Transgender Health:
Tools to Providing Health Care and
Advocacy on College Campuses
Learning Objectives
• To define basic terminology
• To describe the risks to
transgender students by not
having access to supportive
healthcare
• To identify strategies for
providing transgender
inclusive healthcare and
advocacy on campus
Building the Context: Introductions and
Guidelines
• Davis Smith MD, Wesleyan University
pdsmith@wesleyan.edu
• Heather Eastman-Mueller, Ph.D., CHES,
University of Missouri,
EastmanMuellerH@health.missouri.edu
• Alexandra Hall MD, Cornell University
amh89@cornell.edu
• Joleen Nevers MAEd, CHES, University of
Connecticut joleen.nevers@uconn.edu
Epidemiology
• Worldwide estimated incidence:
– Female to male (FTM) transsexual: 1 in 100,000*
• Tend to present in teen years
– Male to female (MTF) transsexual: 1 in 30,000*
• Tend to present in 20-30s
• Newer estimate, based on number of male-to-female
surgeries performed per male US population:
– 1 in 2,500 (Conway, L.)
–
•
Note. These are individuals who can afford and choose surgery
*American Psychological Association (2009)
Primary Source of Medical Care for
Respondents
Healthy Campus 2010: Obj. 1
(Access to Quality Health Care)
• To increase the proportion of insured persons and college
students with coverage for clinical preventive services (1.2)
– 19% lacked any health insurance compared to 17%
– 51% had employer-based coverage compared to 58%
• To reduce the proportion of college students that experience
difficulties or delays in obtaining health care. (1.6)
– 28% of sample faced harassment in medical settings; 2% were
victims of violence in doctor’s office
– 50% of sample reported having to teach their medical
providers about transgender care
HC 2010: Obj. 13
(HIV/AIDS/STD Prevention &
Treatment)
• To reduce the number of
cases of HIV infection
among adolescents and
adults. (13.5)
• Transgender/gendervariant respondents had
four times the national
average of HIV infection
HC 2010: Obj. 15
(Injury and Violence Prevention)
• To reduce the annual rate of rape or attempted rape. (15.35a)
– 3% of college student respondents reported experiencing
sexual assault by another student, faculty or staff
• To reduce physical fighting among college students. (15.38)
– 35% of college student respondents reported harassment and
bullying by students, staff or faculty
– 15% reported having to leave school “because the harassment
was so bad” (includes all levels of education)
HC 2010: Obj 18
Mental Health
• To reduce the rate of suicide attempts by adolescents and college
students. (18.2)
– 41% of respondents reported attempting suicide, compared to
1.6% of general population
• To increase the number of persons seen in primary health care
who receive mental health screenings and assessment. (18.6)
– 75% of respondents received counseling related to their GI/GE
– Additionally, 14% had hoped to receive it someday
HC 2010: Obj 26/27
Substance Abuse
• To increase the proportion of adolescents and college students
not using alcohol or illicit drugs during the past 30 days. (26.10)
– 8% of respondents reported currently using alcohol or drugs to
cope with mistreatment, compared to 7.3%
• To reduce tobacco use by adolescents, young adults and college
students. (27.1.2)
– 30% of sample reported smoking daily or occasionally,
compared to 20.6% general population
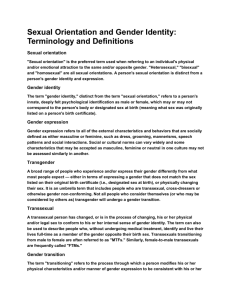
Diagram of Sex and Gender
Biologic Sex (anatomy, chromosomes, hormones)
male
female
Intersex
Gender Identity (Sense of Self)
man
Two spirit/third gender
woman
Gender Expression (Communication of Gender)
masculine
Androgynous
feminine
Sexual Orientation (Erotic Response)
attracted to
women
Bisexual/asexual/pansexual
attracted to
men
Gender Identity
• Internal sense of self as male or female, masculine or
feminine, something in-between or something other
• May or may not be outwardly expressed or apparent
• Only the individual can say for themselves, cannot be
“measured”
Gender Expression
• Appearance
– Dress/Clothing
– Hairstyle
– Make-Up, Jewelry
• Behavior
– Posture & Body
language
– Tone & pitch of voice
– Assertive vs passive
• Roles
– Career / Work
– Family
– Relationships
– Act
– Behavior
– Time/culture
dependent
Sexual Orientation / Attraction
To whom are you attracted?
men
both
women
neither
transmen
androgynous
genderqueer
neutrois
transwomen
“TRANS” or Transgender
Other terms: gender variant, gender non-conforming (GNC),
gender queer
Gender identity and/or gender expression can
differ from the conventional gender expectations
for biological males and females
Contrasts with “cisgender” which represents someone whose
GI/GE is congruent with sex assigned at birth
Transition
• A never-ending, complex process by which a transgender person
begins to live more fully as their true gender, which may include
any combination of the following:
–
–
–
–
–
Social gender roles
Alterations to dress
Legal name change
Changing preferred pronouns
Hormone therapy or sex reassignment therapy
*Not a discrete time period and varies according to person
Transsexual
• Can be a subset of transgender who live or wish to live full
time as members of the gender opposite to their natal sex
• Often, but not always seek medical intervention, such as
hormones and/or surgery
– Female-to-male (FTM): biological females who wish to
live and be recognized as men
– Male-to-Female (MTF): biological males who wish to live
and be recognized as women
Cross Dresser
• A person, regardless of motivation, enjoys dressing clothes or
makeup, of another sex; this may or may not accompany a
degree of exploration into gender identity
• Used to be termed “Transvestite”- currently seen by many as an
offensive term
Transforming Healthcare Video
Transforming your Health
Center
A primer on interventions physical and metaphysical to
better meet the needs of transgender and other students.
The Gender Challenge
• Review every form, questionnaire, process, procedure etc.
– Do you really need to know?
– Can you substitute Gender: _______
The Unshackling of Gender Bonds
• In place of forcing students into a gender binary, allow them to
define themselves.
– Patient-centered care model
• This generates a shared language, including:
– Gender
– Name
– Pronoun
The Gender-Blind Advantage
• We came to realize that a gender-specific structure for a health
assessment was more restrictive than informative.
– To the appeal for consumers
– To our ability to deliver personalized services
• This was especially the case for sexual health screening.
You Tell Me. I’ll Listen.
• In our sexual history-taking, we make no assumptions about
partners or practices.
– We let students define their risks.
• We then match the testing and counseling to their risks.
Clinic Paperwork
• About the Sexual Health Visit
• Pre-Visit Survey
• Visit documentation form
© 2011 P. Davis Smith MD
Role of your Website
• Often a first point of contact
– Scanning for safety
• Opportunity for transparency
Website Content Examples
•
•
•
•
Our Statement on Hormone Therapy
Trans resource list
Visit paperwork
Visit Descriptions
– See next slide
Better for Some Can Be Better for All
• Posting visit descriptions improved efficiency for clinician and
student
– Right patient to right appointment
– Common expectations of appointment intent and content
Targets for Gender-Neutralization
• Preferred name
– Process for legal change
• Room assignment
• Bathrooms
• Locker rooms
• Forms
Partners in the Inclusion Process
•
•
•
•
•
•
•
•
•
Health center staff
Counseling center staff
Health promotion
Registrar
Athletics
Residential life
Administrative leadership
LGBTQ Resource Center
International Center
What Do We Stand to Gain by
Responding to the Needs of this SubPopulation?
• You never know who’s paying attention to what
• Decreased barriers to care
– Appointment literature does not presuppose anything
about sexual habits
– Providers trained to broader range of sexual identity
dynamics
– Health Center recognized as “for us, too”
• Intellectual challenge
• Opportunity to display responsiveness
Lesson #1
• The product is key.
– First rule of Marketing: Deliver on the promise with a first-rate
product.
• Every patient visit is an act of public health
Lesson #2
• Process is a product, too.
– To be a campus institution actualizing transparency and
responsiveness is to be credible and appealing.
Lesson #3
• Barriers to care hold everyone back.
Primary Care
for Transgender Students
Routine Medical Care
• Transgender students get the same illnesses as the rest of our
students
• Be sensitive to the possibility of fear of disclosure or discrimination
– patients may have a heightened level of anxiety when seeking
medical care
• As with all students, listen supportively and with acceptance, not
judgment
• Try to do your best regarding name and pronoun – if unsure, ask
the patient (don’t assume). Alert nursing and front desk staff so
that everyone uses the correct name/pronoun.
• Don’t be intrusive – if it isn’t relevant to the problem for which they
are presenting, don’t ask about transition-related medical
procedures nor about sexual health.
Take care of the anatomy
• If they have a natal vagina
– Can get vaginitis just like everyone else
– If on testosterone, will get atrophy, which can then increase
their overall risk for vaginitis
• Consider add-back vaginal estrace cream if
recurrent/problematic
– Don’t assume they aren’t using it, or don’t want to
• May require lubricant
• May need contraception
• Remember to screen for GC and CT if indicated
Take care of the anatomy
• If they have a neo-vagina
– Can get vaginitis, just like everyone else
– Need post-op dilations to maintain patency
• Often not needed later on if sexually active
– Will likely require lubricant, but not always
– Are unlikely to have a neo-cervix, but if they do, they need
paps
Take care of the anatomy
• If they have a cervix
– Pap according to guidelines
• Age 21-19, every two years
• Age >30, every 3 years IF have had 3 consec. normals
– In transmen on T, expect ASCUS or no transformation zone,
or unable to interpret due to atrophy, etc. Consider checking
for high-risk HPV as a screening test.
Take care of the anatomy
• If they have a uterus and ovaries
– Some potential for increased risk of endometrial hyperplasia in
transmen on testosterone IF prior history of PCOS
• Any vaginal bleeding after amenorrhea on testosterone
needs to be evaluated, just like post-menopausal vaginal
bleeding (PUS, EMB)
– Unclear possible increased risk of ovarian CA in transmen on
testosterone
• Endocrine Society recommends consideration of hyst/BSO
due to unclear but potential risk
• Consider annual pelvic/bimanual exam
• Low threshold for PUS if develops any symptoms
Take care of the anatomy
• If they have breasts
– Screen as for any woman with breasts, i.e. mammograms
starting at either 40 or 50
– Breast exam as part of annual exam
– Consider full breast exam before chest reconstruction surgery
in FTMs
• If they have a prostate (all MTFs)
– Routine screening (DRE and PSA starting at age 50)
Be aware of ancillary services
• Be aware of potential insurance problems, depending on the
gender on the insurance company’s records. Be proactive with
insurance companies about this, and let the patient know that it
might come up.
• Prepare your staff and radiology technicians in advance, as well
as consultants, when necessary
– (yes, this is a man, but he does have a uterus and ovaries and
needs a PUS, don’t think it’s the wrong patient…)
Know your hormones
• We prescribe hormones every day – we know this stuff!
• Risks of estrogen
– Thromboembolic disease
– Elevated BP
– Elevated LFTs, gallbladder disease
– Migraine concerns
– Hyperprolactinemia
– Changes in lipid profile
• Recommended monitoring for transwomen on estrogen
– Recheck visit with vitals and weight Q 3 mo for first year, then Q6-12
months
– Serum testosterone and estradiol Q 3 months
– If on spironolactone, electrolytes Q 3 months for first year
– Q 3-6 month liver enzymes, lipids, prolactin for first year, then
annually
Know your hormones
• Risks of testosterone
– Elevated LFTs
– Polycythemia
– Male cardiovascular status
– Vaginal atrophy
– Changes in lipid profile
• Recommended monitoring for transmales on testosterone
– Recheck visit with vitals and weight Q 3 mo for first year, then
Q6-12 months
– Serum testosterone Q2-3 months til in normal male range
– CBC, LFTs, lipids Q 3 mo for first year, then Q6-12 months
Panel Discussion
• Questions for us?