Physical Therapy Skills
advertisement

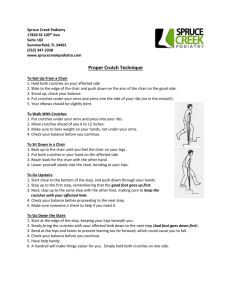
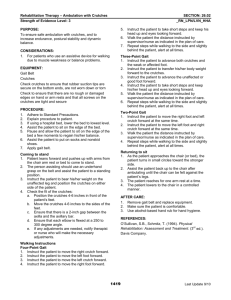
Allied Health Assisting PHYSICAL THERAPY SKILLS Career Highlights Physical Therapy Assistant (PTA) Provide treatment to improve mobility and prevent or limit permanent disability Important members of the health care team Work under supervision of a Physical Therapist Most PTA’s have an associates degree Licensure is required Career Highlights Physical Therapy Assistant (PTA) Job duties include Performing exercises Ultrasound therapy Electrical stimulation treatment Hot, cold, and moist therapy applications Educating patients Career Highlights Physical Therapy Assistant (PTA) Must learn and master the following skills Presenting a professional appearance and attitude Obtaining continuing knowledge Communicating effectively Being sensitive and respecting cultural diversity Learning medical terminology Comprehending anatomy, physiology, pathophysiology Administering CPR and first aid Promoting good nutrition Computer literacy Cleaning and maintaining equipment Ordering and maintaining supplies Performing administrative duties Performing Range-of-Motion (ROM) Exercises Range-of-Motion (ROM) Exercises done to maintain the health of the musculoskeletal system Each joint and muscle in moved through its full range of motion Frequently ordered by the physician for patients with limited ability to move Administered by at physical therapist, nurse, nursing assistant, physical therapy assistant, or other authorized person ROM exercises are done to prevent problems caused by a lack of movement and inactivity such as: Performing Range-of-Motion (ROM) Exercises Contracture: A tightening and shortening of a muscle, resulting in permanent flexing of a joint. Foot drop is a common contracture, but contractures can also affect the knees, hips, elbows, and hands. Performing Range-of-Motion (ROM) Exercises Contracture: Performing Range-of-Motion (ROM) Exercises Muscle and joint function: Circulatory impairment: The circulation of blood is affected, and blood clots and pressure ulcers (bed sores) can develop Mineral loss: Muscles atrophy and become weak. Joints stiffen and become difficult to move Caused by inactivity. Calcium is lost from the bones. Bones become brittle and fractures occur. Increases blood calcium levels, renal calculi develop Other problems: Poor appetite, constipation, urinary infections, respiratory problems, hypostatic pneumonia Performing Range-of-Motion (ROM) Exercises There are four main types of ROM exercises: Active ROM exercises: Performed by patients who are able to move each joint without assistance Strengthens muscles Maintains joint function Helps prevent deformities Performing Range-of-Motion (ROM) Exercises There are four main types of ROM exercises: Active Assistive ROM exercise Patients actively move the joints but they receive assistance to complete the entire ROM At times equipment can be used to help Passive ROM exercises Another person moves each joint for a patient who is not able to exercise Prevents deformities Does NOT strengthen muscles Performing Range-of-Motion (ROM) Exercises There are four main types of ROM exercises: Resistive ROM exercises Administered by a therapist Performed against resistance provided by the therapist Develops strength and endurance The healthcare worker should note if there are any limitations to the exercises before performing ROM exercises In many states and facilities only Physical Therapists or Registered Nurses may perform ROM to the head and neck Performing Range-of-Motion (ROM) Exercises The main terms for movement: Abduction: moving a part away from the midline of the body Adduction: moving a part toward the midline of the body Flexion: bending a body part Extension: straightening a body part Hyperextension: excessive straightening of a body part Rotation: moving a body part around its own axis Circumduction: moving in a circle at a joint Pronation: turning a body part down Supination: turning a body part up Performing Range-of-Motion (ROM) Exercises The main terms for movement: Opposition: touching each of the fingers with the tip of the thumb Inversion: Turning a body part inward Eversion: turning a body part outward Dorsiflexion: bending backward Plantar flexion: bending foot forward Radial deviation: moving toward the thumb side of the hand Ulnar deviation: moving toward the little finger side of the hand Performing Range-of-Motion (ROM) Exercises Principles that must be observed while performing ROM exercises Movements should be slow, smooth, and gentle to prevent injury Support should be provided to the parts above and below the joint being exercised A joint should never be forced beyond its ROM or exercised to the point of pain, resistance, or extreme fatigue If a patient complains of pain, STOP the exercise and report this to your supervisor Watch the patient closely. If you notice a patient is in pain, has SOB, or is diaphoretic, or is pale, STOP and notify supervisor Performing Range-of-Motion (ROM) Exercises Principles that must be observed while performing ROM exercises Each movement should be performed three to five times or as ordered The patient should be encouraged to assist as much as possible Prevent unnecessary exposure of the patient The door or curtain should be closed to provide privacy Use correct body mechanics at all times to prevent injury Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers A transfer (gait) belt is a band of fabric or leather that is positioned around a patient’s waist Used to provide additional support for the patient Provides patient with a sense of security Helps HCW to provide stability Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Important facts to remember: The belt must be the proper size. Must be secure but not too tight Some belts contain loops that are grasped when ambulating the patient. If loops are not present, an underhand grasp should be used The belt should be grasped at the back during ambulation The HCW should walk slightly behind the patient When assisting a person to stand, grasp the belt on both sides The belt should only be applied over clothing. Never on a patient’s skin The use of a gait belt is contraindicated in patients who have an ostomy, gastrostomy tube, abdominal pacemaker, severe cardiac or respiratory disease, fractured ribs, recent chest or abdominal surgery, or pregnancy Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Crutches are artificial supports that assist a patient who needs help walking. Usually prescribed by a physician A therapist or other authorized individual fits them to the patient, and teaches proper use Exercises to strengthen muscles of shoulders, arms, and hands are also frequently prescribed Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Axillary Crutches Made of wood or aluminum Used for a short period of time Bear weight on the hands and not to axillary support Not recommended for weak or elderly patients Require good upper body strength and balance Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Forearm or Lofstrand Crutches Attach to forearms Used for patient with weakness, or paralysis, in both legs Recommended for patients who need crutches for a long time or permanently Requires arms in good condition with good strength Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Forearm or Lofstrand Crutches Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Platform crutches Used for patients who cannot grip handles of other crutches or bear weight on their wrists or hands Do not require as much upper body strength Does require good sense of balance or coordination Patient bears weight on the forearm Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Platform crutches Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Three main types of crutches Platform crutches Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers The following should be observed when fitting crutches to a patient Patient should wear walking shoes that fit well and provide good support Crutches should be positioned 4-6 inches in front of and 2-4 inches to the side of the patient’s foot Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers The following should be observed when fitting crutches to a patient Length of the axillary crutches should be adjusted so that there are 2 inches or 2 to 3 finger widths between the armpit and the axillary bar of the crutch The hand pieces of axillary or forearm crutches should be adjusted so that each elbow is flexed at a 25-30 degree angle Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Common crutch-walking gaits Four-point gait: Used when both legs can bear weight Slow gait Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Common crutch-walking gaits Two-point gait Often taught after four-point gait is mastered Faster gait Usually used when both legs can bear some weight Closest to the natural rhythm of walking Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Common crutch-walking gaits Three-point gait Used only when one leg can bear weight It also can be taught initially Swing-to or Step-to gait More rapid gait Taught after other gaits are mastered Requires upper body and shoulder strength Swing-through or Step-through gait Most rapid gait Requires most strength, balance, and skill Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Cane An assistive device that provides balance and support Several different types of canes Standard Single tipped Curved handles T-handles J-handles Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Cane An assistive device that provides balance and support Several different types of canes Tripod Three tips Quad Cane Four tips Provided widest base of support Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Cane An assistive device that provides balance and support Several different types of canes Walkcane or Hemiwalker Has four legs and a handlebar Good for patients with hemiplegia Bottom of cane tips should be capped with non slip tips Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Cane Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Cane A cane is used on the unaffected (good) side Gives a wider base of support Prevents patient from leaning toward the cane Leg and opposite arm move together Canes must be correctly fitted Bottom tip should be positioned approximately 6-8 inches from the side of the unaffected foot Handle should be level with the top of the femur Elbow should be flexed 25-30 degrees Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Cane Several gaits for can walking can be taught Two point gait Patient moves can and affected leg together Three point gait Patient moves cane Then affected leg Then unaffected leg Therapist determines the correct gait for patient https://www.youtube.com/watch?v=8nvPeXIglI8 Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Walker Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Walker A four legged device that provides support. Several styles Standard Folding Rolling Platform Walkers are used for weak patients who have a poor sense of balance even though no injury may be present To use a walker patients must be strong enough to hold themselves upright while leaning on the walker Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Ambulating Patients Who Use Gait Belts, Crutches, Canes, or Walkers Walker Basic principles for walker use The walker should be fitted to the patient The handle should be level with the top of the femurs Each elbow should be flexed at 25-30 degrees The patient must be taught to lift the walker and place it in front of the body Only placed where the back legs are even with the toes of the patient The patient walks into the walker Administering Heat/Cold Applications Cryotherapy Use of cold for treatment Relieve pain Reduce swelling Reduce body temperature Control bleeding Administering Heat/Cold Applications Cryotherapy Moist Cold Applications are cold and moist against the skin Cold compresses Cold packs Cold soaks More penetrating than dry cold applications Administering Heat/Cold Applications Cryotherapy Dry Cold Cold and dry against the skin Ice bags Ice collars Hypothermia blankets Administering Heat/Cold Applications Cryotherapy Ice bags or collars Special containers filled with ice Most facilities used disposable bags Hypothermia blanket (thermal blanket) Contains coils filled with cool fluid Used to reduce high body temperatures Rectal probe is used to monitor body temperature continuously When temperature reaches certain level blanket decreases circulation of fluid Administering Heat/Cold Applications Thermotherapy The use of heat for treatment Relief of pain Increase drainage from infected area Stimulate healing Increase circulation to certain area Combat infection Relieve muscle spasms Increase muscle motility Administering Heat/Cold Applications Thermotherapy Moist Heat Warm and wet against the skin More penetrating Administering Heat/Cold Applications Thermotherapy Sitz Bath Provides warm, moist heat to the perineal area and rectal area Used postpartum and after rectal surgery Hydrocollator packs Gel filled packs warmed in a water bath 150-170 degrees F Gel maintains warmth for approximately 30-40 minutes Pack can contour to fit smoothly over any area Pack must be covered prior to use Administering Heat/Cold Applications Thermotherapy Dry heat Warm and dry against the skin Warm water bags Heating pads Thermal blankets Aquamatic pads Aquathermia pads Heat lamps Administering Heat/Cold Applications Thermotherapy Warm water bags Special containers filled with warm water Most facilities used disposable bags Thermal blankets Contains coils that can be filled with air or fluid to warm a patient Rectal probe used to monitor patient’s temperature Aquathermia pads Smaller version of thermal blanket that uses fluid Administering Heat/Cold Applications Administering Heat/Cold Applications Administering Heat/Cold Applications Administering Heat/Cold Applications