Phases of Drug Action
Stressors Requiring Medication
Phases of Drug Action
NUR101 Fall 2008
Lecture # 11 & 12
K. Burger, MSEd, MSN, RN, CNE
PPP by Sharon Niggemeier RN, MS
(J. Garnar & R. Kolk) Rev kburger06,07
Three Phases of Drug Action
I. PHARMACEUTICAL PHASE
II. PHARMACOKINETIC PHASE
III. PHARMACODYNAMIC PHASE
I. PHARMACEUTICAL
PHASE
• A solid drug (tablet) has to disintegrate before it can be absorbed
• The process where a solid (tablet) goes into solution is known as dissolution
• ALL drugs must be in solution to cross biologic membranes
II. PHARMACOKINETIC
PHASE
• What the body does to the drugrefers to the study of how the body processes drugs
• It includes the 4 basic components of :
1# Absorption
2# Distribution
3# Metabolism (Biotransformation)
4# Excretion
#1 ABSORPTION
• Movement of a drug from the site of administration into the bloodstream .
• Absorption determines how long it takes for a drug to take effect.
• Usually the more rapid the absorption, faster the drug works
• Drugs can be absorbed through plasma membranes by various methods but primarily by: Diffusion (lipid soluble molecules) & Active transport (protein bound or water soluble molecules)
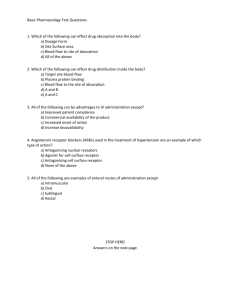
Factors Affecting Absorption
• Surface area
• Contact time with surface
• Circulation
• Solubility (water soluble vs lipid soluble)
• Ionization (weak versus strong acid/base)
• Drug form & drug concentration
• Bioavailability ( after first pass thru liver)
• Route of administration (enteral & parenteral)
• Additives : alter the location of disintegration of drugs as well as increase or decrease the rate of absorption
• Enteric coating allows a drug to dissolve only in an alkaline (pH greater than 7.0) environment such as the small intestine.
•
Sustained release drugs: allow drugs to be released slowly over time, rather than quickly, like conventional tablets. SR, LA
•
Size of drug particles: smaller the particle, faster the onset. Ex: The generic drug Glyburide has trade names Micronase and Glynase. Glynase
(micronized) onset is faster than Micronase (nonmicronized)
Drug Absorption varies by form
Liquids, elixirs, syrups
Suspension solutions
Powders
Capsules
Tablets
Coated tablets
Enteric-coated tablets
Fastest
Slowest
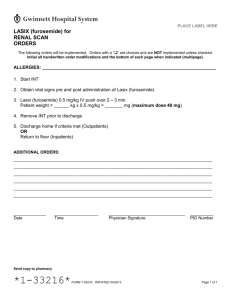
Look at your Lasix Drug Guide
• Is this drug available in more than one form?
• Which will have the fastest absorption?
• What is the absorption rate for the oral tablet form?
Absorption:
ENTERAL ROUTES
Mucous membranes of the mouth:
• Buccal or Sublingual forms of drugs
• Highly vascular absorbing surface
• Avoids first pass phenomenon that occurs in the liver
• Absorptive area is small therefore…
• Only small amounts of drugs can be given
Absorption:
ENTERAL ROUTES
•
Oral Route: Stomach
• Has low pH (about 1.4) the rate of gastric emptying & pH changes will affect how fast or how slow meds are absorbed.
• Has rich blood supply
• Susceptible to first pass phenomenon
• Lipid soluble substances and those that are relatively nonionized are well absorbed here.
CONSIDER THIS…
• Alcohol is extremely lipid soluble
• Aspirin is a very weak acid
• Both are well absorbed in the stomach.
Absorption:
ENTERAL ROUTES
•
Oral Route: Small Intestines
• Most important site for absorption of oral drugs as it has extensive absorptive surface due to many villi.
• Peristalsis and mixing encourage dissolution of drugs.
• Highly vascular and has a pH of 7.0 to 8.0
In what way will diarrhea affect absorption?
Why?
Absorption:
ENTERAL ROUTES
•
Mucus Membranes of the Lower Intestine:
Rectal Route
• Avoids most first pass effects in the liver
• Has extensive vascularity.
• Limited surface area
• Drugs need to be in solution or absorption is erratic and unpredictable.
Absorption: Other Routes
•
PULMONARY: Lungs
• Gases or aerosols can be delivered by this route.
• Rapid absorption occurs due to large surface area, rich blood supply and high permeability of the alveolar membrane.
• Provides a local effect ( ex: bronchodilation ), but may also produce unwanted systemic effects ( ex: sympathetic nervous system stimulation)
Absorption: Other Routes
•
TOPICAL ROUTE: Epidermis is low in lipid and water content, so it is a barrier to absorption.
• Dermis allows rapid absorption therefore:
Abraded skin could allow an overdose of the drug so only use intact skin.
• Effects are usually local
• Lipid soluble drugs can penetrate lipid bylayers of the epidermal cells.
Critical Thinking Questions
A client has an order for Benadryl ointment for an itchy rash on his arms. To promote absorption of the drug, the nurse should:
A. Apply an ice pack to the arms after application
B. Wash the area with mild soap and water before applying the ointment
C. Wear sterile gloves before applying the ointment
D. Ask the client to walk around the room after the application.
Absorption: Other Routes
• Transdermal: A disk or patch containing a days or weeks medication-Absorbed at a steady rate
•
Eyes - produces a local effect. Instruct patient to put pressure on the side of the nose after placing drops to decrease possibility of systemic effect.
•
Ears - used for local treatment of infection or wax
How should you position a client after instilling ear drops?
•
Nasal mucosa - instilled in droplet form or by swab for local or systemic effect.
Absorption:
PARENTERAL
• intravenous
• subcutaneous
• intramuscular
• intradermal
• intraarticular synovial cavity
• intrathecal - spinal subarachnoid space or epidural space
• intraperitoneal
REMEMBER – Parenteral meds retain 100% bioavailability
THEREFORE smaller doses are appropriate
Absorption:
PARENTERAL
• Subcutaneous and intramuscular injections are affected by tissue composition
• Intramuscular route is more effective than the subcutaneous route because there is a greater blood supply in muscle tissue.
• Application of heat or massage can increase vasodilation and improve absorption
Critical Thinking
Case
Mr. L. is admitted to the trauma unit with multisystem injuries from an automobile accident.
He arrived at the unit with multiple abnormal findings, including shock, decreased cardiac output, and urinary output of less than 30 mL/hr.
Which route of administration would be indicated for any medications for this patient?
Explain your reasoning.
#2 Distribution
•
Distribution : the transport of drugs from the blood to the site of action . A drug must be distributed to its site of action to have an effect
• Drugs are also distributed to tissues where it has no effect. Competition for drug binding sites affects the amount of drug available for action in the body .
Factors Affecting Distribution
Volume of Distribution (Vd) - The degree of distribution of a drug into various body compartments and tissue
• C ardiac output and capillary permeability affect the regional blood flow, perfusion of tissues and therefore the volume of distribution
Factors Affecting Distribution
Plasma Protein Binding - drugs bind to proteins in the blood (albumin, globulins) in varying degrees, from highly bound to poorly bound
Protein binding decreases the concentration of free drug in circulation therefore there is a limited amount of drug available to travel to the site of action. Only free drug is able to diffuse into tissues.
Only free drug is able to diffuse into tissues, interact with receptors, and produce biological effects.
Bound drugs are pharmacologically inactive.
Plasma Protein Binding
Continued
• When free drug is eliminated by the body some bound drug is released from protein binding.
• Some drugs persist in the body for three days by this mechanism.
• (2) drugs given concurrently & highly bound to the same site on a plasma protein will compete for the binding site resulting in a greater proportion of free drug .
• This effect may increase the free drug to toxic levels .
Critical Thinking
What effect would an albumin level of 2.8 have on distribution?
What should the nurse be alert to happening ?
Factors Affecting Distribution
• Tissue Binding/Affinity: force by which atoms are held together in chemical compounds
• Lipid soluble drugs have a high affinity for fat tissue and this is where these drugs are stored.
Drugs can be held in reservoirs such as adipose tissue or bone.
• What effect might sudden weight loss or starvation have on a client taking lipid soluble drugs?
Factors Affecting Distribution
•
Blood Brain Barrier - The structure of brain capillaries are less permeable than other body capillaries. Most drugs can’t pass this blood brain barrier. This protects the brain from the harmful effects of many drugs. Drugs that DO cross are highly lipid soluble. ( Ex: phenytoin, antidepressants, caffeine, nicotine )
What other substance did we talk about that is highly lipid soluble????????
• Placenta : the placental membrane is lipid in nature and readily allows non-ionized, lipid soluble drugs to cross the membrane. The use of many drugs has resulted in teratogenic effects on the developing fetus
CONSIDER THIS…
• The elderly have less effective blood-brain barriers.
• Symptoms of dizziness and lightheadedness are more common as side effects to many drugs taken by the elderly.
Look at your Lasix Drug Guide
• What is the site of action for distribution?
• What does it have to say about the drug’s distribution properties?
• Is this drug highly protein bound?
• What does this mean in regards to distribution?
#3 METABOLISM
•
Biotransformation: process by which the body changes the chemical structure of a drug to another form called a metabolite.
• Metabolite: a more water soluble compound that can be easily excreted.
The major organ for this process is the liver
METABOLISM (BIOTRANSFORMATION
)
•
First Pass Phenomenon - Drugs are first absorbed through the small intestine than arrive at the liver via the portal circulation
• There they undergo considerable biotransformation before entering the systemic circulation.
•
There will be less active drug available for action in the body cells after this first Pass through the Liver !
Consider this…
• Enzymes within the liver called cytochromes metabolize lipid soluble drugs.
• People with liver disease have a reduced amount of cytochromes
• What will the overall effect then be??
Variations in Metabolism
•
Pharmacogenetics - hereditary influences on drug responses, refers to variations in which individuals metabolize drugs.
Remember our discussion of Acetylator Rates?
•
Circadian Rhythms - the rate of drug absorption, hepatic clearance, half-life and duration of action, have all been shown to differ depending upon the time of day a drug is administered.
•
Effects of Gender and Age – BMR differences
GERIATRIC CHGS
#4 Excretion
Excretion: process where drugs are removed from the body. Kidneys are the major organs of excretion.
Lungs excrete gaseous drugs.
Biliary excretion (bile & feces) is important for a few drugs. These drugs may be reabsorbed when passing through the intestines from the liver
( enterohepatic re-circulation ).
Intestines, sweat, saliva and breast milk constitute minor routes of drug excretion.
Excretion
Clearance of drugs - elimination of drugs from circulation by all routes. It affects the time a drug remains in the body and the dosage required.
Renal Clearance
Hepatic clearance
PLASMA HALF-LIFE
• The amount of time a drug stays in the body is measured by the elimination half-life.
• This is the time required for the concentration of drug in the blood to decrease by 50%.
• Half-life affects the frequency of administration
• Drugs with short half-lives are quickly eliminated from the body. ( Ex: PCN given several X per day
)
• Drugs with longer half-lives stay in the body longer
(Ex: Digoxin given once a day )
Look at your LASIX drug guide
• What is the half-life of this drug?
• What does that mean in regards to dosing?
• Look at the Route/Dosage for the IV route for adults. What correlation can you make between the instructions there and the drugs half-life’s Time Action Profile?
III. PHARMACODYNAMIC PHASE
• What a drug does to the bodyrefers to the study of the mechanism of drug action on living tissue.
• Drugs may increase, decrease or replace enzymes, hormones or body metabolic functions.
• Chemotherapeutic drugs alter an abnormal parasite or growth on the body such as bacteria, viruses or neoplastic tissue.
examples: antibiotics and antineoplastic drugs .
THEORY OF DRUG-RECEPTOR
INTERACTIONS
• The majority of drugs are believed to exert their effects by combining with a specialized area on the cell or within the cell called receptors . Drug
+ Receptor
Drug receptor (binding) =
Response
• A drug receptor may be on the cell surface or within the cell
• Receptors come in many shapes that are specific for particular drugs.
• The greater the degree of specificity and selectivity for receptors, the fewer undesirable side effects and the greater drug efficacy.
Types of Drug-Receptor
Interactions
•
Agonists : Drug that has the ability to produce a desired therapeutic effect when bound to the receptor.
•
Antagonists : Drugs that bind well to the receptor but produce no receptor response. This can prevent other drugs from having an effect, thus they are called blockers.
Consider This…
• Bronchodilators (ie: albuterol ) used for asthma attacks are classified as betaagonists . They attach to adrenergic receptors in the sympathetic nervous system
(SNS) and mimic the action of norepinephrine.
• Adrenergic antagonists such as betablockers (ie: atenolol) attach to the adrenergic receptors in the SNS and block the action of norepinephrine
Types of Drug-Receptor
Interactions
•
Competitive antagonist : agonist drug and antagonist drug are each competing for the same site.
• The drug present in the greatest number will get bound.
• Therefore a higher dose of agonist is required to overcome this response
Saturability
• Drug receptor binding is saturable
• This occurs when all available receptors are occupied
• Once all available receptors are saturated, increasing the drug concentration WILL NOT increase therapeutic effect but it WILL increase the risk of adverse side effects
Other Ways Drugs Work
•
Enzyme Interaction
Some drugs bind to enzymes and block their action on cells ( ie ACE inhibitor)
•
Non-specific Interactions
No receptor action. Some drugs (ie antibiotics) get into bacteria cells and interrupt their cell processes leading to cell death
Time Course of Drug Action
• The frequency and duration of drug dosing can influence the safety and efficacy of drug therapy.
• Unless a drug is administered by a continuous infusion, variations will occur in the level of drug in the body.
•
Onset of drug action is the time it takes after the drug is administered to reach a concentration that produces a response.
•
Duration of action is the time during which the drug is present in a concentration large enough to produce a response.
•
Peak effect is the time it takes for the drug to reach its highest effective action.
Look at your Lasix Drug Guide
• What is the onset time for the PO route?
• Compare this to the onset for IV.
• If you gave your client 40mg of Lasix @
10am PO, when would you expect the greatest amount of diuresis?
•
Trough level will occur immediately before a drug is given, or once sufficient drug is eliminated. This is the lowest point of drug concentration
• Plasma blood levels may be taken for peak and trough levels. The drug must be administered precisely as ordered and a blood sample must be taken just before the next drug dose is scheduled for an accurate trough level.
Consider this…
• Certain drugs, such as aminoglycoside antibiotics
( Gentamycin ) are extremely ototoxic and nephrotoxic and are administered once daily.
• It is the responsibility of the nurse administering these medications to utilize therapeutic drug monitoring procedures
• Check trough levels 18-24 hrs after previous dose for a < 1mcg/ml level ( or previously set # from
MD / Lab / Pharmacy)
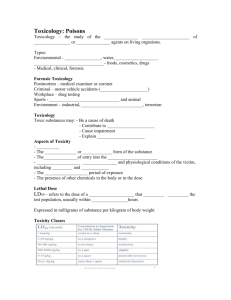
Therapeutic Responses
• Toxicity studies of drugs determine two dosage levels for drugs.
• The effective dose is the dose of a drug necessary to produce the desired intensity of effect in one-half of all patients.
• The lethal dose is the dose of a drug that elicits an undesirable toxic or lethal reaction in one-half of all patients.
Therapeutic Index
• A drug with a wide therapeutic index has a high safety margin and is relatively safe; the lethal dose is greatly in excess of the therapeutic dose.
• A drug with a narrow therapeutic index is more dangerous for the patient because small increases over normal doses may induce toxic reactions
. Peak and trough levels may need to be monitored
Look at your Lasix Drug Guide
• Do you think the therapeutic index of Lasix is high or low?
• Explain your answer.
•
Therapeutic range
: plasma drug concentration between minimum and toxic concentrations.
•
Loading doses
: higher amount of drug given once or twice to achieve maximum effective dose quickly
•
Maintenance dose
: intermittent doses given to maintain plasma levels.
Back to our Case Study
• The 72 y.o. client with hypertension was prescribed 40 mg of Lasix p.o. b.i.d.
• Would you say this is a maintenance dose?
• Why or why not?
• What is the highest loading dose you see in your Lasix drug guide for the p.o. route.
• Why didn’t the MD order this dosage?
Adverse Drug Event (ADE)
• General broad term that describes any adverse outcome to medication administration.
• Can be due to: staff error (preventable) OR
• Can be an adverse drug reaction (nonpreventable)
ADVERSE DRUG REACTIONS
(ADR)
• Unintended, undesirable or unpredictable drug effects. More than
50% of adverse reactions occur from drug-drug, drug-food, or druglaboratory test interactions.
ADR
•
Adverse Effects : are unwanted and/or unintended action that may occur during drug therapy. Every drug has the potential to produce adverse effects.
•
Side Effects : Undesirable but mild unavoidable/predictable pharmacological effects of a drug.
ADR
•
Toxic Effects: More serious effect. Life threatening. Each drug has characteristic toxic effects. May be due to the accumulation of the drug in the body r/t decreased renal function
•
Teratogenic Effects : Drug induced birth defects which follow drug therapy in pregnant women.
Look at your Lasix Drug Guide
• Are there any toxic LIFE THREATENING side effects to Lasix therapy?
• What are the most common side effects?
Drug Interactions
• Occur when 1 drug and a 2 nd drug or element such as food may have an effect on each other.
• These interactions may ↑ or ↓ the therapeutic effect of 1 or both drugs, create a new effect or ↑ incidence of adverse effects
Drug Interactions
• Additive effects : 2 or more “similar effect” drugs are combined. The result equals the sum of the individual agents Each drug is given in a lower dose for an equal effect of either drug given separately. 1+1=2 .
Ex: Percodan ( oxycodone + acetominophen) improves pain relief
• Synergism : The harmonious action of two “unlike” drugs producing an effect which is greater than the total effects of each drug acting by itself. 1+1=3 .
Ex: Advicor ( niacin + statin drugs) improves lipid lowering action.
Drug Interactions
• Potentiation : One drug improves the performance of the other drug. This is a particular type of synergistic effect.
½ + 1 = 2
Ex: amoxicillen + probenecid (anti-gout) prolongs serum levels of the antibiotic
• Idiosyncratic Reactions : Unusual, unexpected reactions to a drug, which may be genetically caused. Sometimes the person will react with the opposite effect to the desired one. (Also called paradoxical reaction)
Ex: Genetic G6PD enzyme deficiency (prevents RBC hemolysis) idiosyncratic reactions to ASA, sulfonamides
(African American and Kurdish Jewish populations)
Our Case Study
• Our 72 y.o. client has developed pneumonia and a DVT as complications from his immobility while hospitalized. The MD has ordered Gentamicin IVPB
( an aminoglycoside antibiotic ) and Heparin
(an anticoagulant).
What type of drug interactions should the nurse be alert to in conjunction with his
Lasix therapy?
Case Study - continued
The oral Lasix that our client is taking is not producing the desirable effect, and the MD orders a STAT dose of Lasix 40 mg IV. You prepare to inject this into the client’s IV line, but see that the Gentamicin previously ordered is currently infusing.
Is it OK to proceed with giving the Lasix IV?
Why of why not?
Allergic Reactions
• Increased reactions with repeated exposure to the drug.
• Hypersensitivity reactions are exaggerated in response to a drug.
• Anaphylaxis: A systemic reaction, the most severe of all the allergic reactions
.
(edema of airways, severe hypotension, cardiac arrhythmia, death)
Case Study
After starting a new IV line, you administer the
Lasix IV. The client almost immediately begins to experience an anaphylatic type reaction. He did not report any past allergies to Lasix, but he is allergic to “sulfa drugs”.
• Should this information have impacted your administration of the Lasix?
• Was this a preventable, predictable drug reaction?
• Was it a medication error?
Nursing Considerations
• Take a careful drug history
• Know what interactions to anticipate
• Identify the drug reaction by monitoring the patient response to the drug.
• Educate the patient and the family re the risks and benefits of the drug.
• Document any drug reactions clearly and specifically