in10520G - Sage Products LLC
advertisement

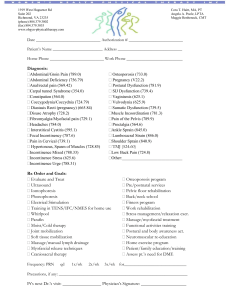
Comfort ® Shield An Innovative Approach to Incontinence Care Risk Factors for Pressure Ulcer Development • • • • • • • Impaired Mobility Fecal Incontinence Malnutrition Decreased Mental Status Peripheral Vascular Disease Urinary Incontinence Diabetes Maklebust J, Magnan MA, Adv Wound Care. Nov 1994;7(6):25, 27-8, 31-4 passim. 87.0% 56.7% 54.4% 50.7% 28.1% 27.0% 23.7% Risk Factors for Pressure Ulcer Development “…The odds of having a pressure ulcer were 22 times greater for hospitalized adult patients with fecal incontinence compared to hospitalized patients without fecal incontinence…and 37.5 times greater in patients who had both impaired mobility and fecal incontinence” JoAnn Maklebust, MSN, RN, CS, NP and Morris A. Magnan, MSN, RN, “Risk Factors Associated with Having a Pressure Ulcer: A Secondary Data Analysis”, Advances in Wound Care, November 1994 Facts About Pressure Ulcers • 80% of pressure ulcers in hospital are Stage I or Stage II.1 • Almost half of all pressure ulcers form on the sacrum (36.9%) and ischium (8.0%).2 • A healthcare facility will spend between $400K and $700K annually on pressure ulcer treatment.3 • JCAHO lists prevention of health care associated pressure ulcers as a patient safety goal.4 • Over a boney prominence.5 1. Whittington KT, Briones R, “National Prevalence and Incidence Study: 6-Year Sequential Acute Care Data,” Adv Skin Wound Care. 2004 Nov/Dec;17(9):490-4. 2. Amlung SR, Miller WL, Bosley LM, Adv. Skin Wound Care. 2001 Nov/Dec; 14(6): 297-301. 3. Robinson, C; Gioekner, M; Bush, S; Copas, J; et al. Determining the efficacy of a pressure ulcer prevention program by collecting prevalence and incidence data: a unit-based effort. Ostomy Wound Manage. 2003. May: 49(5):44-6. 48-51. 4. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/07_ltc_npsgs.htm. 5. Joan Junkin, MSN, RN, CWOCN, BryanLGH Medical Center Searching for an Appropriate Name: Incontinence Associated Dermatitis • Acknowledges that condition extends beyond perineal skin. • Clearly identifies UI or FI as primary causative factor. • Removes negative and unfair association with diapers. • Broad enough to encompass secondary infections such as candidiasis. • Usually well beyond boney prominence http://www.sageproducts.com/education/shArticles.asp Gray M, Lerner-Selekof J, Junkin J, A Closer look at Perineal skin injury associated with incontinence in acute care facilities. A CE symposium in conjunction with the 2006 WOCN conference, Minnieapolis, MN June 2006 May/June 2007 Multi-Site Prevalence Study- Bryan LGH; University of Maryland1 • 608 patients surveyed • 120 patients incontinent • 42.5% Perineal skin injury • 20.0% had IAD • 21.7% had pressure sores Lerner-Selekof J, Junkin J, Prevalence of Incontinence and Associated Skin Injury in the Acute Care Patient, JWOCN, May/June 2007 The Nix Study HIGHLIGHTS “Use of Skin Protectants is Lacking in Protocols and Application” • The goal was to determine if facility has protocol in place for skin protectant application & the frequency of compliance to that protocol. • 76 hospitals & LTC facilities were involved. • While 75% of protocols include the use of a skin protectant, but the actual USAGE of those skin protectants is severely lacking. • Only 10 cents per patient per day is being spent on skin protectants (barrier creams/ointments). Nix, D., Ermer-Seltun, J, Ost/wound Mgmt. Dec 2004;50 (12):59-67 The Lyder Study HIGHLIGHTS “A review of Perineal Skin Care Protocols and Skin Barrier Product Use.” • The goal was to put in place a 3-pronged prevention program to decrease pressure ulcers. • The changes made were with pressure reduction, nutrition, and skin care protectants. • Compliance to the changes was well managed & enforced. • They monitored 136 residents at 2 LTC facilities over a 5-month period. • Overall, they saw 87% and 76% reduction in their pressure ulcer incidence rates. • The average cost for skin care products was about $5 per patient per day. Lyder CH, Shannon R, Empleo-Frazier O, McGeHee D, White C, Ostomy/Wound Management. Apr 2002;48(4):52-62. Clever et al. - Pressure Ulcer Study “Evaluating the Efficacy of a Uniquely Delivered Skin Protectant and Its Effect on the Formation of Sacral/Buttock Pressure Ulcers”* Average Monthly Incidence of Sacral/Buttock Pressure Ulcers Old standard of care vs. using Comfort Shield® as preventative in new standard of care 4.7% 0.5% Old Standard of Care New Standard of Care 7/00 – 3/01 5/01 – 7/01 Reduction in Incidence Of sacral/buttock pressure ulcers 2/02 – 4/02 *Comfort Shield® was used on all incontinent patients and was the only variable changed from the control period. Clever K, Smith G, Bowser C, Monroe K Long-Term Care Unit, Fulton County Medical Center, McConnellsburg, PA, Ostomy/Wound Management. Dec 2002;48(12):60-7. Donna Driver MS, CWOCN Peer-reviewed clinical study published in Critical Care Nurse August 2007 Two Phase Study Phase 1 Multi-step process Phase 2 All in one product Consistency is the Key for Treating Severe Perineal Dermatitis Due to Incontinence Sluser S, Sturgeon Community Hospital and Health Centre. Poster presented at the Clinical Symposium on Advances in Skin and Wound Care, Las Vegas, NV. Oct 2005. “The Development of Cost-Effective Quality Care for the Patient with Incontinence” • Group A = Cleansing spray, washcloths, skin barrier (multi- step process and the current practice). • Group B = Shield Barrier Cloths. • Group C = Disposable washcloth without dimethicone. Results: • Group A = $6.13 per patient per day; 10% skin breakdown. • Group B = $5.40 per patient per day; 8% skin breakdown. • Group C = Discontinued in week 4 due to 29% skin breakdown. • 2003 72 consults due to IAD and 2004 10 consults due to IAD. http://www.sageproducts.com/education/shSymposiaPres.asp Dieter L, Drolshagen C, Blum K, Cost-effective, quality care for the patient with incontinence. Research Poster Abstract presented at WOCN , Minneapolis, MN June 2006 “An Economic Evaluation of Four Skin Damage Prevention Regimens in Nursing Home Residents with Incontinence” By Donna Bliss, Cindy Zehrer, Kay Savik, Graham Smith and Edwin Hedblom Key Economic Findings: Total Average Costs (Per episode – when barrier and cleanser applied every time): $1.17* Average Cost for Shield Per episode – (all in one barrier and cleanser applied every time): $.90** *Excludes average per episode supply cost of $.53 for gloves, 2 disposable wipes, 2 cloth washcloths, 1 absorbent pad, 1 brief, 1 underpad **Based on 3 cloths per episode, $.30 per cloth - Nix Average Labor Costs (Per episode – when barrier and cleanser applied every time): $.64 Barrier Average (Per episode – applied every time): $0.23 Skin Care Product Costs Average (Per episode – applied every time): $.30 Journal of Wound, Ostomy & Continence Nursing. 34(2):143-152, March/April 2007. Bliss, Donna Z.; Zehrer, Cindy; Savik, Kay; Smith, Graham; Hedblom, Edwin IHI Protecting 5 Million Lives From Harm Getting Started Kit: Prevent Pressure Ulcers How-to-Guide http://www.ihi.org/ihi Six Essential Elements of Pressure Ulcer Prevention 1. 2. 3. 4. 5. 6. Admission Assessment Reassess Daily Inspect Skin Daily Manage Moisture Optimize Nutrition and Hydration Minimize Pressure http://www.ihi.org/IHI/Programs/Campaign/ 4. Manage Moisture: Keep the Patient Dry and Moisturize Skin “By combining routine activities in a protocol such as a “pressure ulcer prevention protocol,” staff can complete multiple tasks while in the room every two hours and document them all at once.” • Provide supplies at the bedside of each at-risk patient who is incontinent. This provides the staff with the supplies that they need to immediately clean, dry, and protect the patient’s skin after each episode of incontinence. • Provide under-pads that pull the moisture away from the skin, and limit the use of disposable briefs or containment garments if at all possible. • Provide pre-moistened, disposable barrier wipes to help cleanse, moisturize, deodorize, and protect patients from perineal dermatitis due to incontinence. http://www.ihi.org/IHI/Programs/Campaign/ “Location, location, location: Getting your incontinence care process bedside Yields reduction in skin injury”- Tory Schmitz, RN,MSN CCRN, CNAA-BC The Methodist Hospital, Houston TX • Used both Comfort Bath® and Shield Barrier Cloths • Placed product at patient bedside • Compliance to appropriate incontinence care increased from 76% to 97% • IAD prevalence dropped from 15% to 0 “Location, location, location: Getting your incontinence care process bedside Yields reduction in skin injury”- Tory Schmitz, RN,MSN CCRN, CNAA-BC The Methodist Hospital, Houston TX “Save our skin: Initiative cuts pressure ulcer incidence in half” • OSF St Francis – 710 beds, Level 1 Trauma, Magnet, 25,000 admits. • SOS Program: OR Skin Assessment; new skin prevention protocol-Shield Barrier Cloths. • 9/2001 9.4% baseline incidence rate of PS’s. • 12/2005 1.8% incidence rate. • “Premoistened, disposable barrier wipes…..” http://www.sageproducts.com/education/shArticles.asp Courtney BA, Ruppman JB, Cooper HM, Save our skin: Initiative cuts pressure ulcer incidence in half. Nursing Management. Apr 2006;37(4):36-45 New CMS Guidelines: If It’s Not POA, We Won’t Pay Conditions No Longer Covered: 1. Pressure Ulcers 2. Vascular and Urinary Tract Infections from Catheters 3. Mediastinitis (a SSI from heart surgery) 4. Falls 5. “Never Events” – Objects left in body during surgery – Air embolisms – Blood incompatibility Federal Register, Vol 72, No.162, August 8, 2007 What you NEED to Know: • • • • MANDATORY POA Tracking: 10/1/07 Non-Payment: 10/1/2008 What’s “POA?” 48 Hours According to CMS, what percent of Pressure Ulcers are avoidable? 100%! If POA, Stage III and IV pressure ulcers receive payment Stage I or II pressure ulcers will not receive payment even if they progress to a Stage III or IV Federal Register, Vol 72, No.162, August 8, 2007 “An Economic Evaluation of Four Skin Damage Prevention Regimens in Nursing Home Residents with Incontinence” By Donna Bliss, Cindy Zehrer, Kay Savik, Graham Smith and Edwin Hedblom Key Economic Findings: Total Average Costs (Per episode – when barrier and cleanser applied every time): $1.17* Barrier Average episode – applied every Average Cost for(Per Shield Per episode – when time): $0.23 barrier and cleanser applied every time): $.90**Average (Per Skin Care Product Costs *Excludes average per episode supply cost of $.53 for gloves, 2 disposable episode – applied every time): $.30 wipes, 2 cloth washcloths, 1 absorbent pad, 1 brief, 1 underpad **Based on 3 cloths per episode, $.30 per cloth - Nix Average Labor Costs (Per episode – when barrier and cleanser applied every time): $.64 http://www.ncbi.nlm.nih.gov/sites/entrez Provide the Supplies at the Bedside Why Comfort Shield Barrier Cloths? 1. One-step process. 2. Eliminates process variation between caregivers. 3. Reduces the impact of one of the major risk factors associated with pressure ulcer development which is incontinence. 4. Evidence-based clinical outcomes. 5. Less IAD consults 6. Cost effective: Comfort Shield average cost per day per patient = .29 per cloth x 9 washcloths = $2.64 / vs. traditional incontinence care products at $5.19 per day. INCONTINENT OINTMENTS & BARRIERS 45% 40% Annual 2011 Market 35% 30% 25% 20% 15% 10% 5% 0% 42.4% 17.6% 15.8% 8.6% * others include: Healthpoint, 3M, Fougera, Derma Sciences, etc. 5.3% 3.3% <2% each Source: GHX Trend Report (Dollars) 2nd Quarter, 2011 Hospital; Annual market represents last 4 quarters of data ALL-IN-ONE PREPACKAGED INCONTINENCE OINTMENTS & BARRIERS Annual 2011 Market 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 92.6% 7.4% Source: GHX Trend Report (Dollars) 2nd Quarter, 2011 Hospital; Annual market represents last 4 quarters of data Market Review - Shield Shield Sales* $28.5 M Current Market Capture: 25% Potential Shield Market $113 M Market Available: 75% *Source: Inpatient admissions and LOS for US and Canada per 2006 HCUP Nationwide Inpatient Sample (NIS) and 2006 Canadian Institute for Health Information (CIHI). Rates calculated on assumption of 20% of inpatient incontinence (Junkin) with 3 episodes per day, 3 cloths @ $.31 per cloth. Shield sales figures: Sage Sales from September 2007 – August 2008 Who is Focused on Skin Breakdown? CMS State Operations Manual, F314 “At least daily, staff should remain alert to potential changes in the skin condition and should evaluate and document identified changes. For example, a resident’s complaint about pain or burning at a site where there has been pressure or a nursing assistant’s observation during the resident’s bath that there is a change in skin condition should be reported so that the resident may be evaluated further.” Centers for Medicare & Medicaid Svcs, CMS Manual System, Pub. 100-07 State Operations, Provider Certification, Appendix PP Guidance to Surveyors for LTC Facilities, F314 §483.25(c) Pressure Sores, Monitoring (Rev. 4, Issued/Effective 11-12-2004). Dept of Health & Human Svcs, Transmittal 12, 14 Oct 2005:145 (available at new.cms.hhs.gov/transmittals/downloads/R12SOM.pdf). Who is Focused on Skin Breakdown? CMS State Operations Manual, F315 “One key to preventing skin breakdown is to keep the perineal skin clean and dry. Research has shown that a soap and water regimen alone may be less effective in preventing skin breakdown compared with moisture barriers and no-rinse incontinence cleansers.” Centers for Medicare & Medicaid Svcs, CMS Manual System, Pub. 100-07 State Operations, Provider Certification, Appendix PP Guidance to Surveyors for LTC Facilities, F314 §483.25(c) Pressure Sores (Rev. 4, Issued/Effective 11-12-04) and F315 483.25(d) Urinary Incontinence, Skin-Related Complications (Rev.8, Issued/Effective 06-28-05). Dept of Health & Human Svcs, Transmittal 12, 14 Oct 2005:131,180 (available at new.cms.hhs.gov/transmittals/downloads/R12SOM.pdf). Comfort Shield® Barrier Cloths Replace Thank You For Your Time