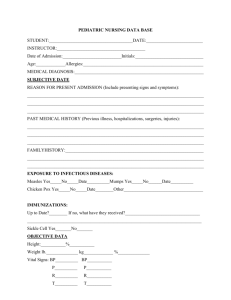
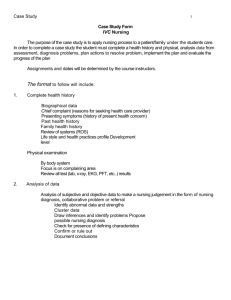
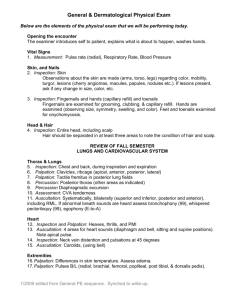
H.-Assessment
advertisement

Nursing Health Assessment Akram Mohammad AbuSalah BNS, MSN, Ph. D. Islamic University of Gaza Strip 1 Chapter (1) The Interview Islamic University of Gaza Strip The first assessment begin in (1992) by American medical association In (1995) health assessment considered as basic human right Preventive health care divided in three categories, primary, secondary and tertiary prevention. Each level of prevention is based on a thorough assessment of the client's health as status. Periodic health assessment needed to be performed by a physician, or a nurse 3 Objectives of health assessment Surveillance of health status, identification of occult disease, screening, and follow-up care The periodic assessment, at regular intervals Increasing client participation in health care Accurately define the health and risk care needs for individuals Health assessment is shared with the client in a clearly and understandable manner The client must share in decision making for his own care. 4 Types of Assessment Comprehensive assessment: is usually the initial assessment it very thorough and includes detailed health history and physical examination and examine the client's overall health status Focused assessment : is problem oriented and may be the initial assessment or an ongoing assessment 5 Frequency of assessment The persons under (35) years every (4 – 5) years The persons from (35 – 45) every (2 – 3) years. Persons from (45-55) years of age undergo a thorough health assessment every year. Persons over (55) years may needs assessment every 6 months or less 6 Importance of nursing health assessment F 1. Systematic and continuous collection of client data 2. It focus on client responses to health problems 3. The nurse carefully examine the client’s body parts to determine any abnormalities 4. The nurse relies on data from different sources which can indicate significant clinical problems 5. Health assessment provides a base line used to plan the clients care 7 6. Health assessment helps the nurse to diagnose client’s problem & the intervention 7. Complete health assessment involves a more detailed review of client’s condition 8. Health assessment influence the choice of therapies & client's responses 8 Purposes of health assessment 1. Gather data 2. Confirm or refuse data obtained in the health history 3.To identify nursing diagnoses 4. To make clinical judgments about client's changing health status 5.To evaluate bio-psycho-social and spiritual outcomes of care 9 Nursing and medical diagnosis There is a big Difference between both because: Nursing diagnose is independent role of the nurse Nursing diagnoses depends on the client's problems/response associated with specific disorder Any problem in nursing diagnosis must notice from a holistic view e.g. bio-psycho-social and spiritual relations 10 Medical diagnoses Depends on clinical picture and laboratory findings The specialist doctor has a right to diagnose not else Example: - DM is medical diagnoses (hypo or hyperglycemia) - Nursing diagnoses in this case e.g. Impaired skin integrity R/T poor circulation, Knowledge deficit about the effects of exercise on needs of insulin. The difference between medical diagnosis, a collaborative problem, and nursing diagnosis is explained with the next table:11 12 Health Assessment Holistic approach: 1. The interview 2. Psychosocial assessment 3. Nutritional assessment 4. Assessment of sleep-wakefulness patterns 5. The health history. 13 1. Interview Definition: communication process focuses on the client's development of psychological, physiological, sociocultural, and spiritual responses, that can be treated with nursing & collaborative interventions 14 Major purpose: To obtain health history and to elicit symptoms and the time course of their development. The interview conducted before physical examination is done. Components of nursing interview 1. Introductory phase 2. Working phase 3. Termination phase 15 1. Introductory phase: Introduce yourself and explains the purpose of the interview to the client. Before asking questions, Let client to feel Comfort, Privacy and Confidentiality 16 Working phase: The nurse must listen and observe cues in addition to using critical thinking skills to validate information received from the client. The nurse identify client's problems and goals. Termination phase: 1.The nurse summarizes information obtained during the working phase 2.Validates problems and goals with the client. 3.Making plans to resolve the problems (nursing diagnosis and collaborative problems are identified and discussed with the client) 17 Communications techniques during interview 1. Types of questions : Begin with open ended questions to assess client's feelings e.g. what, how, which“ Use closed ended question to obtain facts e.g." when, did…etc Use list to obtain specific answers e.g. "is pain sever, dull sharp Explore all data that deviate from normal e.g. “increase or decrease the problem 18 2. Types of statements to be use: Repeat your perception of client's response to clarify information and encourage verbalization 3. Accept the client silence to recognize thoughts 4. Avoid some communication styles e.g. Excessive or not enough eye contact. Doing other things during getting history. Biased or leading questions e.g. "you don't feel bad" Relying on memory to recall information 19 5. Specific age variations : Pediatric clients: validate information from parents. Geriatric clients: use simple words and assess hearing acuity 6. Emotional variations: Be calm with angry clients and simply with anxious and express interest with depressed client Sensitive issues "e.g. sexuality, dying, spirituality" you must be aware of your own thought regarding these things. 20 7. Cultural variations: Be aware of possible cultural variations in the communication styles of self and clients 8. Use culture broker: Use culture broker as middleman if your client not speak your language. Use pictures for non reading clients. 21 Chapter (2) Psychosocial assessment Islamic University of Gaza Strip Psychosocial assessment Psychological assessment involves person's growth and development throughout his life. Discuss crises with the clients to assess relationship between health & illness. “It depends on multiple G&D theories e.g. Erickson, Piaget, and Freud …. etc. 23 Stages of Age Infancy period: birth to 12 months Neonatal Stage: birth-28 days Infancy Stage: 1-12 months Early childhood Stage: It’s refers to two integrated stages of development Toddler: 1 - 3years. Preschool: 3 - 6 years. Middle childhood 6-12 years Late childhood: Pre pubertal: 10 – 13 years. Adolescence: 13 - 19 years Young adulthood 20-40 years Middle adulthood 40-65years Late adulthood 65 and more Chapter (3) Nutritional assessment Islamic University of Gaza Strip Nutritional assessment Nutrition plays a major role in the way an individual looks, feels,& behaves. The body ability to fight disease greatly depends on the individual's nutritional status 26 Major goals of nutritional assessment 1. Identification of malnutrition. 2. Identification of over consumption 3. Identification of optimal nutritional status. Components of Nutritional Assessment 1. Anthropometric measurement. 2. Biochemical measurement. 3. Clinical examination. 4. Dietary analysis 27 1. Anthropometric measurement Measurement of size, weight, and proportions of human body. Measurement includes: height, weight, skin fold thickness, and circumference of various body parts, including the head, chest, and arm. a direct and continuous relationship to morbidity and mortality in studies of large populations. High ratios of waist to hip circumference are associated Assess body mass index (BMI) to shows with higher risk for illness & decreased life span. BMI 28 = (Wt. in kilograms) = (High in meters) 2 60 (1.6)2 = 60 2.56 = 23.4 BMI RANGE Rang kg/m2 less than 16.0 16.0 - 18.4 18.5- 24.9 25–29.9 30-34.9 ≥ 35 Condition Very thin Thin Average Overweight Obese Highly obese 2. Biochemical Measurement Useful in indicating malnutrition or the development of diseases as a result of over consumption of nutrients. Serum and urine are commonly used for biochemical assessment. In assessment of malnutrition, commonly tests include: total lymphocyte count, albumin, serum transferrin, hemoglobin, and hematocrit …etc. These values taken with anthropometric measurements, give a good overall picture of an individual's skeletal and visceral protein status as well as fat reserves and immunologic response. 3. Clinical examination Involves, close physical evaluation and may reveal signs suggesting malnutrition or over consumption of nutrients. Although examination alone doesn't permit definitive diagnosis of nutritional problem, it should not be overlooked in nutritional assessment 31 Nutritional assessment technique for clinical examination A. Types of information needed Diet: Describe the type: regular or not, special, "e.g. teeth problem, sensitive mouth. Usual mealtimes: How many meals a day: when? Which are heavy meals? Appetite: "Good, fair, poor, too good". Weight: stable? How has it changed? 32 Food preferences: e.g." prefers beef to other meats" Food dislike:What & Why? Culture related? Usual eating places: Home, snack shops, restaurants. Ability to eat: describe inabilities, dental problems: "ill fitting dentures, difficulties with chewing or swallowing Elimination" urine & stool: nature, frequency problems Exercise & physical activity: how extensive or 33 deficient Psycho social - cultural factors: Review any thing which can affect on proper nutrition Taking Medications which affect the eating habits Laboratory determinations e.g.: “Hemoglobin, protein, albumin, cholesterol, urinalyses" Height, weight, body type "small, medium, large" After obtaining information, summarize your findings and determine the nutritional diagnosis and nutritional plan of care. Imbalanced nutrition: Less than body requirements, related to lack of knowledge and inadequate food intake Risk for infection, related to protein-calorie malnutrition B. Signs & symptoms of malnutrition Dry and thin hair Yellowish lump around eye, white rings around both eyes, and pale conjunctiva Redness and swelling of lips especially corners of mouth Teeth caries & abnormal missing of it Dryness of skin (xerosis): sandpaper feels of skin Spoon shaped Nails " Koilonychia “ anemia Tachycardia, elevated blood pressure due to excessive sodium intake and excessive cholesterol, fat, or caloric intake Muscle weakness and growth retardation 35 36 4. Dietary analysis Food represent cultural and ethnic background and socio- economic status and psychological meaning have many emotional and Assessment includes usual foods consumed & habits of food The nurse ask the client to recall every thing consumed within the past 24 hour including all foods, fluid, vitamins, minerals or other supplements to identify the optimal meals Should not bias the client's response to question based on the interviewer's personal habits or knowledge of recommended food consumption 37 Diseases affected by nutritional problems 1- Obesity: excess of body fat. 2- Diabetes mellitus. 3- Hypertension. 4- Coronary heart disease. 5- Cancer. 38 Chapter (4) Sleep-wakefulness patterns Islamic University of Gaza Strip Assessment of sleep-wakefulness patterns Normal human has “homeostasis” (ability to maintain a relative internal constancy) Any person may complain of sleep-pattern disturbance as a primary problem or secondary due to another condition 1/4 of clients who seek health care complain of a difficulty related to sleep 40 Factors affecting length and quality of sleep 1. Anxiety related to the need for meeting a tasks, such as waking at an early hour for work. 2.The promise of pleasurable activity such as starting a vacation. 3.The conditioned patterns of sleeping. 4. Physiologic wake up. 5. Age differences. 6. Physiologic alteration, such as diseases 41 Good sleep depends on the number of awakenings and the total number of sleeping hours The nurse can assess sleep pattern by doing interview with the client or using special charts or by EEG Disorders related to sleep 1.Sleep disturbances affects family life, employment, and general social adjustment 2. Feelings of fatigue, irritability and difficulty in concentrating 3. Difficulty in maintaining orientation 42 4. Illusions, hallucination (visual & tactile ) 5. Decreased psychomotor ability with decreased incentive to work 6. Mild Nystagmus 7.Tremor of hands Increase in gluco-corticoid and adrenergic hormone secretion 9. Increase anxiety with sense of tiredness 10. Insomnia "short end sleeping periods“ 11. Sleep apnea "periodic cessation of breathing that occurs during sleep 12. Hypersomnia: "sleeping for excessive periods” the sleep period may be extended to 16-18 hours a day 13. Peri-hypersomnia. "Condition that is described as an increased used for sleep "18-20 hours a day" lasts for only few days 14. Narcolepsy "excessive day time drowsiness or uncontrolled onset of sleep. 15. Cataplexy: abrupt weakness or paralysis of voluntary muscles e.g. arms, legs & face last from half second to 10 minutes, one or twice a year 16. Hypnagogic hallucinations: " Disturbing or frightening dream that occur as client is a falling a sleep 44 Assessment of sleep habits Let the client record the times of going to sleep and awakening periods, including naps. Allow client to described their sleep habits in their own words You can ask the following questions: How have you been sleeping?‖ Can you tell me about your sleeping habits?" Are you getting enough rest?" Tell me about your sleep problem" Good History includes: a general sleep history, psychological 45 history, and a drug history Chapter (5) Nursing Health History Islamic University of Gaza Strip Definition of Health History Systematic collection of subjective data which stated by the client, and objective data which observed by the nurse That using to determine a client functional health pattern status. 47 Phases of taking health history Two phases:The interview phase which elicits information (primary sources) The recording phase (secondary sources). 48 the Guidelines for Taking Nursing History Private, comfortable, environment. and quiet Allow the client to state problems and expectations for the interview. Orient the client the structure, purposes, and expectations of the history. 49 Guidelines for Taking Nursing History cont.. Communicate and negotiate priorities with the client Listen more than talk. Observe non verbal communications e.g. "body language, voice tone, and appearance". 50 Guidelines for Taking Nursing History cont.. Review information about past health history before starting interview. Balance between allowing a client to talk in an unstructured manner and the need to structure requested information. Clarify the descriptors) 51 client's definitions (terms & Guidelines for Taking Nursing History cont.. Avoid yes or no question (when detailed information is desired). Write adequate notes for recording? Record nursing health history soon after interview. 52 Types of Nursing Health History Complete health history: taken on initial visits to health care facilities. Interval health history: collect information in visits following the initial data base is collected. Problem- focused health history: collect data about a specific problem 53 Components of Health History 1-Biographical Data: This includes Full name Address and telephone numbers (client's permanent contact of client) Birth date and birth place. Sex Religion and race. Marital status. Social security number. Occupation (usual and present) Source of referral. Usual source of healthcare Source and reliability of information. Date of interview. 54 2- Chief Complaint: “Reason For Hospitalization Examples of chief complaints: Chest pain for 3 days. Swollen ankles for 2 weeks. Fever and headache for 24 hours. Pap smear needed. Physical examination needed for camp. 55 SYMPTOM ANALYSIS P Q R ST a. Provocative or Palliative First occurrence : What were you doing when you first experienced or noticed the symptom? What to trigger it ? stress? Position?, activity? What seems to cause it or make it worse? For a psychological symptom . What relieves the symptom : change diet? Change position ? Take medication ? Being active? Aggravation: what makes the symptom worse? SYMPTOM ANALYSIS P Q R ST b. Quality Or Quantity QUALITY: How would you describe the symptom- how it feels, looks, or sounds? QUANTITY: How much are you experiencing now? Is it so much that it prevents you from performing any activity? SYMPTOM ANALYSIS P Q R S T C. Region Or Radiation Region : Where does the symptom occur? Radiation : Does it travel down your back or arm, up your neck or down your legs? SYMPTOM ANALYSIS P Q R S T d. Severity scale Severity How bad is symptom at its worst? Course Does the symptom seem to be getting better, getting worse? SYMPTOM ANALYSIS P Q R S T e. Timing Onset : On what date did the symptom first occur Type of onset : How did the symptom start sudden? Gradually? Frequency : How often do you experience the symptom ; hourly ? Daily ? Weekly? monthly Duration : How long does an episode of the symptom last 3-History of present illness Gathering information relevant to the chief complaint, and the client's problem, relevant treatment. 61 including data, and essential self and medical Component of Present Illness Introduction: "client's summary and usual health". Investigation of symptoms: "onset, date, gradual or sudden, duration, frequency, location, quality, and alleviating or aggravating factors". Negative information. Relevant family information. Disability "affected the client's total life". 62 4- Past Health History: The purpose: (to identify all major past health problems of the client) This includes: Childhood illness e.g. history of rheumatic fever. History of accidents and disabling injuries 63 Past Health History. Cont… History of hospitalization (time of admission, date, admitting complaint, discharge diagnosis and follow up care. History of operations "how and why this done" History of immunizations and allergies. Physical examinations and diagnostic tests. 64 5-Family History The purpose: to learn about the general health of the client's blood relatives, spouse, and children and to identify any illness of environmental genetic, or familiar nature that might have implications for the client's health problems. 65 Family History. Cont… Family history of communicable diseases. Heredity factors associated with causes of some diseases. Strong family history of certain problems. Health of family members "maternal, parents, siblings, aunts, uncles…etc.". Cause of death of the family members "immediate and extended family". 66 6-Environmental History: Purpose “To gather information about surroundings of the client", including physical, psychological, social environment, and presence of hazards, pollutants and safety measures." 67 7- Current Health Information The purpose is to record major current health related information. Allergies: environmental, ingestion, drug, other. Habits "alcohol, tobacco, drug, caffeine" Medications taken regularly "by doctor or self prescription Exercise patterns. Sleep patterns (daily routine). The pattern life (sedentary or active) 68 8- Psychosocial History: Includes: How client and his family cope with disease or stress, and how they responses to illness and health. You can assess if there is psychological or social problem and if it affects general health of the client. 69 9- Review of Systems (ROS) Collection of data about the past and the present of each of the client systems. (Review of the client’s physical, sociologic, and psychological health status may identify hidden problems and provides an opportunity to indicate client strength and disabilities 70 Physical Systems Which includes assessment of:- General review of skin, hair, head, face, eyes, ears, nose, sinuses, mouth, throat, neck nodes and breasts. Assessment of respiratory and cardiovascular system. Assessment of gastrointestinal system. Assessment of urinary system. Assessment of genital system. Assessment of extremities and musculoskeletal system. Assessment of endocrine system. Assessment of heamatoboitic system. Assessment of social system. Assessment of psychological system. 10- Nutritional Health History “Discussed Before” 72 11- Assessment of Interpersonal Factors. This includes :Ethnic and cultural background, spoken language, values, health habits, and family relationship. Life style e.g. rest and sleep pattern Self concept perception of strength, desired changes Sexuality developmental level and concerns Stress response coping pattern, support system, perceptions of current anticipated stressors. 73 Chapter (6) Functional Health Pattern Islamic University of Gaza Strip Definition of (NANDA) The North American Nursing Diagnosis Association (NANAD 1994) defines a nursing diagnosis as “A clinical judgments about individual, family or community response to actual and potential health problems and life responses” 75 Functional health pattern (NANDA) 1- Health Perception-Health Management Pattern 2- Nutritional—Metabolic Pattern 3- Elimination Pattern 4- Activity—Exercise Pattern 5- Sexuality—Reproduction Pattern 6- Sleep—Rest Pattern 7- Sensory—Perceptual Pattern 8- Cognitive Pattern 9- Role—Relationship Pattern 10- Self-Perception-Self-Concept Pattern 11- Coping-Stress Tolerance Pattern 12-Value—Belief Pattern Health Perception-Health Management Pattern 1- Determine how the client perceives and manages his or her health. 2- Compliance with current and past nursing and, medical recommendations. 3- The client's ability to perceive the relationship between activities of daily living and health. Subjective Data Client's Perception of Health: Describe your health. Client's Perception of Illness Describe your illness or current health problem. Health Management and Habits Tell me what you do when you have a health problem. Compliance with Prescribed Medications and Treatments Have you been able to take your prescribed medications? If not, what caused your inability to do so? Objective Data Refer to General Physical Survey Associated Nursing Diagnoses Wellness Diagnoses Effective Management of Therapeutic Regimen Risk Diagnoses Risk for Injury Risk for Suffocation Risk for Trauma Actual Diagnoses Altered Growth and Development Ineffective Management of Therapeutic Regimen: Individual Ineffective Management of Therapeutic Regimen: Family Ineffective Management of Therapeutic Regimen: Community Noncompliance. Nutritional-Metabolic Pattern Assessing the client's nutritional-metabolic pattern is to determine the client's dietary habits and metabolic needs. The conditions of hair, skin, nails, teeth and mucous membranes are assessed. Subjective Data Dietary and Fluid Intake Describe the type and amount of food you eat at breakfast, lunch, and supper on an average day Do-you take any vitamin supplements? Describe. Do you find it difficult to tolerate certain foods? Specify. Do you ever experience nausea and vomiting? Describe. Do you ever experience abdominal pains? Describe Condition of Skin Describe the condition of your skin. How well and how quickly does your skin heal? Do you have any skin lesions? DescribeDo you have any itching? What do you do for relief? Condition of Hair and Nails Have you had difficulty with scalp itching or sores? Do you use any special hair or scalp care products? Have you noticed any changes in your nails? Color Cracking? Shape? Lines? Metabolism What would you consider to be your "ideal weight"? Have you had any recent weight gains or losses? Do you have any intolerance to heat or cold? Have you noted any changes in your eating or drinking habits? Explain. Have you noticed any voice changes? Objective Data Assess the client's temperature, pulse, respirations, and height and weight. Wellness Diagnoses 0pportunity to enhance nutritional metabolic pattern Opportunity to enhance effective breastfeeding Opportunity to enhance skin integrity Risk Diagnoses Risk for Altered Body Temperature Hypothermia Risk for Infection Risk for altered nutrition less than body requirements . Risk for Aspiration Actual Diagnoses Fluid Volume Deficit Fluid Volume Excess Altered Nutrition: Less than body requirements Altered Nutrition: More than body requirements Ineffective Breastfeeding Altered Oral Mucous Membrane Impaired Skin Integrity. Elimination Pattern Adequacy of the client's bowel and bladder. The client's bowel and urinary habits. Bowel or urinary problems Use of urinary or bowel elimination devices. Subjective Data Bowel Habits How frequent are your bowel movements? Do you use laxatives? What kind and how often do you use them? Do you use enemas or suppositories? How often and what kind? Do you have any discomfort with your bowel movements? Describe. Bladder Habits How frequently do you urinate? What is the amount and color of your urine? Do you have any of the following problems with urinating: Pain? Blood in urine? Difficulty starting a stream? Incontinence? Voiding frequently at night? Voiding frequently during day? Bladder infections? Have you ever had a urinary catheter? Describe. When? How long? Objective Data Refer to abdominal assessment, and the rectal assessment. Associated nursing-Diagnoses Wellness Diagnoses Opportunity to enhance adequate bowel elimination pattern Opportunity to enhance adequate urinary elimination pattern Risk Diagnoses Risk for constipation Risk for altered urinary elimination Actual Diagnoses Altered Bowel Elimination Constipation Diarrhea Bowel Incontinence Altered Urinary Elimination Patterns of Urinary Retention Total Incontinence Stress Incontinence Activity-Exercise Pattern Activities of daily living, including routines of exercise, leisure, and recreation. Activities necessary for personal hygiene, cooking, shopping, eating, maintaining the home, and working. An assessment is made of any factors that affect or interfere with the client's routine activities of daily living. Subjective Data Describe your activities on a normal day. (Including hygiene activities, eating activities.) Do you have difficulty with any of these self-care activities? Explain. Does anyone help you with these activities? How? Do you use any special devices to help you with your activities? Does your current physical health affect any of these activities e.g. dyspnea, shortness of breath, palpations, chest pain. pain, stiffness, weakness)? Explain. Occupational Activities Describe what you do to make a living. Do you feel it has affected your health? How has your health affected your ability to work? Objective Data Refer to Thoracic and Lung Assessment Cardiac Assessment PeripheralVascular Assessment Musculoskeletal Assessment. Associated Nursing Diagnoses Wellness Diagnoses Opportunity to enhance effective cardiac output Opportunity to enhance effective self-care activities Opportunity to enhance adequate tissue perfusion Opportunity to enhance effective breathing pattern Risk Diagnoses Risk for Disorganized Infant Behavior Risk for Peripheral Neurovascular Dysfunction Risk for altered respiratory function Actual Diagnoses Activity Intolerance Impaired Gas Exchange Ineffective Airway Clearance Ineffective Breathing Pattern Disuse syndrome Impaired Physical Mobility Inability to Sustain Spontaneous Ventilation Altered Tissue Perfusion Sexuality-Reproduction Pattern Subjective Data 1- Female Menstrual history: Last cycle begin? Duration ? Any change or abnormality ? Describe any mood changes or discomfort before, during, or after your cycle Obstetric history How many times have you been pregnant? Describe the outcome of each of your pregnancies. If you have children, what are the ages and sex of each? Explain any health problems or concerns you had with each pregnancy. If pregnant now . Contraception What do you or your partner do to prevent pregnancy? Describe any discomfort or undesirable effects this method produces. Have you had any difficulty with fertility? Explain Special problems Do you have or have you ever had a sexually transmitted disease? Describe. Describe any pain, burning, or discomfort you have while voiding. Objective Data Refer to Breast Assessment, d Abdominal Assessment, and urinaryReproductive Assessment Associated nursing Diagnoses Wellness Diagnosis: Opportunity to enhance sexuality patterns Risk-Diagnosis Risk for altered sexuality pattern Actual Diagnoses Sexual Dysfunction, Altered Sexuality Patterns Sleep-Rest Pattern Subjective data Sleep Habits: How would you rate the quality of your sleep? Special Problems Do you ever experience difficulty with falling asleep? Remaining asleep? Do you ever feel fatigued after a sleep period? Sleep Aids What helps you to fall asleep? medications? reading? relaxation technique?WatchingTV? Listening to music? Objective Data 1. Observe appearance a. Pale b. Puffy eyes with dark circles 2. Observe behavior a.Yawning b. Dozing during day c. Irritability d. Short attention span Associated nursing Diagnoses Wellness Diagnosis: Opportunity to enhance sleep Risk Diagnosis Risk for sleep pattern disturbance Actual Diagnosis: Sleep Pattern Disturbance. Sensory-Perceptual Pattern Subjective Data Describe your ability to see, hear, feel, taste, and smell. Describe any difficulty you have with your vision, hearing, and ability to feel (e.g., touch, pain, heat, cold), taste (salty, sweet, bitter, sour), or smell. Pain Assessment Complete Symptom Analysis Special Aids: What devices (e.g., glasses, contact lenses, hearing aids) Describe any medications you take to help you with these problems. Objective Data Refer to the section on Nose and Sinus Assessment, Eye Assessment, and Ear Assessment. Associated Nursing Diagnoses Wellness Diagnosis: Opportunity to enhance comfort level Risk Diagnoses Risk for pain Actual Diagnoses Pain Cognitive Pattern Subjective Data Ability to Understand: Explain what your doctor has told you about your health. Ability to Communicate: Can you tell me how you feel about your current state of health? Ability to Remember: Are you able to remember recent events and events of long ago? Explain. Ability to Make Decisions: Describe how you feel when faced with a decision. Objective Data Refer to the Mental Status Assessment Associated nursing Diagnoses Wellness Diagnosis: Opportunity to enhance cognition Risk Diagnosis: Risk for altered thought processes Actual Diagnoses: Acute confusion Chronic Confusion Knowledge Deficit (Specify) Impaired Memory Role-Relationship Pattern Subjective Data Perception of Major Roles and Responsibilities in Family Describe your family. Are there any major problems now? Perception of Major Roles and Responsibilities at Work Describe your occupation. What is your major responsibility at work? Perception of Major Social Roles and Responsibilities Describe your neighborhood and the community in which you live. Objective Data 1. Outline a family genogram for your client. 2. Observe your client's family members. Associated Nursing Diagnoses Wellness Diagnoses: Opportunity to enhance effective relationships Opportunity to enhance effective communication Risk Diagnoses: High risk for Loneliness Risk for Altered Parent/Infant/Child Attachment Actual Diagnoses: Impaired Verbal Communication Impaired Social Interaction: Social Isolation Coping-Stress Tolerance Pattern Subjective Data Perception of Stress and Problems in Life Describe what you believe to be the most stressful situation in your Life. How has your illness affected the stress you feel? Coping Methods and Support Systems: What do you usually do first when faced with a problem? What helps you to relieve stress and tension? Do you use medication, drugs, or alcohol to help relieve stress? Explain. Objective Data Refer to the Mental Status Assessment. Associated nursing Diagnoses Wellness Diagnoses Opportunity to enhance effective individual coping. Opportunity to enhance family coping Risk Diagnoses: Risk for self-harm Risk for suicide Actual Diagnoses: Ineffective Individual Coping Ineffective Family Coping: Disabling Value-Belief Pattern Subjective Data Values, Goals, and Philosophical Beliefs Religious and Spiritual Beliefs: Are there certain health practices or restrictions that are important for you to follow while you are ill or hospitalized? Explain. Objective Data Observe religious practices Bible , clergy Observe client's behavior for signs of spiritual distress Anxiety, Anger , Depression , Doubt, Hopelessness and Powerlessness Associated Nursing Diagnoses Wellness Diagnosis: Potential for Enhanced Spiritual Well-Being Risk diagnosis: Risk for spiritual distress Actual Diagnosis: Spiritual disturbance (distress of the human spirit). Chapter (7) Physical Assessment Techniques Islamic University of Gaza Strip Indications for the Physical Exam Routine screening Eligibility prerequisite for health insurance, military service, job, sports, school Admission to a hospital or long term care facility 112 STEPS OF ASSESSMENT Think Organize Don’t forget…Nutrition / Height & Weight Environment: Accommodate special needs (cultural sensitivity) Equipment - clean surface & clean equipment Room - quiet, warm & well lit Maintain privacy Observe & Listen 113 DON’T FORGET REVIEWING GENERAL INFORMATION INTRODUCTION TO CLIENT OBTAINING THE HEALTH HISTORY PAIN ASSESSMENT THIS IS KEY TO HOLISTIC APPROACH 114 Physical Assessment There are four techniques to use in performing physical assessment: 1.Inspection 2. Palpation 3. Percussion 4. Auscultation Note: there are five addition skill known as olfaction 115 116 1. Inspection: Inspection is defined as “the use of the senses of vision, smell and hearing to observe the normal condition or any deviations from normal of various body parts.” The nurse inspects or looks body parts to detect normal characteristics or significant physical sings. Inspection helps to know normal characteristics before trying to distinguish abnormal findings in different ages. The quality of an inspection depends on the nurse's willingness to spend time doing a thorough job. 117 Inspection Use vision, hearing & smell Always first Look for symmetry Use good lighting Use good exposure 118 Principles of Accurate Inspection Good lightening either day light or artificial light is suitable. Expose body parts being observed only. look before touching. warm room for examination of the client “not cold not hot". Observe for color, size, location, texture, symmetry, odors, and sounds. Compare each area inspected with the opposite possible. Use pen light to inspect body cavities. 119 side of body if Palpation Touch & feel with hands to determine: Texture – use fingertips (roughness, smoothness). Temperature – use back of hand (warm, hot, cold). Moisture (dry, wet, or moist). Organ location and size Consistency of structure (solid, fluid, filled) Slow and systematic Light to deep Light palpation (tenderness) Deep palpation (abdominal organs/masses) Principles for Accurate Palpation Examiner finger nails should be short. Use sensitive part of the hand. Light Palpation precedes deep palpation. Start with light then deep palpation Tender area are palpated last Tell client to take slow deep breath to enhance muscle relaxation. Examine condition of the abdominal organs Depressed areas must be approximately “2cm” Assess turger of skin measured by lightly grasping the body part 121 with finger tips. Light palpation 122 Deep palpation 123 Percussion Tap a portion of the body to elicit tenderness that varies with the density of underlying structures. Percussion denotes location, size and density of underlying structures, percussion requires dexterity. Methods of percussion: Direct method: involving striking the body surface directly with one or two fingers. Indirect method: performed by placing the middle finger of the examiner’s non dominant hand “pleximeter hand” firmly against the body surface with palm and fingers remaining off the skin, and the tip of the middle finger of the dominant hand “plexor” strikes the base of the distal joint of the pleximeter. Use a quick & sharp stroke Percussion 125 Description of sounds Sound produced by the body is characterized by intensity, frequency, duration and quality. Intensity, or loudness, associated with physiologic sound is low; thus, the use of the stethoscope is needed. Frequency, or pitch, of physiologic sound is in reality “noise” in that most sounds consist of a frequency spectrum as opposed to the single-frequency sounds that we associate with music or the tuning fork. Duration relates to the time elapsed from the beginning of the sound till the end of the sound. Quality of sound relates to overtones that allow one to distinguish between different sounds. 126 Sounds produced by percussion Sound Tympany Intensity Loud Pitch High Duration Moderate Quality Drum like Example Large pneumothorax Resonance Moderate Low Long hollow Normal lung Very Longer Booming Emphysematous low than to loud Hyper- Very loud resonance lung resonance Dullness Soft to High Moderate Thud like Liver High Short Flat Muscle moderate Flatness 127 Soft Five percussion sounds produced in different body regions 1. Resonant – normal lung 2. Hyper resonant: it’s a louder and lower pitched than resonant sounds. Normally heard in children and very thin adults , and abnormally in emphysema 3. Tympany : A hollow drum-like sound produced when a gas-containing cavity is tapped sharply. Tympany is heard if the chest contains free air (pneumothorax) or the abdomen is distended with gas air filled (stomach) 4. Dull or thud like sounds are normally heard over dense areas such as the heart or liver. Dullness replaces resonance when fluid replaces air-containing lung tissues, such as occurs with pneumonia, pleural effusions, or tumors 5. Flat: shown in no air areas such as thigh muscle, bone and tumor Auscultation “To listen for various breath, heart, and bowel sounds” Direct or immediate auscultation is accomplished by the unassisted ear that is without amplifying device. This form of auscultation often involves the application of the ear directly to a body surface where the sound is most prominent. Mediate auscultation: the use of sound augmentation device such as a stethoscope in the detection of body sounds. Auscultation Listening to body sounds Movement of air (lungs) Blood flow (heart) Fluid & gas movement (bowels) Remember the sound changes in the abdomen… 130 HOW TO BEGIN… Positions for physical exam Using a stethoscope: Longer the tube – more sound has to travel Hold diaphragm firmly against client’s skin (NOT THROUGH CLOTHING) If using bell – less pressure Warm in your hands first! Listen / Concentrate on the sounds 131 Olfaction Another skill that used during assessment, certain alteration is body function create characteristic body odors, smelling can detect abnormalities that unrecognized by other means. Assessment of characteristic odors: Alcohol odor from oral cavity means ingestion of alcohol. Ammonia from urine means urinary tract infection. Body odor from skin, particularly in areas where body parts rub together means poor hygiene, excess perspiration (bromidrosis). 132 Feces odor from wound site means wound abscess, but if this odor from vomitus this means bowel obstruction, and if the odor from rectal area this means fecal incontinence. Foul–smelling stools in infant from stool means mal absorption syndrome. Halitosis from oral cavity means poor dental and oral hygiene, gum disease. Sweet, fruity ketones from oral cavity may be from diabetic acidosis. Musty odor from casted body part means infection inside cast. Fetid odor from tracheostomy or mucous secretions means infection of bronchial tree (pseudomonas bacteria). Basic Guidelines for physical Assessment 1. Obtain a nursing history and survey 2. Maintain privacy. 3. Explain the procedure 4. Always inspect, palpate, percuss, and then auscultate 5. 6. 7. 8. except abdominal start with auscultate Compare symmetrical sides If abnormality (Symptom analysis ) Client teaching Allow time for client’s questions. "Remember: the most important guideline for adequate physical assessment is conscious, continuous practice of physical assessment skills". Variation in physical assessment of the pediatric client. Sequence of physical assessment is dependent upon the developmental level of the client. Allowing time for interaction with the child prior to beginning the examination helps to reduce fears. In certain age groups, portions of assessment will require physical restraint of the client with the help of another adult. Distraction and play should be intermingled throughout the examination to assist in maintaining rapport with the pediatric client. Involving assistance from the child’s significant caregiver may facilitate a more meaningful examination of the younger client. The examiner should be prepared to alter the order of the assessment and approach to the child based on the child’s response. Protest or an uncooperative attitude toward the examiner is a normal finding in children from birth to early adolescence, throughout parts or even all the assessment process. Variations for physical assessment of the geriatric client. Remember: normal variation related to aging may be observed in all parts of the physical examination. Dividing the physical assessment into parts in order to avoid fatigue in the older client. Provide room with comfortable temperature and no drafts. Allow sufficient time for client to respond to directions. If possible assess the elderly clients in a setting where they have an opportunity to perform normal activities of daily living in order to determine the client’s optimum potential. Chapter (8) Vital Signs and General Assessment Islamic University of Gaza Strip Vital signs and general assessment Equipment needed: Balance scale. Tape measure. Thermometer. Sphygmomanometer. Stethoscope. Subjective Data: Reason for seeking health care and major concern about current health, current age, height, and weight, recent weight changes, fever, history of hypertension, hypertension, difficulty breathing, changes impulse or heart rate. 139 Objective Data: Observe client from head to toe to note any gross abnormalities in appearance or behaviors. Assess vital signs, temperature, pulse, respirations, and blood pressure to detect any severe deviations and to acquire base line data. Weight the client and measure for height with shoes, and heavy clothing removed. 140 Vital signs (assessment) include: Assessment of temperature, pulse, respiration and blood pressure are known as life signs. Vital signs are indicators of the body’s physiologic status and response to physical, environmental and physiologic stressors. Vital signs reveal the client’s current ability to maintain body temperature regulation, to maintain local and systemic blood flow, and to provide oxygenation of body tissues. A.Temperature Body temperature is difference between heat produced and heat lost. The hypothalamus acts as the body's thermostat to maintain between the body's heat-producing function (metabolism, shivering, muscle contraction, exercise and thyroid activity) and heat losing methods (radiation, convection) 141 Method of measurement a. Oral b. Rectal c. Axillary d. Forehead e.Tympanic Remember Routinely, where accuracy is not crucial, an oral temp will sufficient. Rectal temperature is the most accurate. Unless contraindicated a rectal temperature is often preferred. Factors influencing of temperature Biologic rhythms Gender: women has greater fluctuations in body temperature than men because change of hormones Environmental effect (hot, cold), Physiologic change(exercise) Drugs and Age (child have slightly higher normal temperature, elderly people have decrease body temperature). B. Pulse The pulse reflects the force of the heart contracting. Also reflects stroke volume, the mount of blood ejected with each contraction. A pulse deficit (a difference between the apical and radial pulse rate) Factors influencing of pulse 1. Pain 2. Emotion 3. Exercise 4. Prolong heat application 5. Decrease BP, and increase temperature. 6. Poor oxygen in the blood. Remember Palpate the radial pulse and count for at least "30" second. If the pulse is irregular, count for full minute and note the number of irregular beats per minute. Note is the pulse against your finger strong or weak (Amplitude of Rhythm: regular or irregular Amplitude of rhythm Absent 0 Thready 1 Weak 2 Normal 3 Bound 4 Site of pulse Temporal, Carotid, Brachial, Radial, Femoral, Dorsalis Pedis , Popliteal, Posterior Tibia and Apical. N.B pulse rate is "60-100 b/m" regular in rhythm. The normal pulse rate varies from a low of 50 bpm in healthy, athletic young adults to rates well in excess of 100 bpm after exercise or during 144 times of excitement 145 C. Respiration: Count the number of respiration (rate), in full minute Respiration: normally "16-20 breath/minute" (for healthy adult person). Note rhythm (regular or irregular) and depth of breathing (reflects the tidal volume, described as shallow or deep breathing). Factors influencing of reparation 1. Age Newborn 35 breath / minute , 1 year 30 breath / minute , 6 year 21 breath / minute, 10 year 19 breath / minute , 18 year 16-18 breath / minute 2. Any disease 3. Exercise 4. Emotion D. Blood pressure: Measure Blood Pressure in both arms. Pulse pressure: the difference between the systolic and the diastolic pressures (normally is 30 to 40 mm Hg) Palpate the systolic pressure before using the stethoscope in order to detect an auscultatory gap. Apply cuff firmly, if too tight (small) it will give falsely high reading. Use cuff in appropriate size. Note position of client when measuring blood pressure. Monitor blood pressure after client is seated or supine quietly for "10" minute. Repeat after two minutes.Then repeat with client standing. Factors influencing the BP 1. Age Newborn 40 mmHg/systolic / 20 diastole 1 month 84/54 mmHg 1 year 95 /65 mmHg 6 year 105 / 65 mmHg 10 – 13 year 120 / 80 mmHg 14- 17 year 120/80 mmHg 18 year 120/80 mmHg Normal range 100 – 140mmHg (systolic) and from 60-90 mmHg/( diastolic) 2. Sex 3. Emotion 4. Position: Laying down 4. After meal 5. Exercise 148 Instrumentation used in assessment Instruments, or “equipments” used during physical assessment should be readily accessible, clean, in proper working order. Ophthalmoscope: "lighted instrument for visualization of the eye". Otoscope: for examination of the ear. Snellen eye chart: used as a screening test for vision. Nasal speculum: used for assessment of the nose. Vaginal speculum: examination of the vaginal canal and cervix. Tuning fork: for testing auditory function and vibratory perception. Percussion hammer: “reflex hammer” used to test reflexes and determine tissue density. 149 150 Positions Each position has it's specialty for parts of examination. Draping during assessment is used to prevent unnecessary exposure. Drapes may be paper, cloth, or bed linens I. Sitting position Areas Assessed: Head and neck, back, posterior thorax and lungs, anterior thorax and lungs, breasts, axially, heart, vital signs, and upper extremities Rationale: Sitting upright provides full expansion of lungs and provides better visualization of symmetry of upper body parts. Limitations: Physically weakened client may be unable to sit. Examiner should use supine position with head of bed elevated instead. II. Supine position Areas Assessed: Head and neck anterior thorax and lungs, breasts, axillae, heart, abdomen, extremities, and pulses Rationale: This is most normally relaxed position. It prevents contracture of abdominal muscles and provides easy access to pulse sites. Limitations: If client becomes short of breath easily, examiner may need to raise head of bed. III. Dorsal position: Areas Assessed: Head and neck, anterior thorax and lungs, Breasts, axillae and heart. Rationale: Clients with painful disorders are more comfortable with knees flexed. Limitations: Position is not used for abdominal assessment because it promotes contracture of abdominal muscles IV. Lithotomy position: Areas Assessed: Female genitalia and genital tract Rational: This position provides maximal exposure of genitalia and facilitates insertion of vaginal speculum. Limitations: Lithotomy position is embarrassing and uncomfortable, so examiner minimizes time that client spends in it. Client is kept well draped. Client with severe arthritis or other joint deformity may be unable to assume this position. V. Sims’ position: Areas Assessed: Rectum and vagina Rationale: Flexion of hip and knee improves exposure of rectal area. Limitations: Joint deformities may hinder client’s ability to bend hip and knee. VI. Prone position: Areas Assessed: Musculoskeletal system Rationale: This position is used only to assess extension of hip joint. Limitations: This position is intolerable for client with respiratory difficulties. VII. Knee-chest position: Areas Assessed: Rectum. Rationale: This position provides maximal exposure of rectal area. Limitations: This position is embarrassing and uncomfortable. Clients with arthritis or other joint deformities may be unable to assume this position. 155 Chapter (9) Assessment of Skin, Hair and Nails Islamic University of Gaza Strip Structure of the Integument The skin is the largest organ of the body comprising 15 percent of total body weight. Layers of the skin A. Epidermis B. Dermis C. Subcutaneous tissue Epidermal appendages Hair Nails Glands: two types of skin glands: 1. Sweat Gland Eccrine sweat glands: are widely distributed and open directly onto the skin surface Apocrine sweat glands: open into hair follicle in axillary and genital areas 2. Sebaceous glands: Produce sebum(oily secretion) 158 Functions of skin and epidermal appendages Barrier to water and electrolyte loss Regulation of body heat Sensory organ for touch, temperature, and Pain Production of protective skin film by eccrine and sebaceous glands Participation in production of vitamin Wound repair 159 Assessing the Integument 1. Subjective data Skin infection, rashes, lesions, itching. Precipitating factors: stress, weather, drugs Changes in skin color, lesions Amount of sun exposure Scalp lesions, itching, and infections. Changes in texture and amount of hair. Changes in nails and cuticles nail breaking 160 2. History of current symptom Are you having experience of skin problem, such as rashes, lesion Describe any birthmarks, tattoos, or moles Have you noticed any changed in your ability to feel pain, pressure, light touch, or temperature changed? Have you had any hair loss or change in the condition of your hair? Have you had any change in the condition or appearance of your nails? Describe any previous problem within the skin, hair or nails ( past history) Have you ever had any allergic skin reaction to food, medication, plants? Has anyone in your family had a recent illness, rash, or other skin problem? (Family history) 3. Physical Assessment Equipment Penlight Tongue depressor Magnifying glass Flashlight Centimeter rule Wood’s lamp Gloves Technique to examination of skin Inspection Palpation Inspections and palpation of skin Color Moisture Temperature Turgor Vascular changes Edema Skin odors are usually noted in the skin fold. 162 Thickness Lesions 163 Inspection color of skin Skin color varies from body part to body part and from person to person. Assessment first involves area of skin not exposed to the sun e.g. palms of the hands. Pallor easily perceived in the buccal “mouth” mucosa particularly in individuals with dark skin. Cyanosis readily seen in area of least pigmentation e.g. lips, nail beds conjunctiva and palm. Jaundice orYellow seen in client’s sclera. Erythema may indicate circulatory changes 164 165 Palpation moisture of skin Skin is normally smooth and dry. Skin folds e.g. axillae are normally moist. In presence of lesions or ooze fluid, nurse must wear gloves to prevent exposure to infections drainage Moisture indicates: 1- Degree of client’s hydration 2- Condition of the outer lipid layer of the skin surface Dry (xerosis):Vitamin A def. and Myxedema Oily: Acne 166 Palpation of Temperature Temperature of skin depends on the amount of blood circulating through dermis. Generalized warmth: (Fever, Hyperthyroidism) Local warmth: (Inflammation) Coolness: (Hypothyroidism, Frost bite, Hypothermia, Shock, Low cardiac output) Palpation of skin with dorsum of the hand. Assessment of skin is critical point in some conditions such as: after cast application, or after vascular surgery. 167 Palpation of Texture Texture of skin normally smooth, soft and flexible If any abnormalities in texture found you must ask the client is he exposed to any recent injury to the skin? Nurse determines whether the client’s skin is smooth or rough, thin or thick, tight or supple (flexible). Very Soft: (Thyrotoxicosis) Tight: (Scleroderma = hard skin) Rough: (Hypothyroidism) 168 Palpation of Turgor Turgor: is the skin elasticity diminished by edema or dehydration. Assessment of turgor done by pinching skin between the thumb and forefinger and released. Normally skin return immediately to its position. Failure of this process means dehydration. Decrease in turgor predisposes the client to skin breakdown. Palpation of Vascularity Vascularity: Assessment of circulation of skin E.g. petechiae may indicate serous blood clotting disorders, drug reactions or liver disease. Inspection and Palpation of Edema Edema : "Build up of fluid in tissues“ Inspected for location, color, and shape. Palpates areas of edema to determine mobility, consistency, and tenderness Inspection and Palpation of Lesions Normally skin free of lesions except common freckles. If lesion present, inspection must done for distribution, arrangement, morphology, color and size Palpation for lesion’s mobility, contour (flat, raised or depressed) and consistency (soft or hard are indicated). Cancerous lesions frequently undergo changes in color and size. Hair and Scalp Assessment done for distribution, thickness, texture, and lubrication of the hair. Some events which affect the distribution of hair over the body e.g. client with hormone disorders, woman with hirsutism Amount of hair covering extremities may be reduced as a result of aging and arterial insufficiency especially in lower limbs. Scaliness or dryness of the scalp is frequently caused by dandruff or psoriasis. 171 Nails Assessment Nails reflect an individual's general state of health, state of nutrition, and occupation. Nails are normally transparent, smooth, and convex, with a nail bed angle of about 160 degrees. The surrounding cuticles are smooth, intact and without inflammation. Nail bed is normally firm on palpation. Nails normally grow at a constant rate. Abnormal condition of nail Anonychia: complete absence of nails Platunychia: flatting nails Koilonychia : nails like spoon shape (iron deficiencies anemia) Racket nail: fattened and expanded nails Onycholysis: separation of nail form nail bed (thyrotoxicosis) Melanoychia: presence of brown color in nails plate Paronychia: inflammation of tissue surrounding the nail 173 174 Chapter (10) Assessment of respiratory system Islamic University of Gaza Strip Anatomy of Respiratory System The lung is a two cone-shaped, elastic structure suspended within the thoracic cavity. Lung are paired, they are not complete symmetric, the right lung contain three lobe, whereas the left lung contain only two lobes. The apex of each lung extended slightly above the clavicle, where the base is at the level of diaphragm The thoracic cavity contains the nasopharynx, larynx, trachea, bronchi, bronchioles, alveoli. The thoracic cavity is lined by a thin, double- layered serous membrane 176 collectively called the pleural membrane 177 178 Assessment of respiratory system Subjective data: the nurse must ask the client about: Coughing (productive, non productive) Sputum (type & amount) Allergies, dyspnea or SOB (at rest or on exertion). Chest pain, history of asthma, bronchitis, emphysema, tuberculosis. Cyanosis, pallor. Exposure to environmental inhalants (chemicals, fumes). History of smoking (amount and length of time) 179 Technique for Respiratory Exam Before beginning, if possible: Quiet environment Proper positioning (patient sitting for posterior thorax exam, supine for anterior thorax exam) Expose skin for auscultation Patient comfort, warm hands and diaphragm of stethoscope, be considerate of women (drape sheet to cover chest) After that the nurse should apply the four techniques; 180 Inspection, Palpation, Percussion and Auscultation Initial Respiratory Survey (Inspection) Observe the patient’s breathing pattern Rate (normal vs. increased/decreased) Depth (shallow vs. deep) Effort (any sign of accessory muscle use, inspect neck) Assess the patient’s color Cyanosis Normal Respiratory Rates Infant 30-60 Toddler 24-40 Preschooler 22-34 School-age child 18-30 Adolescent 12-16 Adult 16-20 181 Inspection and assessment of respiration patterns Assess the skin and overall symmetry and integrity of the thorax. Assess thoracic configuration. Client must be uncovered to the waist, and in sitting position without support. Observation of skin may give you knowledge about nutritional status of the client. Anterior- posterior diameter of thorax in normal person less than the transverse diameter = (1:2). Assess for abnormality of configuration, e.g. pigeon chest, funnel chest, spinal deformities. Assess ribs and inter spaces on respiration – may give information about obstruction in air flow e.g. bulging of inter spaces on expiration may be from obstruction to air out flow “tumor, aneurysm, cardiac enlargement” Assess pattern of respiration Normally: men and children – breathe diaphragmatically and Women breathe thoracically or costally. Tachypnea: respiratory rate over than 20/m for adult. Bradypnea: respiratory rate less than 10/m. Palpation: palpate areas of chest especially areas of abnormalities. If clients complains: all chest areas must palpated carefully for tenderness, bulges, or any movements 183 Assess thoracic expansion: Anterior: put your hands over anterior-lateral chest and thumbs extended along costal margin pointing to xiphoid process. Posterior: thumbs placed at level of T 10 with palms placed on posterior-lateral chest. By two ways you feel amount of thoracic expansion during quiet and deep breathing, and symmetry of respiration between left and right hemi thoraces. Assessment of fremitus: which is vibration perceptible on palpation" In subcutaneous emphysema: you must palpate the tissue, audible cracking sounds are heard – these sounds are termed Crepitation 184 185 Percussion of chest: Done to determine relative amounts of air, liquid, or solid material in the underlying lung, and to determine positions and boundaries of organs. Percussion done for posterior and anterior and lateral aspects of chest with all directions, and with about “5”cms intervals. Auscultation: To obtains information about the function of respiratory system & to detect any obstruction in the passages. Instruct the client to breathe through the mouth more deeply and slowly than in usual respiration and then to hold the breath for a few seconds at the end of inspiration to increase intrapleural pressure and reopen collapsed alveoli. Auscultate all areas of chest for at least one complete respiration: 12 anterior locations and 14 posterior locations Auscultate symmetrically: Should listen to at least 6 locations anteriorly and posteriorly 187 Breathe sounds: are analyzed according to pitch, intensity, quality, and relative duration of inspiratory and expiratory phases. Bronchial breathe sounds: are normally heard over manubrium of sternum If heard over lung tissue – indicate pathologic condition, these sounds “high-pitched loud sounds with decrease inspiratory and lengthened increase expiratory phases. Absent or decreased breath sounds can occur in: Foreign body. Bronchial obstruction. Shallow breathing. Emphysema 188 Breath Sounds Normal breath sounds are distinguished by their location over a specific area of the lung and are identified as tracheal, vesicular, bronchovesicular, and bronchial (tubular) breath sounds as the next: 1.Tracheal Very loud, high pitched sound Inspiratory = Expiratory sound duration Heard over trachea in the neck 2. Bronchial Loud, high pitched sound Expiratory sounds > Inspiratory sounds Heard over manubrium of sternum If heard in any other location suggestive of consolidation 189 3. Bronchovesicular Intermediate intensity, intermediate pitch Inspiratory = Expiratory sound duration Heard best 1st and 2nd ICS anteriorly, and between scapula posteriorly If heard in any other location suggestive of consolidation 4.Vesicular Soft, low pitched sound Inspiratory > Expiratory sounds Major normal breath sound, heard over most of lungs 190 Adventitious Breath Sounds An abnormal condition that affects the bronchial tree and alveoli may produce adventitious (abnrmal= addtional) sounds. Adventitious sounds are divided into two categories: discrete, noncontinuous sounds (crackles) and continuous musical sounds (wheezes) as the next: 1. Crackles (Rales) Discontinuous, intermittent, nonmusical, brief sounds. Heard more commonly with inspiration Classified as fine or coarse Its may associated with Prolonged recumbency Crackles caused by air moving through secretions and collapsed alveoli and associated with the following conditions: pulmonary edema, early CHF, and pnumonia 191 2.Wheeze Continuous, high pitched, musical sound, longer than crackles Whistle quality, heard during expiration, however, can be heard on inspiration Produced when air flows through narrowed airways Associated conditions: asthma, chronic bronchitis, and COPD 3. Rhonchi Similar to wheezes (subtype of wheeze) Low pitched, snoring quality, continuous, musical sounds Implies obstruction of larger airways by secretions Associated condition: acute bronchitis 192 4. Stridor Inspiratory musical wheeze Loudest over trachea Suggests obstructed trachea or larynx Medical emergency requiring immediate attention Associated condition inhaled foreign body 5. Pleural Friction Rub Pleural friction rubs are specific examples of crackles. Discontinuous or continuous brushing sounds It is a loud dry, cracking or grating sound indicating of pleural irritation, heard over lateral and anterior lung in sitting position that heard during both inspiratory and expiratory phases Occurs when pleural surfaces are inflamed and rub against each other Associated conditions as pleural effusion, Pneumonothorax Medical conditions associated with decreased or absent of breath sounds Asthma COPD Pleural Effusion: fluid accumulating within the pleural space Pneumothorax: caused by accumulation of air or gas in the pleural space. ARDS( adult respiratory distress syndrome) Atelectasis : is defined as a state in which the lung, in whole or in part, is collapsed or without air entery Five Main Symptoms of Respiratory Disease Cough Breathlessness Sputum Wheeze Pain Chapter (11) Head Assessment, face and neck Islamic University of Gaza Strip Assessment of the Head Inspects the size, shape, and contour of head. The skull is generally round with anterior & posterior prominences. Large infant's head may be hydrocephalus. Large adult's head & facial bones resulting of acromegaly. Palpates the skull for nodules or masses Assessment of the eye Assess external eye structures and pupils, visual acuity, ocular movements, Peripheral vision. Assessment of external eye structures: position and alignment of eyes, eye brow, eye lids, eye lashes, lacrimal glands, pupils and iris. Assessment of pupils done by using penlight which produce constriction of pupils to show accommodation and convergence of pupils. Assess internal eye structures e.g. iris , retina, macula etc Consider the following Factors: Age use of corrective lens, artificial eye, allergies, pain, visual disturbances Health related factors such increase Blood Pressure, or Diabetes mellitus Using the following equipment to assess the eyes: Eye chart (Snellen chart), Chart or newsprint. Cover card. Penlight, and ophthalmoscope Ask the client about history of previous eye surgery, trauma, use of corrective glasses or contact lenses, blurred vision, Diplopia, strabismus, recent changes in vision, date of previous vision test, allergies, eye redness, and frequent watering discharge 197 Assess Visual Acuity: Done by placing the client 20 feet from the Snellen eye chart and testing each eye alone. Assess extra ocular movements by asking client to hold his head and follow movements of your forefinger. Assess peripheral vision: “Visual fields” Hemianopsia: blindness of 1/2 field in one or both eyes. Quadrantanopsia: blindness of 1/4 of visual field in one or both eyes. Ascotoma: Island like blindness in visual field Ear Assessment Take history of ear surgery, trauma, frequent infection, ear pain, drainage, hearing loss, tinnitus, vertigo, ototoxic medications, and last hearing examination Assess client in sitting position & inspects the auricle’s placement, size, symmetry, and color. Redness: sign of inflammation or fever. Color of ears must be the same as of the face. Pallor: indicate frost bite. Palpate the auricles for texture, tenderness, and skin lesion. If client complains of pain: pull the auricle and press on the tragus and behind the ear over the mastoid process if pain increase, means external ear infection, if pain is not increase, means middle ear infection may be present. 199 Inspection the ear canal for size and discharge. Assessment of cerumen if it is yellow or green may indicate infection. Assessment of hearing acuity: done simply by identification of voice tones, with the client repeating testing words spoken by the nurse (whisper test) N.B: deeper structure and middle ear can be observed only by otoscope. Whisper Test (patient with normal acuity can correctly repeat what was whispered) Weber Test (uses bone conduction to test lateralization of sound by a tuning fork) Rinne Test (useful for distinguishing between conductive and sensorineural hearing losses) 200 Weber Test: A tuning fork, set in motion by grasping it firmly by its stem and tapping it on the examiner’s hand, is placed on the patient’s head. A person with normal hearing will hear the sound equally in both ears or describe the sound as centered in the middle of the head. In an abnormal patient, the sound is heard louder in one ear (lateralization). Rinne Test The examiner shifts the stem of a vibrating tuning fork between two positions: 2 inches from the opening of the ear canal (for air conduction) and against the mastoid bone (for bone conduction). Patient is asked to indicate which tone is louder or when the tone is no longer audible. Normally, sound heard by air conduction is audible longer and louder than sound heard by bone conduction. With a conductive hearing loss, bone-conducted sound is heard longer than air-conducted sound With a sensorineural hearing loss, air-conducted sound is audible longer than bone conducted sound. 202 The Otoscope Examination Using the Otoscope : Otoscope should be held in the examiner’s right hand, in a pencil-hold position, with the bottom of the scope pointing up. This position prevents the examiner from inserting the otoscope too far into the external canal. Choose the largest appropriate speculum Using the opposite hand, the auricle is grasped and gently pulled upper and back to straighten the canal in the adult, while pulled down and back in infant and child ( <3 age ) The External Canal : Redness / swelling / lesion / foreign body / discharge Tympanic Membrane : Color / character / perforation The healthy tympanic membrane is shiny, translucent , pearl-gray color 203 Cone-shaped light reflex 204 Assessment of the nose Functions of the nose 1. Identify odors (upper 1/3 of septum) 2. Air passageway (obligate in newborns) 3. Air conditioning: humidify, warms/cools air, cleans and filters air of dust and most bacteria and voice resonance Inspect and Palpate External Nose 1) Symmetric, in the midline, skin lesion, pain 205 Nostril patency: Inspect & observe symmetry, inflammation & deformity. In case of swelling or deformities of nose, the nose is palpated gently for tenderness, swelling and underlying deviations. Normally the external nose is symmetrical, strait, non tender, and without discharge. Assess mucosa which is normally pink in color. Yellowish or greenish discharge – means sinus infection. Pale mucosa with clear discharge – means allergy. For client with NGT, nurse should routinely checks for local breakdown of skin “Excoriation” of the nostril that characterized by redness and sloughing of the skin 206 Assessment of the sinuses Frontal and maxillary sinuses are examined for pain and edema. Palpate sinuses both frontal (below the eyebrow) and maxillary (below cheekbones) for tenderness, which verbalized by client during exam. Percuss sinuses for resonance which is normally hollow tone, and noting abnormality e.g. flat, dull tone elicited or expresses pain on percussion Transillumination sinusitis: is the transmission of light through tissues of the body. A common example is the transmission of a flash of light through fingers, producing a red glow. This is because red blood cells absorbed other colors of the beam and transmitted only the red component. Absence of light indicates mucosal thickening or the cavity is likely contain fluid or pus sinuses 207 208 Assessment of Mouth and pharynx 1. Assessment of oral cavity can be made during administration of oral hygiene. Lips – inspected for color, texture, hydration, contour, and lesions. Inner and buccal mucosa, Gums and teeth inspected for color, hydration, texture and lesions e.g. ulcers, abrasions or crusts. Tongue and floor of mouth can carefully inspect. Assessment of palate “soft and hard” by extending client’s backward, assessment for color, shape, texture, and extra bony prominences or defects 2. Assessment of Pharynx Assessment for pharynx done: by using tongue depressors. Pharyngeal tissues are normally pink and smooth. Edema, ulceration, or inflammation indicates infections or abnormal lesions 210 Assessment of Neck Assessment done by inspection and palpation that the client placed in a sitting position Assess neck muscles, trachea, thyroid gland, carotid arteries and jugular veins, cervical lymph nodes and cervical vertebrae. Assess neck size and position of trachea and thyroid Assess range of motion by asking the client to tilt the head backward and side to side Assess lymph nodes and venous distention. Normally: Neck should be symmetrical with full range of motion. No neck vein distention should be visible. Inspect and palpate cervical vertebrae Assess the posterior aspects of the neck for symmetry, tenderness, masses or swelling. Thyroid gland is assessed by palpation, observation and auscultation. Normal thyroid gland is not palpable. The isthmus is the only portion of the thyroid that is normally palpable Palpation – for gland itself. If enlargement of thyroid gland is detected, the area over the gland is auscultated for a bruit Bruit: vibrations sound of blood flow through arteries. In enlarged gland, heard with the diaphragm of stethoscope (This abnormal finding) 212 Trachea Trachea normally centered; (at the suprasternal notch) The cartilages should be smooth, non tender and move easily under examiner’s fingers when the client swallow Palpation done by placing the thumb and forefinger on each side of the trachea Assessment of the lymphatic system Lymphatic System consists of a network of collecting ducts, lymph fluids e.g. spleen, thymus, tonsils, adenoids--- etc Functions of lymphatic system Movement and transportation of lymphocytes Production of lymphocytes. Production of antibodies. Phagocytosis Absorption of fat and fat soluble substances. Enlargement of lymph node: provides early indication of infection or malignancy. Examination of lymphatic System : 2 steps Firstly inspection for enlarged lymph nodes, skin lesions and edema Secondly palpating gently the lymph nodes areas using pads of "2, 3, 4" fingers in gentle circular motion. Press lightly and then increasing pressure gradually. Move skin lightly over the under lying tissues & not moving the examining fingers over the skin. Large nodes due to malignancy are generally not tender vary in size, hard, asymmetrical Some Areas of lymph nodes Pre auricular: in front of the ear. Mastoid or posterior auricular – behind the ear. Above the mastoid process. Occipital – at the base of skull posterior. Parotid – near the angle of the jaw. Sub-mandibular – midway between angle of jaw and the tip of the mandible. Submentum – in the midline posterior to the tip of the mandible. Anterior superficial nodes – in the anterior triangle of the neck. Posterior cervical nodes – in the posterior triangle of the neck. Deep cervical nodes – very deep and difficult to be examine. Supra clavicular or scalene nodes – In the angle formed by clavicle and Sternocleidomastoid muscle. Axilla, breast & Lower extremity (inguinal and popliteal nodes) 215 Chapter (12) Assessment of the breast Islamic University of Gaza Strip Assessment of the breast The breasts, or mammary glands, are highly specialized glands, which extend laterally from edges of the sternum to the anterior axillary fold. They are located between the third and seventh ribs on the anterior chest wall. Each breast is divided into 15 to 20 irregularly shaped lobes separated by fibro elastic and adipose tissues. The areola is a roughened, segmented, circular formation, which surround the nipple. Subjective data Tenderness, pain, swelling, or change in size of breasts. Change in position of nipple or nipple discharge. Presence of cysts, lumps, and lesions. History of prior breast surgery 217 Female breast: Inspection: Best done in sitting position with arms relaxed at sides Carefully observe the breasts for symmetry. The normal breasts may be slightly different in size. If necessary, reassure the patient that any difference in size is normal. Inspect Areola and nipples for position, pigmentation, inversion, discharge, crusting & masses. Examine the breast tissue for size, shape, color, and contour Assess level of breasts, notes any retractions or dimpling of the skin. Ask client to elevate her hands over her head, repeat the observation. Ask client to press her hands to her hips and repeat observation. Inspect the axilla for: rashes, signs of infection and unusual pigmentation 218 Palpation: Best done in recumbent position: Raise the arm of client on the side of the breast being palpated above client’s head. Palpate the breast from less painful or less diseased area (Use on palpation palmer aspects of the fingers in a rotating motion, compressing the breast tissue against the chest wall, this is done quadrant by until the entire breast has been palpated. Note skin texture, moisture, temperature, or masses. Gently squeeze the nipple and note any expressible discharge. "Normally not present in non lactating women". Repeat examination on the opposite breast & compare findings. If mass is palpated, its location, size, shape, consistency, mobility and associated tenderness are reported Remember the breast may feel slightly more fibrotic or be somewhat tender just prior to or during the menses. Male Breast: Examination of male breast can be brief and should never be omitted. Observe nipple & areola for ulceration, nodules, swelling or discharge Instruct the patient to raise both arms, exposing the skin of the axilla. Carefully inspect the axilla for: rashes, signs of infection and unusual pigmentation Palpate the areola for nodules or tenderness 220 Chapter (13) Assessment of Cardiovascular System Islamic University of Gaza Strip Anatomy of the Heart Right Atrium Right Ventricle Left Ventricle Left Atrium Superior and Inferior Vena Cava Pulmonary Artery Pulmonary Vein Aorta TWO PUMPS Right side pumps blood to lungs Left side pumps blood to body FOUR VALVES Two Atrioventricular Valve (AV) Tricuspid Valve (right atrioventricular valve) Mitral (left atrioventricular valve) Two Semilunar Valve (SL) Aortic valve (left semilunar valve) Pulmonary valve (right semilunar valve) Subjective data: 1. Assessment of chief complaints: Chest pain: location, quality, duration & associated symptoms. Irregular heart beat: too fast, jump etc. 223 2. Assessment of risk factors: Ask about history of hypertension, diabetes, and rheumatic fever Ask about family history of heart attack, hypertension, stroke, and diabetes Describe your nutritional intake: high cholesterol, triglyceride level. Do you smoke? How much? And for how long? How do you view yourself? What do you do to relax? How many hours a day do you work? How do cope with stress. Exercise: what do you do for exercise? How often? Pain in calves, feet, buttocks or legs? What aggravates the pain (walking, sitting long periods, standing long periods, sleep) what relieves the pain “elevating legs, rest, lying down”. In what type of chair does client usually sit? Does he/she cross legs frequently? 224 Inspection: Assessment the client must be is in supine or sitting positing according to his health By inspection and palpation you may detect ventricular hypertrophy. Use source of light to inspect subtle movements in chest e.g.: pulsation, retraction etc. Apical pulse in left fifth intercostal space, if deviation in site observed may indicate cardiac enlargement 6th intercostal space. Retractions may be seen around site of apical pulse, marked retraction may indicate pericardial disease. 225 Palpation (supine position) Palpate from apex, moving to external border to base Detect abnormalities in site of palpation and abnormal sounds especially for thrill “abnormal flow of blood” Describe in terms: locations of pulsation in relation to mid-sternal, mid-clavicular or axillary lines. Palpation of apical pulse, strength differs from thin person to obese. Conditions such as anxiety, anemia, fever, and hyperthyroidism may increase in force and duration of apical pulse (you feel lifting sensation under your fingers). Palpation of pulse at base of the heart (putting your hand at second left intercostal spaces at sternal borders). Percussion: “not used in cardiac assessment” Auscultation: All heart sounds are generally low pitched “low frequency” and difficult for the human ear to hear. Auscultation can be started from base to apex or from apex to the base. Assess: Rate and rhythm of the heart beat. Concentrates initially on sound "1", noting its intensity and variations, possible duplication and effects of respiration. Sound 1 caused by the closing of the tricuspid and mitral valves. Systole begins with Sound "1" & extends to Sound "2" Then listen to Sound "2" for same characteristics. Sound "2": results from closing of the aortic & pulmonary valves Diastole begins with Sound "2" and extends to next Sound "1" Sound "2" louder than Sound "1" at the base of heart, and is lighter than Sound "1" at the apex. Finally listen for extra sounds and for murmurs Sound "3": During diastole, rapid filling and distention of ventricles occur causes vibrations of ventricular walls" and this known as sound "3" ". Sound "3" best heard at the apex with bell of stethoscope. Its indicate Pathological alterations in ventricular filling in early diastole. it represents a normal finding in children Sound "4": occur after Sound "3" (late diastolic filling), occur from vibrations of ventricular wall or vibrations of the valves. It’s usually associated with cardiac disease, often that with altered ventricular compliance Gallop Sound: a gallop characterized by the superimposition of abnormal third and fourth heart sounds, usually indicative of myocardial disease. Heart murmurs (abnormal sounds produced by vibrations within the heart or in the walls of large vessels “during systole or diastole”. Murmurs occurrence result from valve defects, changes in the blood vessels or an increased flow of blood through a normal structure (eg, with fever, pregnancy, hyperthyroidism). Special maneuvers for vascular assessment Check for deep phlebitis by quickly squeezing calf muscles against tibia (normally no pain) Check Homan's sign by extending leg and dorsi-flexing foot (normally no pain). 229 Arterial and venous insufficiency of lower extremities 230 Chapter (14) Assessment of the abdomen Islamic University of Gaza Strip Assessment of the abdomen The abdomen is the largest body cavity that extends from the diaphragm inferiorly to the inlet of the true pelvis. Its contents are partially protected: Superiorly by the lower ribs. Posterior by the lumbar vertebra. Laterally by the iliac bones Abdomen Regions Divisions of the abdomen Four Quadrants. Nine regions. Locating Abdominal Structure By Quadrant 1. Right Upper Quadrant (RUQ) Ascending and transverse colon Duodenum Gallbladder Liver , head of pancreas Right of adrenal gland The small intestine or ileum in all quadrant Right kidney (upper pole) and right ureter 2. Right Lower Quadrant (RLQ) Appendix Ascending colon , Cecum Right kidney lower pole Right ovary and tube, right ureter, and right spermatic cord 233 3. Left Upper Quadrant (LUQ) contains of: Left of adrenal gland Left kidney (upper pole) Left ureter Pancreas (body and tail) Spleen Stomach Transverse ascending colon 4. Left Lower Quadrant (LLQ) contains of: Left kidney (lower pole) Left ovary and tube Left spermatic cord Sigmoid colon 5. Midline Balder , Uterus , Prostate gland Assessment Procedures Subjective data: ask the client about: Nutritional history: appetite, weight loss or gain. Gastro intestinal symptoms: dysphagia, nausea, vomiting, and indigestion. Bowel habits: pattern, and stool characteristics. Pain: location, quality, pattern, and relationship to ingestion of food. Use of medications: Aspirin, Anti inflammatory drugs, and steroids. Gastro intestinal diagnostic tests and surgeries. The client is placed in the supine position, with small pillows under the head and knees. The abdomen is exposed from the breast to the symphysis pubis Start assessment with inspection, auscultation, then percussion and palpation. Stand the client right side and carry out assessment systematically, beginning 235 with the left upper quadrant.The bladder should be empty. Inspection: Under source of light you see exactly changes in contours. Assess the presence or absence of symmetry, distention, masses, visible peristaltic waves and respiratory movement. Inspect the abdominal skin for pigmentation e.g. jaundice, lesions, striae scars, dehydration, general nutritional status and condition of umbilicus, this give information about general state health Contour of the normal abdomen is described as: flat, rounded, or scaphoid. Normally contour is description of the profile line from the rib margin to the pubic bone. Flat contour seen in the muscularly competent and well nourished individual. Rounded abdomen: Normally in infant and toddler, but in the adult caused by poor muscle tone and excessive Subcutaneous fat deposition. Scaphoid contour “Concave in horizontal line” seen in thin clients of all ages. Inspect for respiratory movements especially for retraction of the abdominal wall on inspiration which is called "Czerny's sign “associated with some Central Nervous System diseases such as chorea” Auscultation: Auscultate peristaltic sounds which are normally high pitched. Listen for at least "5" minutes before concluding that no bowel sounds are present. "Peristaltic sounds may be quite irregular". Duration of single sound may be less than a second or more than it. Stimulation of peristalsis may be achieved by flicking the abdominal wall with a finger “direct percussion Auscultate vascular sounds: Loud bruits detected over the aorta may indicate presence of an aneurysm; the aorta is auscultated superior to the umbilicus Listen for Peritoneal friction rub over the area of liver and spleen e.g. spleen infection, abscess or tumor: best heard over the lower rib cage in the anterior axillary line. (rough grating sound like sound of two pieces of leather being rubbed together). 237 Percussion: To detecting fluid or gaseous distention and masses and assessing solid structures within the abdomen. Percussion of one for each quadrant to assess areas of tympany and dullness. Potentially painful areas are always Percuss last Percussion allows you to identity borders of the liver to detect organ enlargement. To detect liver size, start percussion at the right iliac crest and proceeds up ward on the right mid-clavicular line, when dullness occur this is the lower border of the liver. To detect upper border of the liver percuss, down from the nipple along mid-clavicular line, then dullness occur “upper border” may be found in (5,6,7) intercostals space, distance between points lower and upper is (612cm). Diseases e.g. cirrhosis, cancer, and hepatitis cause liver enlargement Stomach position: With percussion you can locate the tympanic air bubble of the stomach by percussing over the left lower anterior rib cage. Kidney Tenderness: In sitting or erect position, use direct or indirect percussion to assess for kidney inflammation. Use ulnar surface of the partially closed fist and percuss the costo-vertebral angle at the scapular line. If the kidneys are inflamed, client feels tenderness during percussion Palpation: Detect abdominal tenderness and noting the quality of abnormal distensions or masses. During palpation assess for muscular resistance, distention, tenderness and superficial organs or masses. Assess for distended bladder if client has inability to void (Bladder lies normally below the umbilicus and above symphysis pubis). In deep palpation depress hands (2.5-7.5 cm), "1-3 inch" Deep palpation never used over a surgical incision or tender organs, or masses. If tenderness present, check for rebound tenderness, if it was positive indicated peritoneal irritation e.g. appendicitis 239 Palpation of liver: Right upper quadrant under the rib cage Place your left hand under client’s posterior thorax at the 11th and 12th ribs and by your right hand palpate in and up to feel the liver’s edge as the client inhales. G.B normally not felt and if distended it felt under liver and may indicate cholecystitis. Palpation of spleen: Generally not palpable in normal adult person, but in case of spleen enlargement you can palpate it below costal margin. 240 Assessment of the anus and recto sigmoid region Events required rectal examination: Abdominal pain Alternation in bowel habits. Anal pain, anal spasm. Anal itching or burning. Black tary stool. Rectal bleeding. Positions for rectal examinations: Left lateral or SEM's position. Knee- chest position Standing position, most common use for prostate gland examination. Lithotomy position Squatting position. In all positions, before examination wear two gloves Inspection: Spread buttocks carefully with both hands to examine the anus and skin around it which is more pigmented, moist, and hairless. Assess lesions, scars, or inflammation, peri-rectal abscess, fissures, piles, fistula opening, tumor and rectal prolapsed. Ask the client to strain down ward as in defecation. Inspect for pilonidal sinus or cyst at the sacro- coccygeal area, and give description Palpation: (PR examination) Spread the buttocks apart with your non dominant hand. Gloved index gently placed against the anal verge, and with firm pressure in direction of umbilicus as the rectal sphincter relaxes. Ask client to lighten the sphincter around your finger to examine muscle strength. Mucosa of the anal canal is palpated for tumor or polyps. Assess normal cervix in female which felt as small round mass during P.R examination 242 Common diseases can be detected during rectal examination: Pilonidal cyst or sinus. Pruritus anus Rectal tenesmus:. Fecal impaction Anal fissure Fistula in anus Hemorrhoids: External painful & internal painless unless complicated. Rectal polyps Rectal prolapse: e.g. in case of internal hemorrhoids Anal incontinence. Abscesses or masses e.g. Ischio rectal abscess, peri rectal obstruction 243 Chapter (15) Assessment of musculo-skeletal system Islamic University of Gaza Strip The primary structures of the musculoskeletal system are the bones, 245 muscles, cartilage, ligaments, tendons and joints. The bony skeleton provides a sturdy framework to support body structures. The bone matrix stores calcium, phosphorus, magnesium and fluoride. In addition, the red bone marrow located within bone cavities produces red and white blood cells in a process of hematopoiesis. There are 206 bones in the human body, divided into four categories. Long bones (eg, femur) Short bones (eg, metacarpals) Flat bones (eg, sternum) Irregular bones (eg, vertebrae) Assessments are made of muscles, bones and joints. When assessing the musculoskeletal system keep in mind that injury or inflammation of any part of the system can cause pain, stiffness, or an alteration in motor strength or mobility. Musculoskeletal assessment is conducted from head to toe with 246 inspection and palpation Assessment of musculo-skeletal system done firstly when the client walks, moves in bed or performs any type of physical activity. The nurse usually assesses the musculoskeletal system for: Muscle – size, contractures, tremors, muscle tonicity, smoothness of movement and muscle strength. Bones – skeletal structure, tenderness, edema Joints – swelling, tenderness, smoothness of movement, crepitation, nodules, range of motion. Terms used to describe joint movement: Flexion – bend that decrease angle between bones Extension – straightening a limb to increase the angle of joint Abduction – moving a limb away from the body’s midline Adduction – moving a limb towards the body or beyond it Internal rotation – turning a body part towards midline External rotation – turning a body part away from midline Circumduction – circular movement of a body part Supination – turning the palm upwards Pronation – turning the palm downwards Inversion – turning the hand or foot inward Eversion – turning the hand or foot outward 247 Musculoskeletal Assessment Subjective data: Observer gait and posture as client walks into room. Normally the client walks with arms swinging freely at sides and the head and the face leading the body. Pain: assess pain at rest, with exercise, changes in shape or size of an extremity, changes in mobility to carry out activities of daily living, sports, and works. Stiffness of joint Decreased or altered or absent sensations. Redness or swelling of joints. History of fractures and orthopedic surgery. Occupational history 248 Objective data Determine range of motion, muscle strength and tone, joint and muscle condition. Muscle problems commonly are manifestations of neurological disease, so you must do neurological assessment simultaneously. Joints vary in their degree of mobility, range from freely movable e.g. knee, to slightly movable joints e.g. the spinal vertebra. During assessment of muscle groups: assess muscle weakness, or swelling, and size, then compare between sides. Joints should not be forced into painful positions. Loss of height is frequently the first clinical sign of osteoporosis. Small amount of height loss expected with aging. Ask client to put each joint through its full range of motion, if there is weakness, gently supporting & moving extremities through their Range of motion, to assess abnormalities. Normal joints are non tender, without swelling and move freely. In elderly joints often become swollen & stiff, with reduced range of motion, resulting from cartilage erosion and fibrosis of synovial membranes 249 Chapter (16) Assessment of Neurological system Islamic University of Gaza Strip Assess this system when doing physical examination e.g. cranial nerve function can be testing during the survey of the head and neck. The neurological assessment consists of six parts: (mental status, cranial nerves, sensory functions, motor function, cerebellar function, reflexes). Subjective data: Loss of consciousness, dizziness, and fainting. Headache: precipitating factors and duration. Numbness and tingling or paralysis or neuralgia. Loss of memory, confusion, visual loss, blurring, and pain. Facial pain, weakness, twitching, speech problems e.g. aphasia. Swallowing problems and drooling. Neck weakness or spasm 251 Mental and emotional Mental and emotional status is observed as the nursing history is collected, and by simply interacting with client, e.g. “Nursing care plan” Level of consciousness Level of consciousness ranges from full a wakening, “alertness” to unresponsiveness to any form of external stimuli. Alert client responds to questions spontaneously. Assess level of consciousness by using Glasgow coma scale 252 Glasgow coma scale 253 Assessment of behavior and Appearance Behavior, mood, hygiene, grooming and choice of dress reveal pertinent information about client’s mental status. Appearance reflects how a client feels about the self. Personal hygiene such as unkempt hair, a dirty body, or broken, dirty fingernails should be noted. Language: Assess ability of individual to understand spoken or written words & how he speak or writes. Assess intellectual function, which includes: memory “recent, immediate, past”, knowledge, abstract thinking, association and judgment. Assess for sensory function: Assess sensitivity to light touch “cotton” Assess sensitivity to pain “pinprick” Assess sensitivity to vibrations “tuning fork” Assess sensitivity to positions. Don’t forget comparing both sides of body 254 Chapter (17) Assessment of Urinary System Islamic University of Gaza Strip The main function of urinary system is regulation of the fluid and electrolytes composition of the body fluids and removal of metabolic end products from the blood Nursing History: Normal voiding pattern and frequency (oliguria – urinary urgency – poyluria – anuria - dysuria –hematuria - enuresis) Appearance of the urine, urine culture and any recent changes (amount – color). Normal colure yellow-straw Family history of kidney problems (polycystic kidney and all types of hereditary nephritis are genetically transmitted, kidney and bladder calculi The present illness such as pain or burning sensation, UTI, an ostomy. Past history and current problems with urination: (syphilis, gonorrhea, sexual transmitted disease STD) DM and HTN . Factors influencing the elimination pattern Medications: Diuretics, Psychotropic agents , Anti-hypertensive 256 Medical Terms related to urinary system Dysuria: painful or difficult voiding Hematuria: red blood cells in the urine Urgency: strong desired to urinate due to inflammation in bladder , prostate , urethra Polyuria: abnormal large volume of urine voided in given time = 2500ml Oliguria: small volume of urine between 100-500 ml Anuria: absence of urine in bladder less than 50 ml Enuresis: involuntary voiding during sleeping. 257 Physical Assessment of Urinary System Inspection Inspection including examination of abdomen and urethral meatus. Auscultation including renal arteries Percussion includes the kidneys to detect tenderness Palpation to detect any mass, lumps, tenderness Percussion of the kidney To detect areas of tenderness by costovertebral test, normally will feel a thudding sensation or pressure but not tenderness Palpation of kidney Contour, size, tenderness, and lump. In adult normal the kidneys not be palpable because of their location deep with abnormal. Elderly the right kidney is slightly lower than the left, it may be easier to palpate 258 Percussion of the bladder Percuss the area over the bladder (5cm) above the symphysis pubis. To detect difference in sound, percuss toward the base of the bladder. Percussion normally produces a tympanic sound Palpation of bladder Normally feel firm and smooth. In adult bladdre may not be palpable Inspection of the urethral meatus Look for swelling, discharge and inflammation Assessment of Urine Urine assessment includes: Measure volume of urine Inspect colour, clarity, and volume Test the specific gravity, glucose, ketone bodies and blood and pH Normal urine volume 1-2 litter per 24 hours (normal adult) 259 Color: typically yellow-straw but varies according to recent diet and 260 concentration of the urine. Drinking more water generally tends to reduce the concentration of the urine and therefore cause it to have a lighter color. (The converse is also true.) Smell: Generally fresh urine has a mild smell but aged urine has a stronger odor, similar to that of ammonia. The smell urine may provide health information. For example, urine of diabetics may have a sweet or fruity odor due to the presence of ketones. Acidity: PH is a measure of the acidity ( or alkalinity0 of a solution. PH is a measure of the activity of hydrogen ions (H+) in a solution 95% Water, 5% chemical solutes. Urea from breakdown of amino acids (protein) to give ammonia + C02 giving urea and creatinine from breakdown of creatine phosphate in muscle Collection of urine samples All urine tests are ideally performed on fresh specimemens: Urine container has been adequate protection agonist bacterial contamination and chemical deterioration Identification or labeled should be provided. The patient should then be gowned for the physical examination Bring it into the dry room Urine specimens should collect from the patient means of the clean –catch midstream technique. All specimens should be refrigerated as soon as possible they are obtained . to avoid shifted the PH of urine to alkaline because contamination of ureasplitting bacteria from the environment Consider the Developmental Stages Pediatric: difficulties, crying, change in urinary in childhood). Pregnant: Pain during urination, normal increase urine in volume and frequency and decrease urine specific gravity Elderly: how much and how type of liquid do you drink in the evening? do you ever lose of control of your bladder 261 The End 262