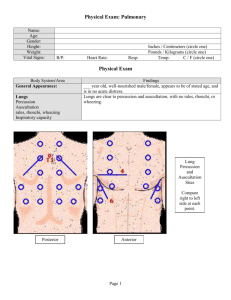
PHYSICAL ASSESSMENT: HEAD TO • TOE Physical assessment • Is a process by which a nurse obtains a data that describes a client’s changing health status and • • person’s responses to actual or potential health problems which is analyzed to form pertinent • diagnosis. Is a head-to-toe review of each body system that offers objective information about the client and allows the nurse to make clinical judgment. Importance of physical assessment • • • To early detect and treat diseases and disorders. To identify actual and potential health problems. To establish a data based from To make clinical judgments about a • management. To evaluate the physiological outcome of care. To obtain and gather data about the client’s health basis of data for future assessment. An excellent way to evaluate an individual’s current health status. Four basic techniques in physical assessment 1. Inspection ➢ It is the use of one’s senses of vision and smell to consciously observe the patient. ➢ It is also known as concentrated watching. ➢ It is a close, careful scrutiny; first of the individual as a whole and then of each body system. which the subsequent phases of • • • the nursing evolve. To assess the client’s impact of 2. Palpation activity and exercise on the client’s overall level of health. To assess the client’s routine exercise pattern and observe ➢ It is the act of touching a patient in a therapeutic manner to elicit specific information. ➢ It follows and often confirms how the client’s body system points you noted during inspection. response to activity and exercise. To establish the client-nurse Palpation applies your sense of relationship. • • To obtain information about the client’s health including, physiologic, psychological, sociocultural, cognitive, developmental and spiritual aspects. To identify the client’s strength and weaknesses. Purpose of physical assessment • To supplement, confirm or refute data obtained in the nursing history. • To confirm and identify nursing diagnosis. touch to assess these factors o Texture o o Temperature Moisture o o Organ location and size Any swelling, vibration or o pulsation Rigidity or spasticity o o o Crepitation Presence of lumps or masses Presence of tenderness or pain. Two distinct types of palpation a. Light palpation ➢ it is superficial, delicate ❖ The striking hand directly and gentle. contacts the body wall. This ➢ finger pads are used to gain information of the patient’s skin surface to a depth of approximately ½ - 1 inch below the surface. ➢ reveals information on skin produces a sound and is used in percussing the infant’s thorax or the adult’s sinus areas. II. Mediate or Indirect Percussion ❖ It is used more often and involves both hands. The texture and moisture; overt striking hand contacts the large or superficial masses; and fluid, muscle guarding and superficial tenderness. b. Deep palpation III. ➢ it can reveal information stationary hand fixed on the person’s skin. This yields a sound and a subtle vibration. Direct Fist Percussion ❖ It is used to assess the about the position of organs and masses, as well presence of tenderness in internal organs, such as the as their size, shape, mobility, consistency, and areas of discomfort. ➢ uses the hands to explore liver or the kidneys. The presence of pain in conjunction with direct fist percussion indicated inflammation of that the body’s internal structure to a depth of 1 to organ or a strike of too high in intensity. 2 inches or more. ➢ most often used for the abdominal and male and female reproductive assessments. IV. Indirect Fist Percussion ❖ Its purpose is the same as direct fist percussion. In fact, the indirect method is preferred over the direct method. It is because in this methods, the non dominant hand absorbs some of the force of the striking hand. The resulting intensity should be sufficient force to produce 3. Percussion ➢ It is the technique of striking or tapping the person’s skin with short, sharp strokes to assess underlying structures. ➢ The strokes yield a palpable vibration and a characteristic sound that depicts the location, size and density of the underlying organ. pain in the patient if organ inflammation is present. Percussion elicits five types of sounds I. II. ➢ These sounds also are diagnostic of normal and abnormal findings. ➢ The thorax and abdomen are the most frequently percussed location. Four types of percussion techniques I. Immediate or Direct Percussion Flatness (dull) – bone and muscle Dullness (thud-like) – liver, spleen, heart III. IV. V. Resonance (hollow) – air-filled lung / normal lung Hyperresonance – emphysematous lung Tympany – stomach filled with gas (air) 4. Auscultation ▪ Introduce yourself to the patient. ➢ It is the act of active listening to Enlist the patient’s cooperation by the body organs to gather information on patient’s clinical status. ➢ includes listening to sounds that are voluntarily and involuntarily produced by the body such as the explaining what you are about to do, where it will be done, and how it may feel. Explain to the patient why you may be spending a long time performing one particular skill. heart and blood vessels and the lungs and abdomen. ➢ Auscultated sounds should be analyzed in relation to their relative intensity, pitch, duration, quality, and location. Two types of auscultation a. Direct or Immediate auscultation ➢ It is the process of listening ▪ ▪ Do medical hand washing . ▪ Position the patient as dictated by the body system being assessed. Warm all instruments prior to their use. ▪ DURING ▪ Conduct the assessment in a ▪ systematic fashion every time. While performing each step in the with the unaided ear. This can physical assessment process, you include listening to the patient from some distance away or placing the ear directly on the may need to inform the patient of what to expect, where to expect it, and how it should feel. patient’s skin surface. And example is the wheezing that is audible to the unassisted ear in a person having a severe asthmatic attack. b. Indirect or Mediate auscultation ➢ It is the use of stethoscope, ▪ Avoid making crude or negative remarks, be cognizant of your facial expression when dealing with malodorous and dirty patients or with disturbing findings. ▪ Proceed from the least invasive to the most invasive procedure for which transmits the sounds to the nurse’s ear. each body system. ▪ Nursing responsibilities BEFORE ▪ Always dress in clean professional manner, make sure you have your name pin or workplace ▪ identification. Remove all bracelets, necklaces, or earrings that can interfere during the physical assessment. ▪ Be sure your hair will not fall forward and obstruct your vision or touch to the patient. ▪ Ensure that all necessary equipment is ready for use and within reach. If the patient complains of fatigue, continue the assessment later. AFTER ▪ ▪ Provide recognition to the patient when the physical assessment concluded; inform the patient what will happen next. Place patient in a comfortable position. ▪ Do after care. ▪ ▪ Do medical hand washing. Document assessment findings in the appropriate section of the patient record. Materials and Instruments of Physical Treatment To depress the tongue during assessment of the mouth and 1. Flashlight or penlight - To assist in viewing of the pharynx and cervix or to determine the reaction of the pupils of the eye. 2. Laryngeal or dental mirror - To observe the pharynx and oral cavity 3. Nasal septum - - To permit visualization of the lower and middle turbinates; usually a penlight is used for illumination. 4. Ophthalmoscope - A lighted instrument to visualize the interior of the eye 5. Otoscope - A lighted instrument to visualize the eardrum and external auditory canal (a nasal speculum may be attached to the Otoscope to inspect nasal cavities). 6. Percussion (reflex) hammer - An instrument with a rubber head to test reflexes 7. Tuning Fork - A two-prolonged metal instrument used to test hearing acuity and vibratory sense. 8. Cotton applicators - To obtain specimens. 9. Gloves - To protect the nurse 10. Lubricant - to ease the insertion of instruments (ex.Vaginal Speculum) 11. Tongue blades (depressors) pharynx Various positioning of the patient ❖ Dorsal recumbent Back-lying position with knees flexed and hips externally rotated; small pillow under the head; soles of feet on the surface. Supine (horizontal recumbent) Back-lying position with legs extended; with or without pillow under the head. ❖ Sitting A seated position. The back is unsupported and legs hanging freely. ❖ Lithotomy Back-lying position with feet supported in stirrups; the hips should be in line with the edge of the table. ❖ Sims Side-lying position with the lowermost leg flexed at the hip and knee, upper arm flexed at the shoulder and elbow. ❖ Prone Lies on the abdomen with head turned to the side, with or without a small pillow. Various positioning of the patient