo. Prenatal Testing Amniocentesis: Identifies genetic defects Examines a small sample of fetal cells drawn by a needle. Inserted into the amniotic fluid surrounding the unborn fetus. 15-20 weeks into pregnancy. Nearly 100 percent accurate. Fetal Blood sampling: (FBS) After 18 weeks of pregnancy. Collects a small amount of blood from the umbilical cord. Detects Down syndrome and most other chromosome abnormalities. Neonates Labor: The Process of Birth Begins Oxytocin: Released by the mother’s pituitary gland. When the concentration of oxytocin is high enough, mother’s uterus begins periodic contractions. Braxton-Hicks Contractions: (After 4th month) False labor Contractions will eventually get strong enough to force the fetus down the birth canal until the baby enters the world. Cone-head (Don’t Panic!) Neonates: The Stages of Labor Most labors take 16-24 hours for firstborn children. Duration of labor can vary depending on mother’s: Age Race Ethnicity Number of prior pregnancies Neonates: The Stages of Labor Stage 1: (Longest stage) Uterine contractions every 8-10 minutes Last 30 seconds Toward the end contractions occur every 2 minutes Last 2 minutes As the contractions increase the cervix (separates uterus from the vagina) becomes wider Eventually expanding to allow the baby’s head to pass through Transition: Final part of the first stage Fully opened cervix is usually around 10cm Stage 2: (Approx. 90 min) Episiotomy: Incision made to increase the size of the vagina to help in stretching Is it ethical? Baby’s head emerges from the mother Stage ends when the baby has completely left the mother The placenta is still inside the mother at the end of this stage Neonates: The Stages of Labor Stage 3: (Quickest stage) Expelling of the umbilical cord and placenta Lasts just a few minutes In most cases once a baby makes it outside they spontaneously cry, which helps them to clear their lungs of fluid If they don’t the child may need to be stimulated or startled to make it cry If it still does not: Immediate life saving attention may be necessary Neonates: Apgar Scale Rhythm: Repetitive, cyclical pattern of behavior. Important way that behavior can become integrated in the neuronal system and aide in the learning Circadian Rhythm State: Degree of awareness that an infant displays to both internal and external stimulation. Alertness, fussing, crying, and different levels of sleep. How much stimulation is necessary for a reaction Neonates: Apgar Scale Apgar Scale Defined: A standard measurement system that looks for a variety of indications of good health in newborns. Evaluates 5 basic qualities: Appearance (color) Pulse (heart rate) Grimace (reflex irritability) Activity (muscle tone) Respiration (respiratory effort) Scoring: From 0-2 on each of the five qualities Score total ranges from 0-10 Prognosis: Score from 10 down to 8 means that the child is fine Score from 7 down to 4 will most probably need help to start breathing Score less than 4 means that the child needs immediate life-saving attention The Apgar Scale Score Body Color Heartbeat Reflex Irritability Muscle Tone Respiratory Effort 0 1 2 Blue, pale Body pink, extremities blue Absent Slow – less than Fast – 100 to 140 100 beats per min. beats per min. No response Grimace Limp and flaccid Inactive, weak, Strong, active some flexion of motion extremities Irregular and slow Breathing good with normal crying Breathing for no more than 1 min. Entire body pink Coughing, sneezing, crying Neonates: If the Child does not Pass the Apgar Scale Average infant weights: 7 ½ pounds Infant Mortality: Death within the first year of life Anoxia: Lack of oxygen If lasts longer than a few minutes can cause mental retardation Stillbirth: Delivery of a child who is not alive Less than 1 in 100 Neonates: If the Child does not Pass the Apgar Scale BIRTH COMPLICATIONS: Preterm infants: (Premature infants) Born prior to 38 weeks after conception High risk for illness and death. Average preterm weighs less than 5 ½ pounds Called Low-Birthweight Infants High risk for infection and RDS (Respiratory Distress Syndrome) because of their lungs have not developed completely Presents great difficulty in taking in sufficient levels of oxygen Small-For-Gestational-Age Infants: Due to delayed fetal growth: Weigh 90% of the average weight of infants of the same gestational age Neonates: If the Child does not Pass the Apgar Scale Very-Low-Birthweight Infants: Weigh less than 2 ¼ pounds Been in womb less than 30 weeks Their eyes are fused shut, and earlobes are hardly formed Their skin is darkened red color These infants rarely reach the Age of Viability: Point at which an infant can survive prematurely An infant born earlier than 25 weeks has less than a 50-50 chance of survival. Postmature Infants: Still not born after two weeks after the mother’s due date Blood supply from placenta may become insufficient Blood supply to the brain may be decreased (brain damage) Baby may be too large to make it through the birth canal Neonates: If the Child does not Pass the Apgar Scale Possible consequences of low birthweight: Brain injuries Lung and liver diseases Learning disabilities ADHD Lower levels in reading and math achievement Deficits are evident in adulthood Neonates: If the Child does not Pass the Apgar Scale About 50% of low-birthweight children are enrolled in special education programs. Low birthweight is linked to asthma. Some defects can be improved with: Early speech therapy Intensive enrichment programs Kangaroo care and massage therapy Postpartum Period Lasts about 6 weeks after childbirth when woman adjusts physically and psychologically back to the prepregnant state. Influenced by preceding conditions and experiences Mother learns to care for the baby, feel good about herself and those close to her Physical: hormone changes, weight loss, return to menstruation, loss of energy or fatigue Psychological: feelings of depression, anxiety, coping in new role, excessive worrying Percentage of U.S. Women Who Experience Postpartum Blues and Postpartum Depression Postpartum blues: symptoms appear 2 to 3 days after delivery and subside within 2 to 3 weeks 70% 20% No symptoms 10% Postpartum depression: symptoms linger for weeks or months and interfere with daily functioning