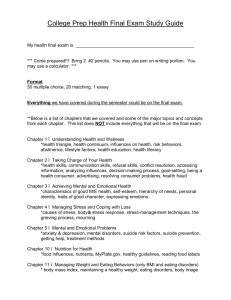
Powerpoint - Florida/Caribbean AIDS Education & Training Center
advertisement

Common Mental Health Issues in Patients with HIV Francisco Fernandez, MD Professor and Chair, USF Health Psychiatry USF Morsani College of Medicine Faculty, Florida/Caribbean AETC Disclosure of Financial Relationships This speaker has no significant financial relationships with commercial entities to disclose. This speaker will discuss off-label use or an investigational product during the program: • Use of stimulants and amantadine in cognitive disorders. This slide set has been peer-reviewed to ensure that there are no conflicts of interest represented in the presentation. Psychiatric Illness in HIV • Mental disorders are highly prevalent in HIV1 infection and AIDS – Dual Diagnosis coexisting substance abuse and psychiatric disorders – Triple Diagnosis coexisting medical illness with substance abuse and psychiatric disorders – HIV-Associated Neurocognitive Disorders (HAND) DEPRESSION Epidemiology of Depression in HIV • • • • Depression is the most common mental health disorder in HIV patients1 36% of adults patients receiving medical care for HIV were depressed in the past 12 months2 Depression is the most common reason for psychiatric referral Rates of depression are highest among injection drug users (IDU) and women engaging in high risk behaviors3 1. Orlando et al., 2002; Komiti et al., 2003 2. HCSUS Bing et al., 2001;Galvan et al., 2002 3. Goodkin et al., 1996 HIV Mood Disorders: Completed Suicide Study Subjects Findings ________________________________________________________ Marzuk 1992 AIDS vs others 36-66 x increase with AIDS Kizer 1992 AIDS vs others 17 x increase with AIDS Cote 1992 72,000 U.S. suicides 7.4 x increase with AIDS Marzuk 1997 HIV+ vs others 2-3 x increase with HIV < suicide risk factors (RFs) Types of Depressive Disorders vs Major Depressive Disorder (MDD) • Psychiatric Differential Diagnoses – Mild depression (or minor depression) – Dysthymia – Bipolar disorder, currently depressed – Adjustment disorder with depressed mood • Medical Differential Diagnoses – Central Nervous System (CNS) HIV cognitive disorders [Minor Cognitive Motor Disorder (MCMD) & HIV-associated dementia (HAD)] – CNS opportunistic illnesses and cancers – Substance abuse – Medication effects – Endocrine abnormalities (hypogonadism, adrenal insufficiency) How to Identify MDD in a Primary Care Setting? • Fewer than 50% of patients with MDD are identified by their primary care providers (PCPs)1 • Two simple questions to ask: 1. During the past two weeks have you felt sad, down or depressed most of the day, nearly every day? 2. During the past two weeks have you been less interested in most things or less able to enjoy the things that you used to enjoy most of the time? 1. Asch et al., 2003 Screening and Diagnostic Tools • Screening: PHQ-2 • Diagnosis: PHQ-9; Depressive disorder module of the SCID or MINI-6 • PHQ-2 and PHQ-9 readily available at no cost • PHQ-9 reliable diagnostic tool. Also provides severity parameters which can help decide the action plan PHQ-2: Patient Health Questionaire-2 Kroenke et al. Med Care 2003; 41(11):1284-92 PHQ-9:Patient Health Questionaire-9 Kroenke et al. J GenIntern Med, 2001;16(9)606-13 SCID: Structured Clinical Interview for DSM Disorders www.cumc.columbia.edu/dept/scid/index.html MINI-6: The Mini-International Neuropyschiatric Interview www.medical-outcomes.com First Line Treatment for MDD • Psychotherapies: “talk therapy” like cognitive behavioral therapy (CBT), interpersonal therapy (IT), psychodynamic therapy, etc. • Medications: antidepressants [selective serotonin reuptake inhibitors (SSRIs), serotonin–norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), others] • Neurostimulation – Electroconvulsive therapy (ECT) – Transcranial Magnetic Stimulation • Combination of psychotherapy and medication Selecting an Antidepressant: Potential for Drug-Drug Interactions Low P450 blockers: Likely to have little impact on metabolism of other drugs Bupropion Citalopram Mirtazapine Venlafaxine Sertraline Potent P450 blockers: Potential for strong impact on metabolism of other drugs Methylphenidate Paroxetine Fluoxetine Fluvoxamine Crewe HK, et al. Br J Clin Pharmacol. 1992;34:262-265. Nemeroff CB, et al. Am J Psychiatry. 1996;153:311-320. von Moltke LL, et al. J Clin Psychopharmacol. 1994;14:1-4. von Motkle LL, et al. Clin Pharmacokinet. 1995;20(suppl 1):33. When to Refer to a Mental Health Specialist • Acute risk of suicide • Psychotic symptoms, signs of dementia or bipolar disorder • Patients with limited or non-response to treatment • PCP level of comfort ANXIETY Prevalence of Anxiety • Anxiety disorders are the most prevalent psychiatric disorders in the general population (Lifetime prevalence 25%)1 • In HIV infected individuals the prevalence rate of anxiety disorders can be as high as 38%2 • Cohen et al. (2001) found that in an urban U.S. HIV clinic anxiety was present in up to 70% of patients 1. Kessler et al., 1994, 2005 2. Elliott, 1998 Anxiety in HIV Patients • Anxiety as a normal response • Anxiety as a disorder – Primary • Adjustment, panic disorder, post-traumatic stress disorder (PTSD), generalized anxiety disorder (GAD), social anxiety disorder (SAD), obsessive compulsive disorder (OCD) – Secondary Anxiety • AIDS-associated illness, other medical illnesses • Anxiety as a side effect – Secondary to medications • like HIV or hepatitis C virus (HCV) treatments (e.g., efavirenz, steroids, isoniazid, interferon) – Secondary to street drugs (stimulants, alcohol, etc) Screening and Diagnostic Tools • Screening: Hospital Depression and Anxiety Scale (HADS); Hamilton Anxiety Scale (HAM-A) • Diagnosis: Specific modules of the SCID or MINI-6; specific disorder scales • Screening questions Treatment Approaches • Overall, very similar to major depressive disorder • Psychotherapies: “talk therapy” like CBT (cognitive behavioral therapy), IT (interpersonal therapy), psychodynamic therapy, support groups, etc. • Medications: antidepressants (SSRIs, SNRIs, TCAs, MAOIs, other), benzodiazepines. – In substance use disorders (SUD) buspirone, antiepileptic drugs [(AEDs) tiagabine, gabapentin] • Combination of psychotherapy and medication SUBSTANCE USE, ABUSE, DEPENDENCE Prevalence of Substance Use Disorders (SUD) in HIV • SUD have a higher prevalence in HIV patients compared to the general population • Bidirectional risk relationship between HIV and SUD1,2,3,4 • Most prevalent: alcohol (EtOH), cocaine, opiates – 25-60% life time prevalence of alcohol abuse or dependence in HIV patients, a 2-4 fold increase compared to the general population 5,6,7,8 – 23-56 % lifetime prevalence of other drug use disorders in HIV subjects, a 4-5 fold increase compared to the general population 5,6,7,8 1. Harvey and Spigner, 1995; 2. Katz et al., 2000; 3. Stall and Purcell, 2000; 4. Wingood and DiClemente, 1998; 5. Rabkin, 1996; 6. Dew et al., 1997; 7. Ferrando et al., 1998; 8. Kessler et al., 1994 Impact of SUD on HIV • In the U.S., SUD is the main driver of HIV transmission [intravenous drugs (IVD) leading] • If untreated can result in poor treatment outcomes • Decreased adherence to combination antiretroviral therapy (CART) • Increased risk taking behaviors • Increased medical and psychiatric comorbidities Recognizing SUD • High suspicion is recommended given high prevalence and bidirectional risk – Should be asked at initial visit and at each follow up • Use screening instruments • Use of urine drug screens (UDS) • Generally more effective to have an open/ nonjudgmental approach when asking patients • “Many persons who are ill may use drugs or alcohol to get through tough times. What have you used to cope with these difficult times?” Treatment Options for SUD • Medical treatment – Detoxification – first step • • • • Opiates methadone, buprenorphine, clonidine Cocaine symptomatic, dopamine (DA) agonists, naltrexone ETOH benzodiazepines, naltrexone Nicotine replacement therapy, bupropion, varenicline – Maintenance: methadone, buprenorphine, DA agonists, naltrexone, disulfiram, topiramate • Topiramate signal across all appetitive drives • Therapeutic Strategies – Motivational enhancement therapy, CBT – 12 Steps facilitation [Alcoholics Anonymous (AA), Narcotics Anonymous (NA)] – Residential treatment HIV Associated Neurocognitive Disorder (HAND) • HIV-neurocognitive impairment continues to be an important problem • HIV-neurocognitive impairment can be easily recognized – Neurodiagnostic tests can improve confidence in the diagnosis and exclude neoplasms and opportunistic infections • HIV-neurocognitive impairment can be treated – Primary therapy antiretroviral therapy (ART) that better distributes into the CNS leads to better outcomes – Secondary anti-inflammatory therapies – Palliative therapies Criteria for HAND Acquired Impairment in ≥ 2 Cognitive Abilities Interferes with Daily Functioning No Preexisting Cause Delirium Absent Asymptomatic Neurocognitive Impairment (ANI) Mild No ● ● Mild Neurocognitive Disorder (MND) Mild Mild ● ● HIV-Associated Dementia (HAD) Marked Marked ● ● Changing Prevalence of HAND • • • • Highly active antiretroviral therapy (HAART) HIV-associated dementia (HAD) Motor neuron disease (MND) Asymptomatic neurocognitive impairment (ANI) Modified from Heaton R., et al: HIV-associated neurocognitive disorders (HAND) persist in the era of potent antiretroviral therapy: The CHARTER Study; and Heaton R., J Int Neuropsychol Soc. May 1995;1(3):231-251. Screening for HAND by Self Report Medical Outcomes Study (MOS) HIV Cognitive Functional Status Scale 1. Difficulty reasoning and solving problems? 2. Forget things that happened recently? 3. Trouble keeping your attention on any activity for long? 4. Difficulty doing activities involving concentration and thinking? Validated against neuropsychological (NP) overall performance Knippels, Goodkin, Weiss, et al., AIDS, 2002;16:259-267 Pharmacotherapy of HAND • Primary Treatments – Antiretroviral medications • Secondary Treatments – Immunostimulants and inflammatory mediators • Palliative Treatments – Psychotropic agents – Nutritional Neuro-AIDS Can Be Treated Higher CNS PenetrationEffectiveness (CPE) Scores and Lower Viral Loads in Cerebrospinal Fluid (CSF) Letendre et al, Archives of Neurology, 2008 Antiretroviral Effectiveness CNS Penetration-Effectiveness Score Nucleoside Reverse Transcriptase Inhibitors (NRTIs) Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) Protease Inhibitors (PIs) Fusion Inhibitors Good Fair Poor 1 0.5 0 Abacavir Zidovudine Emtricitabine Lamivudine Stavudine Delavirdine Nevirapine Efavirenz Indinavir Indinavir-r Lopinavir-r Amprenavir-r Atazanavir Atazanavir-r Darunavir-r Didanosine Tenofovir Zalcitabine Amprenavir Nelfinavir Ritonavir Saquinavir Saquinavir-r Tipranavir-r Enfuvirtide LeTendre S., et al, Arch Neurol., 2007 From JC McArthur, MBBS, MPH, at 13th Annual Ryan White HIV/AIDS Program Clinical Conference, IAS–USA. Relevance of ART, CNS Penetrance & HAND • Despite HAART’s effect on incidence, prevalence of HAND remains high, and pathological evidence of CNS infection persists (Heaton R., Neurology, 2010; Vago L., AIDS, 2002) • HAART can reverse neurocognitive deficits, but at best, it is usually only partial – ? Functional performance change (Tozzi V., AIDS, 2002) • Long term aviremic HIV+ individuals have high rate of HAND MND (Simioni P., AIDS 2009) How Best To Treat HAND in 2012 • Primary therapy suppress HIV RNA viral load systemically and in CSF • Consider secondary pharmacotherapy • Control all controllables – – – – Anxiety and depression, drug and alcohol use Co-infections (HCV) Medication side-effects Lab indices (anemia, thyroid, B12, glucose, cholesterol) • Trial of dopamine agonists – Stimulants – Amantadine Summary • Depression, anxiety, SUD, HAND, and HIV are highly comorbid – Once they combine, there is synergy in the overall effect on the affected individuals and their treatments – Careful medical and neurobehavioral evaluation is required to rule out primary treatable CNS disease and comorbid psychiatric disorders – Effective treatment strategies are available for the primary and secondary HIV manifestations • The neuropsychiatric complications of the disease deserve the same aggressive approach as that of the systemic aspects of the disease DANIEL A Neuropsychiatric Case Study Daniel • Daniel is a 52-year-old man, HIV+ since 1996. He remains asymptomatic. He also has hepatitis C. • 1996: CD4=212, viral load (VL)=182,000 • 1997: HAART – undetectable VL; CD4 ~ 600's. • Drug holiday – 2004-06, resumed treatment 2007 • Current Meds: darunavir, etravirine, emtricitabine/tenofovir, ritonavir • High-level job, he is meticulous and dresses impeccably • He is a “weekend warrior” – Uses ecstasy and alcohol. • For the last 9 months low energy and some memory difficulties • He thought this was stress-related; however, a vacation did not help Daniel – What is your presumptive diagnosis? • • • • • Adjustment disorder ART resistance Substance abuse Cirrhosis Depression What would you like to do next? A. Cognitive assessment B. Complete blood count (CBC), comprehensive metabolic panel (CMP), syphilis serology, CD4, viral load C. Endocrine screen D. CT-brain and/or MRI E. All of the above 100% A. 0% 0% B. C. 0% 0% D. E. Daniel – Clinical & Lab Findings • h/o recurrent depressive illness • h/o relapsing alcoholism and ecstasy abuse • Liver enzymes and thyroid labs – within normal limits (wnl) • VL and CD4 - no changes • CT Scan - wnl • Testosterone – 120 ng/dl What next? A. Initiate low dose citalopram B. Hormone replacement therapy (HRT) C. PRN lorazepam D. End of life Counseling E. All of the above 100% 0% A. 0% B. C. 0% 0% D. E. Daniel – Recommendations • Treat alcohol / ecstasy abuse • HRT – No improvement with testosterone replacement in 4 to 6 weeks • Start formal psychotropic agent – Which would you choose? Which psychotropic agent would you choose? A. Citalopram (Celexa®) B. Quetiapine (Seroquel®) C. Venlafaxine (Effexor XR®) D. Bupropion (Wellbutrin XL®) E. Topiramate (Topamax®) 0% A. 0% 0% B. C. 0% 0% D. E. Daniel – follow up • Daniel stops alcohol and ecstasy use temporarily • Testosterone replacement continues • Venlafaxine 150 mg/day • Initially his energy, memory and concentration improve • Complains of feeling depressed, hopeless, anhedonic, isolates himself, poor appetite, mild suicidal thoughts, interrupted sleep What is your diagnosis now? A. Adjustment disorder with depressed mood B. Substance-induced mood disorder C. Major depression – recurrent D. Bipolar depression E. Acute stress reaction/disorder 100% 0% A. 0% B. C. 0% 0% D. E. Daniel – MDD recurrent • SNRI (liver protection, low drug-drug interaction potential with ARVs, low CNS side effects) – Increase venlafaxine to 300 mg/daily – Daniel’s depression improves, but memory and concentration do not What are his other diagnoses? A. Residual depression B. Relapse on alcohol and ecstasy C. Minor cognitivemotor disorder D. Acute stress disorder E. Neurotoxicity 100% 0% A. 0% B. C. 0% 0% D. E. Daniel – 2 months later … • Daniel shows very late to his appointment – unusual for him • He looks unkempt • Seems distracted What do we need to rule out? A. Residual depression B. Relapse on alcohol and ecstasy C. HIV-Associated Dementia D. Progression to AIDS E. Neurotoxicity 100% 0% A. 0% B. C. 0% 0% D. E. Daniel 2 months later … • • • • • Alcohol? None Ecstasy? None Depression? No Testosterone? Normal Liver Function Tests (LFTs), Thyroid and HIV Labs – no changes Now what? A. Neuroimaging B. Lumbar puncture C. Neuropsychological testing D. Psychiatric consultation E. All of the above 100% 0% A. 0% B. C. 0% 0% D. E. Daniel – other considerations • • • • • • Is Daniel taking other medications? Other drugs? Over the counter pills or vitamins? Any new events? None of these are present? Now what? Daniel – Work up results … • Lumbar Puncture? Mild pleocytosis and elevated protein. • Neuro consult “minor cognitive abnormalities without any focal neurological findings besides mild neuropathy." • Psychiatry “no residual depression, no active substance use, Mini-Mental State Exam (MMSE) 25/30, slowing of information processing” • Neuropsychological evaluation – attention and working memory deficits. Slow motor activity and thinking processes. • MRI – reported as normal • What does this mean? Diagnoses? Daniel – Concluding • Daniel, besides – Hepatitis C, HIV, Hypogonadism – Recurrent Major Depression, Alcohol/ecstasy • MCMD vs HAD • Anything else we need to address? – Adherence – Medication List – Psychosocial • Prognosis? • What is your personal reaction as Daniel’s provider? Daniel - Treatment • • • • • • • ARV that cross the Blood Brain Barrier Avoid alcohol, drugs, sedating meds Stimulants vs DA-agonists Environmental Interventions Rehabilitation Family, work, friends Support groups, education Questions Gracias! • Francisco Fernandez, M.D. • ffernand@health.usf.edu • (813) 974-1437