poster - sharc
advertisement

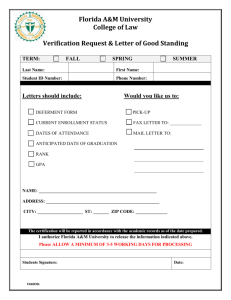
Co-infections of Hepatitis C or Tuberculosis Among Persons Living with HIV in The Florida Cohort Project Alexander Zirulnik MPH, Chukwuemeka Okafor MPH, Akemi Wijayabahu, Zhi Zhou MPH, Jennifer Janelle MD, Ezekiel Ojewale MD MPH, Robert Cook MD MPH for the Florida Cohort Investigators Background Results Florida has the highest incidence of new HIV infections in the country with a rate of 31.4% and increasing each year (Florida Charts, 2014). In 2014, newly reported HIV infections were distributed among 47% African Americans, 21% Hispanic, 30% White, and 2% other. High risk groups of HIV infection are African American, men who have sex with men (MSM), injection drug users (IDU) and young adults with risky behavior (alcohol and drug use). Chronic Hepatitis-C (HCV) account for 25% and Hepatitis-B infection account for 10% of co-infections in people living with HIV. Hepatitis infection has serious, life threatening conditions mostly pertaining to liver complications (AETC, 2015). Thus the Center for Disease Control has recommended vaccination against HBV and early detection of HBV and HCV. Unlike HBV, HCV does not have prophylaxis vaccines. IDU has been recognized as the major reason to acquire HCV in Florida, according to Florida Charts, 2013. When compared to Hepatitis co-infections, overall TB incidence has been decreased in Florida. Among Tuberculosis (TB) infected people, 8.9% are co-infections with HIV. Both major co-infections (HCV and TB) are disproportionately distributed among racial and ethnic minority groups in Florida. These co-infections continue to be clinical and are research priorities as it pertains to persons living with HIV. The purpose of this project is to examine any trends of co-infections among racial minorities in the Florida Cohort. Positive (-VL) Hispanic 82% 9% 4% Positive (Unknown VL) 5% Not Hispanic, Black Not Hispanic, White 82% 12% <1% 6% 72% 11% 3% 14% Discussion/Conclusion Methods The Florida Cohort was initiated in 2014 as part of the NIAAAsupported Southern HIV Alcohol Research Consortium (SHARC). Recruitment began in October of 2014 and currently includes urban (UF Health Shands, Orange, Hillsborough, Broward, and Miami-Dade Counties) and rural (Alachua, Sumter and Columbia Counties) sites. Participants completed a baseline survey that asked the m to selfreport a history of HCV or TB positive test results. See below: “Question 6. Have you ever been diagnosed with tuberculosis (TB), or been told you have a positive skin test (sometimes called a PPD) or a positive tuberculosis blood test (called a Quantiferon Gold or T-spot test)?” “Question 7. Have you ever been tested for Hepatitis C (Hep C)?” Participants’ information is further linked to medical records and statewide HIV surveillance data for confirmation. Co-infection status of first 575 persons enrolled were compared to the overall HIV positive population in Florida. Dependent Variable: Proportion of people in HIV cohort having HCV and TB positive test results Independent Variable: HCV and TB Co-Infection status (positive test results) Covariates Gender, race and Ethnicity HCV Status Confirmed by Labs (n=206) (% within each race/ethnicity) Race/Ethnicity Negative Positive (+VL) Florida Cohort Tuberculosis History (n=541) (% within each race/ethnicity) Race/Ethnicity No Yes Not Sure Hispanic Not Hispanic, Black Not Hispanic, White 79% 16% 5% 78% 18% 4% 92% 6% 2% Florida Cohort Hepatitis C Screening History (n=545) (% within each race/ethnicity) Race/Ethnicity None Yes – Yes – Result was Result was Positive Negative Hispanic 8% 21% 66% Not Hispanic, Black Not Hispanic, White Not Sure 5% 15% 23% 48% 14% 12% 18% 61% 9% • The Florida Cohort strives to represent an accurate representation of persons living with HIV in the state of Florida. • 15% reported a history of a positive Tuberculosis test, while 22% of the participants reported a positive Hepatitis C result. • In the Florida Cohort, tuberculosis co-infections are consistent with state surveillance data that shows TB rates are higher among minorities living with HIV. • Hepatitis C co-infections are proportionate among white and non-white participants in the Florida Cohort. • However, 14% (higher proportion of minorities) of our study population reports no history of HCV screening. Further expansion of HCV screening may result in increased treatment and resolution of HCV infections. • Over 10% of our sample have current, active HCV co-infections that could be cured/resolved. • As objective medical record abstraction increases among all participants in the Florida Cohort, a more accurate picture of coinfections will be presented. Strengths/Limitations • Self-reported measures from the Florida Cohort Survey remain the largest study limitation. However, using future laboratory results and confirmatory tests from medical abstractions (in progress), we hope to ascertain a more accurate diagnosis and screening history of all participants. Acknowledgement • Chang, C.C., Crane, M., Zhou, J., Mina, M., Post, J.J., Cameron, B.A., Lloyd, A.R., Jaworowski, A., French, M.A. and Lewin, S.R., 2013. HIV and co‐infections. Immunological reviews, 254(1), pp.114-142. • Funding support: NIAAA U24022002