File - Fronto-temporal dementia(MAPT gene)
advertisement
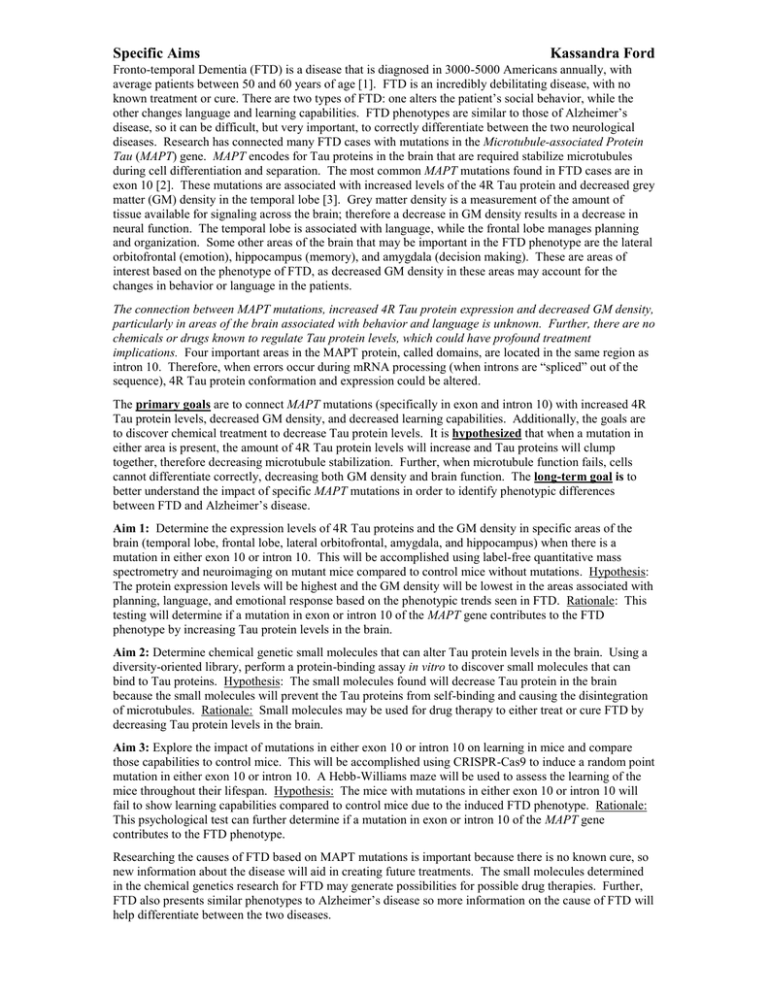
Specific Aims Kassandra Ford Fronto-temporal Dementia (FTD) is a disease that is diagnosed in 3000-5000 Americans annually, with average patients between 50 and 60 years of age [1]. FTD is an incredibly debilitating disease, with no known treatment or cure. There are two types of FTD: one alters the patient’s social behavior, while the other changes language and learning capabilities. FTD phenotypes are similar to those of Alzheimer’s disease, so it can be difficult, but very important, to correctly differentiate between the two neurological diseases. Research has connected many FTD cases with mutations in the Microtubule-associated Protein Tau (MAPT) gene. MAPT encodes for Tau proteins in the brain that are required stabilize microtubules during cell differentiation and separation. The most common MAPT mutations found in FTD cases are in exon 10 [2]. These mutations are associated with increased levels of the 4R Tau protein and decreased grey matter (GM) density in the temporal lobe [3]. Grey matter density is a measurement of the amount of tissue available for signaling across the brain; therefore a decrease in GM density results in a decrease in neural function. The temporal lobe is associated with language, while the frontal lobe manages planning and organization. Some other areas of the brain that may be important in the FTD phenotype are the lateral orbitofrontal (emotion), hippocampus (memory), and amygdala (decision making). These are areas of interest based on the phenotype of FTD, as decreased GM density in these areas may account for the changes in behavior or language in the patients. The connection between MAPT mutations, increased 4R Tau protein expression and decreased GM density, particularly in areas of the brain associated with behavior and language is unknown. Further, there are no chemicals or drugs known to regulate Tau protein levels, which could have profound treatment implications. Four important areas in the MAPT protein, called domains, are located in the same region as intron 10. Therefore, when errors occur during mRNA processing (when introns are “spliced” out of the sequence), 4R Tau protein conformation and expression could be altered. The primary goals are to connect MAPT mutations (specifically in exon and intron 10) with increased 4R Tau protein levels, decreased GM density, and decreased learning capabilities. Additionally, the goals are to discover chemical treatment to decrease Tau protein levels. It is hypothesized that when a mutation in either area is present, the amount of 4R Tau protein levels will increase and Tau proteins will clump together, therefore decreasing microtubule stabilization. Further, when microtubule function fails, cells cannot differentiate correctly, decreasing both GM density and brain function. The long-term goal is to better understand the impact of specific MAPT mutations in order to identify phenotypic differences between FTD and Alzheimer’s disease. Aim 1: Determine the expression levels of 4R Tau proteins and the GM density in specific areas of the brain (temporal lobe, frontal lobe, lateral orbitofrontal, amygdala, and hippocampus) when there is a mutation in either exon 10 or intron 10. This will be accomplished using label-free quantitative mass spectrometry and neuroimaging on mutant mice compared to control mice without mutations. Hypothesis: The protein expression levels will be highest and the GM density will be lowest in the areas associated with planning, language, and emotional response based on the phenotypic trends seen in FTD. Rationale: This testing will determine if a mutation in exon or intron 10 of the MAPT gene contributes to the FTD phenotype by increasing Tau protein levels in the brain. Aim 2: Determine chemical genetic small molecules that can alter Tau protein levels in the brain. Using a diversity-oriented library, perform a protein-binding assay in vitro to discover small molecules that can bind to Tau proteins. Hypothesis: The small molecules found will decrease Tau protein in the brain because the small molecules will prevent the Tau proteins from self-binding and causing the disintegration of microtubules. Rationale: Small molecules may be used for drug therapy to either treat or cure FTD by decreasing Tau protein levels in the brain. Aim 3: Explore the impact of mutations in either exon 10 or intron 10 on learning in mice and compare those capabilities to control mice. This will be accomplished using CRISPR-Cas9 to induce a random point mutation in either exon 10 or intron 10. A Hebb-Williams maze will be used to assess the learning of the mice throughout their lifespan. Hypothesis: The mice with mutations in either exon 10 or intron 10 will fail to show learning capabilities compared to control mice due to the induced FTD phenotype. Rationale: This psychological test can further determine if a mutation in exon or intron 10 of the MAPT gene contributes to the FTD phenotype. Researching the causes of FTD based on MAPT mutations is important because there is no known cure, so new information about the disease will aid in creating future treatments. The small molecules determined in the chemical genetics research for FTD may generate possibilities for possible drug therapies. Further, FTD also presents similar phenotypes to Alzheimer’s disease so more information on the cause of FTD will help differentiate between the two diseases. Specific Aims Kassandra Ford References: [1] The Association for Frontotemporal Degeneration. Disease Overview. (n.d.). Retrieved March 1, 2015, from http://www.theaftd.org/understandingftd/ftd-overview [2] Ghetti, B., Oblak, A., Johnson, K., Dickerson, B., & Goedert, M. (2015, February 1). Invited review: Frontotemporal dementia caused by microtubule-associated protein tau gene (MAPT) mutations: A chameleon for neuropathology and neuroimaging. Retrieved February 18, 2015, from http://onlinelibrary.wiley.com/doi/10.1111/nan.12213/epdf [3] Deters, K., & Al, E. (2014, December 5). Cerebral hypometabolism and grey matter density in MAPT intron 10 3 mutation carriers. Retrieved February 20, 2015, from http://www.ncbi.nlm.nih.gov/pubmed/25628962