Developing Automated Communicable Disease Reporting
advertisement

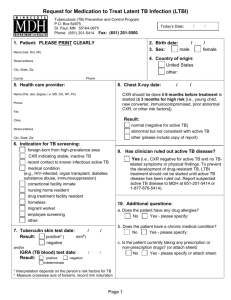
Developing Automated Communicable Disease Reporting: Two Pragmatic Technological Solutions Kathryn Como-Sabetti, Asa Schmidt, Dede Ouren, Kathleen Steinmann, Matt Muscha, Richard Danila Minnesota Department of Health, HealthPartners Inc., Hennepin County Medical Center Minnesota Communicable Disease Reporting Rule • MN statute requires all licensed healthcare providers and laboratorians to report specific communicable disease • 78 pathogens/syndromes are reportable – 18 immediately reportable by phone – 60 reportable within 1 working day • Over 25,000 reportable communicable diseases received in 2010 Minnesota Communicable Disease Reporting Rule, cont. • Centralized communicable disease reporting – Case investigation may be performed by local public health depending on pathogen and jurisdiction • Minnesota is part of the Emerging Infection Program – Increases the number of reportable diseases and complexity of reporting Communicable Disease Reporting Process – Non Urgent Reports IP Identifies reportable disease IP Reviews Chart and Completes CRF CRF Submitted to MDH (via fax, mail, phone or web) CRF Submitted to MDH (via fax, mail, phone or web) MDH receives CRF MDH enters information from CRF into program database MDH receives CRF Repeat multiple times per day MDH Enters Case Into Program Database IP Reviews Chart for Additional Information MDH Calls IP for additional Information (sometimes) Background • Communicable disease reporting rule changed in 2004 – MN-APIC/IPs expressed concern about the burden of increased reporting – MDH agreed to look into ways to decrease reporting burden • Fall 2006; MN-APIC authored a letter to the Commissioner of Health regarding the increasing burden of infectious disease reporting • Difficult economic times force all agencies to “find efficiencies” ADR vs ELR • MDH has had a number of labs submitting communicable disease reports through electronic laboratory reporting (ELR). • ELR had limited impact on disease reporting when ELR has very little case information. – IPs still required to either complete a case report form ADR vs ELR, cont. • Automated disease reporting (ADR) includes demographic, contact, laboratory, and facility information – Combines ELR with information from the patient’s electronic health record – Decreases the number of case reports completed by IPs MINNESOTA DEPARTMENT OF HEALTH COMMUNICABLE DISEASE REPORTING FORM Disease Name: ________________________ Onset date:____/____/____ DEMOGRAPHIC INFORMATION LABORATORY AND FACILITY INFORMATION Name Reporter Last: ___________________________ First: ______________ DOB:____/____/____ Age:_____ Days Gender: Report date:____/____/____ Male Female Transgender Months MI: _________ Years Country of birth: City: _________________________________________ Ordering provider:_____________________________ English Other:________________________ U.S. Other:______________ Phone: _____________________ Institution/Clinic: ______________________________ Unknown Medical record #: ___________________________________________ Preferred language: Name: _______________________________ Unknown Phone:_______________________________________ Primary care provider: _________________________ Address:___________________________________________________ Unknown Homeless Phone:_______________________________________ Lab Name:_____________________________________ City:______________________ State:____ Zip:_____ Phone:_________________________________________ County:________________ Phone 1st:___________________Phone 2nd:_____________________ Occupation:_______________ Parent/Guardian:_______________ MDH contact if additional information needed (choose at least one): Reporter Primary care provider Ordering provider Lab Other:_______________________________________________________ Was the patient hospitalized? Yes No Unknown Ethnicity: Race (check all that apply): Hispanic/Latino American Indian/Alaskan Native Asian Hospital name: _________________________________________________ Non-Hispanic/ NonLatino Black/African American White Admit date: ____/____/____ Discharge date: ____/____/____ Native Hawaiian/Pacific Islander Unknown Died? Yes No Unknown If yes, date of death: ____/____/____ Unknown Other:______________________________ Specimen collection date: _____/_____/_____ Specimen source :______________________________________ Pregnant (if applicable): Yes No Unknown IF YES, due date: _____/_____/_____ Highlighted fields were identified as those in electronic medical records that could be pulled though an automated process. Revised 6/10 Solution #1 - Background • August 2007 RFA released by MDH for data mining systems to develop automated reporting to MDH – 2 awards approximately $24,000 each – No applications • April 2009 RFA released by MDH for health systems to develop automated reporting to MDH – 1 award up to $92,000 – Awarded to HealthPartners/Region’s Hospital Grant Objectives • Automate the pull of demographic information from an electronic medical record and send an electronic case reports to MDH – HealthPartners opted to automate the identification of reportable diseases • Develop a roadmap for other institutions to develop ADR Solution #1 - Process • Teams were formed at HealthPartners and MDH and included experts from the Laboratory, Epidemiology, Infection Prevention, and Information Technology (IT) – IT experts included: project management, message format, message transport, translation, and laboratory information systems • Kick off meeting • Monthly project conference calls Solution #1 – Implementation • 681 tags of laboratory test/result combinations identified reportable diseases • Once tagged, case reports were generated using Clarity extracting from the patient’s medical record (EPIC) Solution #1 – Implementation Sunquest 1. Lab results in LIMS (sunquest) triggers the feed EPIC 2. Information is passed on to the HER (EPIC), for case information HL7 3. HL7 message is created PHIN-MS Rhapsody 4. Transfer of file to MDH 5. Upload of data into MEDSS 6. IP staff at regions have access to add additional information manually TASK format HL7 results from LIS to EHR system confirm the English Text Code tag interpretation confirm reportable flag confirm extracted data is formatted in the proper sequence HL7 format has data elements mapped into agreed locations confirm standard encrypted EDI transmission from RH to MDH data communication is functional DEPARTMENT Infection Prevention Microbiology LIS IT Solution #2 - Background • Hennepin County Medical Center (HCMC) contracted with Premier to implement SafetySurveillor for healthcare associated infection surveillance • Included in the contract was a provision that SafetySurveillor would develop reports identifying reportable communicable diseases Solution #2 - Process • 4 reports were developed by HCMC and Premier to identify cases: – Communicable disease report to identify cases by pathogen only – Communicable disease report to identify cases by pathogen and specimen source – Neonatal sepsis report (pathogen and patient DOB) – Invasive MRSA report Solution #2 – Process, cont. • Paper reporting by healthcare providers for STDs continues with ADR reporting to audit – Process to identify treatment is not automated but necessary for STD reports • MDH approved message format – Message includes demographic, contact, laboratory, hospitalization and provider information Solution #2 – Process, cont. • Team was not formed • Facility IP coordinated development of SafetySurveillor reports • IP coordinated IT assistance as needed at the facility Solution #2 – Implementation Premier .csv 1. Reports run by HCMC staff in the Premier system 3. Flat file is created PHIN-MS 4. Transfer of file to MDH Rhapsody 5. Upload of data into MEDSS 6. IP staff at HCMC have access to add additional information manually Current Status Solution #1 • MDH receives files daily from HP – Implementation is going through a validation step to confirm all data is correct • Upload into MEDSS will create new disease events in the system – De-duplication will try to match to existing persons and events. • Disease events will be listed on daily workflows for epis (routing is based on disease) • IPs at HP are being trained on MEDSS Current Status Solution #2 • MDH receives files twice a week from HCMC – MDH staff time saved for reviewing HCMC charts • Files are manually routed to disease program staff • MEDSS team is currently working on mapping the message into MEDSS • Approximate 20% of chlamydia and gonorrhea was not reported by providers Lessons learned • ADR improved disease reporting at HCMC • Manual process of running ADR reports resulted in reports not being sent daily • ADR decreases the burden of infectious disease reporting on healthcare facility staff – Once in MEDSS we expect ADR will decrease MDH staff time spent entering records Lessons learned, cont. • There is no standard. Rules for the what tests/results to send are unique – Early discussions about when to send data is essential – Lab/IP staff provide the knowledge • IT/Lab/IP/EPI partnership essential – Team approach lead to smoother implementation • IP provides clinical interpretation Lessons learned, cont. • Creating the ADR message was complicated without a standard to fall back on, we ended up modifying the HL7 message for ELR reporting • Standardized coding of tests and results would make it easier to route to the correct program areas/epis • When data is sent from one system to another information gets lost – Example: Coded test/results in LIMS were passed on as text to the EHR system, forcing us to translate them back after we received it. Lessons learned, cont. • A practical focus made it possible – What data elements can we rely on? If we can’t trust the data don’t try to get it if its complicated – What is our goal? If we want things to be easier for the IPs and we manage to do an automated transfer of 80% of the cases, can’t they then do the rest manually if we give them the tools? – If we maintain the process of ‘report immediately by telephone’ for the conditions that needs this we got our EPIs to be more confident in the process Questions and Contact Information • Asa Schmidt, Project Manager – Asa.schmidt@state.mn.us • Kathryn Como-Sabetti, Epidemiologist – Kathy.como-sabetti@state.mn.us 651-201-5414