Physical Characteristics of Blood
advertisement

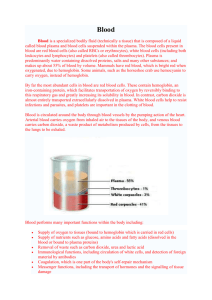
Physical Characteristics of Blood • Thicker (more viscous) than water and flows more slowly than water • Temperature of 100.4 degrees F • pH 7.4 (7.35-7.45) • 8 % of total body weight • Blood volume – 5 to 6 liters in average male – 4 to 5 liters in average female – hormonal negative feedback systems maintain constant blood volume and osmotic pressure Blood components • 55% = plasma: mainly water – 7 to 8% dissolved substances (sugars, amino acids, lipids & vitamins), ions, dissolved gases, hormones – most of the proteins are plasma proteins: provide a role in balancing osmotic pressure and water flow between the blood and extracellular fluid/tissues – loss of plasma proteins from blood – decreases osmotic pressure in blood and results in water flow out of blood into tissues swelling – most common plasma proteins: albumin, globulins, clotting proteins (fibrin) Blood: Cellular elements • 45% of blood is the cellular elements or formed elements • 99% of this (44.55% of total blood) is erythrocytes or RBCs – formed by differentiation of hematopoietic stem cells (HSCs) in the red bone marrow of long bones and pelvis – makes about 2 million per second! – made from an immature cell = reticulocyte – as they mature in the marrow they lose most organelles and its nucleus – lives only about 120 days – destroyed by the liver and spleen – liver degrades the hemoglobin to its globin component and the heme is degraded to a pigment called bilirubin - bile – Iron(Fe+3) • • • • transported in blood attached to transferrin protein stored in liver, muscle or spleen attached to ferritin or hemosiderin protein in bone marrow being used for hemoglobin synthesis -1% found in the Buffy coat : -leukocytes (WBCs) and platelets (thromobocytes) -neutrophils: phagocytic properties -release agents which destroy/digest bacteria -eosinophils: parasitic defense cells -also involved in the allergic response -release histaminase to slows down inflammation caused by basophils -basophils: release heparin, histamine & serotonin -heighten the inflammatory response and account for hypersensitivity (allergic) reaction -monocytes: enter various tissues and differentiate into phagocytic macrophages -lymphocytes: T and B cells Hematopoiesis HSC Hematocrit • Percentage of blood occupied by cells – female normal range • 38 - 46% (average of 42%) – male normal range • 40 - 54% (average of 46%) • testosterone • Anemia – not enough RBCs or not enough hemoglobin • Polycythemia – too many RBCs (over 65%) – dehydration, tissue hypoxia, blood doping in athletes Blood Groups and Blood Types • RBC surfaces are marked by genetically determined glycoproteins & glycolipids – agglutinogens or isoantigens – distinguishes at least 24 different blood groups • ABO, Rh, Lewis, Kell, Kidd and Duffy systems RH blood groups • Antigen was discovered in blood of Rhesus monkey • People with Rh agglutinogens on RBC surface are Rh+. Normal plasma contains no anti-Rh antibodies • Antibodies develop only in Rh- blood type & only with exposure to the antigen – transfusion of positive blood – during a pregnancy with a positive blood type fetus • Transfusion reaction upon 2nd exposure to the antigen results in hemolysis of the RBCs in the donated blood Hemolytic Disease of Newborn • Rh negative mom and Rh+ fetus will have mixing of blood at birth • Mom's body creates Rh antibodies unless she receives a RhoGam shot soon after first delivery – can lead to miscarriage or spontaneous abortion of future Rh+ children – RhoGam binds to loose fetal blood and removes it from body before she reacts • In 2nd child, hemolytic disease of the newborn may develop causing hemolysis of the fetal RBCs • Symptoms – oxygen-carrying capacity of blood is reduced – fatigue, cold intolerance & paleness Anemia • lack of O2 for ATP & heat production • Types of anemia – iron-deficiency = lack of absorption or loss of iron • type of nutritional anemia • failure to take in essential raw ingredients not made by the body – pernicious = lack of intrinsic factor for vitamin B12 absorption from the digestive tract • B12 is essential for normal RBC formation and maturation • binding of B12 to intrinsic factor allows its absorption • intrinsic factor – synthesized by the small intestine – hemorrhagic = loss of RBCs due to bleeding (ulcer) – hemolytic = defects in cell membranes cause rupture • rupture of too many RBCs by external factors such as malaria (normal RBCs) or genetic disorders like sickle cell anemia (defective RBCs) – thalassemia = hereditary deficiency of hemoglobin – aplastic = destruction of bone marrow (radiation/toxins) • failure of the bone marrow to produce enough RBCs • may selectively destroy the ability to produce RBCs only • but may also destroy the myeloid stem cells – affect WBCs and platelets Sickle-cell Anemia (SCA) • Genetic defect in hemoglobin molecule (Hb-S) that changes 2 amino acids in the globin protein – at low very O2 levels, RBC becomes deformed by changes in hemoglobin molecule within the RBC • sickle-shaped cells do not pass through capillaries well and get stuck = causing occlusions and decreased blood flow to organs • also rupture easily = causing anemia & clots • Found among populations in malaria belt – Mediterranean Europe, sub-Saharan Africa & Asia • Person with only one sickle cell gene – increased resistance to malaria because RBC Blood Clotting – in a test tube blood separates into liquid (serum) and a clot of insoluble fibers (fibrin) in which the cells are trapped – in the body the clot “plugs” damaged blood vessels and initiates healing – ultimate step is conversion of fibrinogen (soluble plasma protein) into insoluble fibrin • Substances required for clotting are Ca+2, enzymes synthesized by liver cells (clotting factors and plasma proteins) and substances released by platelets or damaged tissues – thrombin – released by damaged cells, catalyzes the conversion of fibrinogen to fibrin – 12 clotting factors involved • Clotting is a cascade of reactions in which each clotting factor activates the next in a fixed sequence resulting in the formation of fibrin threads – prothrombinase & Ca+2 convert prothrombin into thrombin – thrombin converts fibrinogen into fibrin threads Overview of the Clotting Cascade -may be triggered through two possible paths 1. extrinsic pathway 2. intrinsic pathway -both pathways result in the release and activation of specific clotting factors -either path leads to activation of the common pathway -common pathway results in the formation of prothrombinase (clotting factors X and V) -prothrombinase activates thrombin -thrombin cleaves fibrinogen to form fibrin The Body’s Response to Infection: The Immune System • Three lines of defense The Body’s Response to Infection: First Line of Defense • 1. Skin – Sheds, takes pathogens with it – Has low pH, repels microorganisms – Glands in skin secrete chemicals to slow bacterial growth • 2. Mucous membranes – Mucous traps pathogens – Can be sneezed, coughed away The Body’s Response to Infection: Second Line of Defense • 1. White blood cells production • A.: macrophages and other phagocytes – Engulf and digest invasive organisms – Also digest old red blood cells and cellular debris – Can release chemicals to stimulate production of more white blood cells – like T and B cells • B. White blood cells: natural killer cells – Attack tumor cells and virus-infected cells – Release chemicals that break apart the cell membranes of infected cells or tumor cells The Body’s Response to Infection: Second Line of Defense – Inflammation • 2. Inflammation: response which produces redness, warmth, swelling, and pain – After tissue injury, damaged cells release histamine – Histamine causes vasodilation which increases blood flow • this will increase more WBCs into the infected area • brings more O2 and nutrients – BUT also brings in more fluid – some fluid gets pushed out into the surrounding tissues = Swelling The Body’s Response to Infection: Second Line of Defense – Defensive Proteins • 3. Interferons are produced by infected cells – bind to healthy cells – stimulate production of anti-viral chemicals • 4. Complement proteins are made in response to inflammation and infection – are a class of about 20 different proteins – can coat surface of bacteria to facilitate phagocytosis – can make holes in bacterial membrane BOOM! The Body’s Response to Infection: Second Line of Defense – Fever • 5. Fever – temperature above range of 97-99º F – macrophages can release pyrogens • which causes temperature of tissue to increase – increased temperature inhibits bacterial growth – increases metabolism of healthy cells – promotes mitosis and tissue repair – large-scale production of pyrogens can increase overall body temperature = Fever – also increases the efficiency of immune cells The immune system Cells of the immune cells (macrophages, T cells, B cells) are found in specific locations called lymphatic tissues The Body’s Response to Infection: Third Line of Defense – Lymphocytes • Lymphocytes are a specific defense because they recognize specific antigens – antigen = cell-surface protein that identifies the type of cell bearing it • also distinguishes it from antigens in another organism • when your immune system is developing – your lymphocytes learns what antigens belong to you and what don’t – develop self-tolerance • examples of non self-tolerant, foreign antigens = proteins found on or in viruses, bacteria, fungi, protozoans and worms. • Lymphocytes travel throughout the body in spaces between the cells and are carried in the blood and lymphatic system. The Lymphatic System • Lymphocytes travel throughout the body in spaces between the cells and are carried in the blood and lymphatic system. • the lymphatic system = system of lymphatic vessels + lymph nodes + lymphatic tissues (spleen, thymus, tonsils) that filter lymph and circulate WBCs • lymph = yellow-colored fluid that is produced from your blood plasma – – produced when plasma filters out of your blood and into your tissues some of that filtrate becomes lymph The Lymphatic System • • • • • Lymph comes from your blood plasma but is returned to you blood stream along the way it flows through lymph nodes which house lymphocytes and macrophages these immune cells clean the lymph of bacteria so what gets returned to your blood is cleaned lymph is the way we “launder” our blood http://www.niaid.nih.gov/topics/immuneSystem/Pages/structureImages. aspx The Body’s Response to Infection: Third Line of Defense – Lymphocytes • Two types of Lymphocytes – A. T cells – B. B cells Lymphocytes • Lymphocytes are produced from stem cells in the red bone marrow. • they are named by the location where they were first identified • B cells develop in the bone marrow • T cells develop in the thymus – thymus disappears over time T and B Lymphocytes • B cells – Recognize small organisms such as bacteria by producing antibodies – antibodies = small proteins that bind foreign antigens and target the foreign cell for destruction by the host’s immune system – can respond to viruses if “helped” by T cells Antibody: abbreviated as Ig made up of four protein chains two light chains two heavy chains – determine the type of antibody “ends” of the antibody are specific for the foreign antigen = “Antigen-binding Site” T and B Lymphocytes • T cells – Respond to larger organisms (e.g. fungus), viruses, and body cells that have gone awry (e.g. tumor cells) • also attack transplanted tissues! • if they attack normal cells = Auto-immune disease – Attack the antigen-bearing cell directly by secreting chemicals that kill it – help B cells and “teach” them what antibodies to make • can bind a foreign protein and then interact with a B cell • B cell then makes antibodies to that foreign protein T and B Lymphocytes • B and T cells display cell-surface proteins that bind to foreign antigens – called antigen receptors – once they bind the T and B cells are called “activated” – activated T cells “help” B cells by physically binding them – the B cell then begins to make antibodies B and T cells have a Memory once the infection is cleared, there are a small number of T and B cells that “remember” the infection will become activated if the foreign antigen re-appears faster activation than the 1st time Types of Immunity: Antibody and CellMediated Immunity • B cell mediated immunity is called Antibody mediated immunity • B cells exposed to foreign antigens rapidly divide = clonal expansion • most B cells develop into plasma cells that make the antibodies • Rest of B cells become memory cells to provide long term immunity Antibody and Cell-Mediated Immunity • T cell mediated immunity is called Cell-mediated immunity • T cells divide exposed to foreign antigens divide and develop into different types of cells – depends on the foreign antigen – if it’s a bacterial antigen helper T cells • help B cells make antibodies – if it’s a viral or tumor antigen cytotoxic T cells • secrete chemical to directly kill the pathogen • e.g. interferons • some stay as memory T cells Cell-Mediated Immunity T cells need “help” learning what a foreign antigen is the are “presented” the foreign antigen by another cell = Antigen-Presenting cell the APC internalizes the foreign invader and “displays” foreign antigens on its surface the T cell binds the APC and “learns” what the foreign antigen looks like the T cell is now activated and can develop either into helper or cytotoxic T cells foreign cell foreign antigen secrete chemicals called interleukins that enhance B cell and T cell activity also help B cells to make antibodies Types of Immunity • immunity can also be classified into: • Passive Immunity – short-term immunity, lasts as long as the antibodies are in bloodstream. – can be passed on via fluids – e.g. antibodies found in breast milk • Active Immunity – long-term, caused by exposure to antigen and production of B and T cells. – basis for immunity from vaccinations Vaccinations • Vaccinations attempt to take advantage of longterm immunity through exposure to parts of antigens. – Produces population of memory cells – Some antigens, such as flu, mutate quickly and require frequent vaccinations – Some antigens are difficult to make vaccines for The Body’s Response to Infection: The Immune System – Allergy • Allergy – immune response that occurs even though no pathogen is present – Body reacts to a non-harmful substance as if it were pathogenic • called an allergen – immune cells called mast cells produce large amounts of histamine and leukotrienes inflammation – Common allergies include ragweed pollen and peanuts – Asthma might be caused by allergy