6.Urine concentration and dilution
advertisement

Urine concentration and dilution
Learning objectives
• Describe the mechanism of formation of
dilute and concentrated urine.
• Describe the role of the ascending limb of
the loop of Henle in producing a high renal
interstitial fluid osmolality. Beginning with
the loop of Henle, contrast the tubular fluid
and interstitial fluid osmolality changes that
allow either dilute or concentrated urine to
be produced and excreted.
Learning objectives
• Identify the tubular section and cellular
mechanism by which ADH increases
permeability to water and urea.
• Distinguish between central and
nephrogenic diabetes insipidus based
on plasma ADH levels and the response
to an injection of ADH.
Dilute urine
• 1. Because the osmolarity of the interstitial
fluid of the renal medulla becomes
progressively greater, more and more water is
reabsorbed by osmosis as tubular fluid flows
along the descending limb toward the tip of
the loop.
• 2. Cells lining the thick ascending limb of the
loop have symporters that actively reabsorb
Na, K, and Cl from the tubular fluid. As
solutes—but not water molecules—are
leaving the tubular fluid, its osmolarity drops
to about 150 mOsm/liter.
3. While the fluid continues flowing along the
distal convoluted tubule, additional solutes but
only a few water molecules are reabsorbed.
4. Finally, the principal cells of the late distal
convoluted tubules and collecting ducts are
impermeable to water when the ADH level is
very low.
Formation of Concentrated
Urine
Production of concentrated urine by the
kidneys occurs in the following way
1) Symporters in thick ascending limb cells
of the loop of Henle cause a buildup of Na
and Cl in the renal medulla.
2) Countercurrent flow through the
descending and ascending limbs of the
loop of Henle establishes an osmotic
gradient in the renal medulla
• tubular fluid becomes progressively more
concentrated as it flows along the descending
limb and progressively more dilute as it moves
along the ascending limb.
3) Cells in the collecting ducts reabsorb more
water and urea.{ under ADH}
4 )Urea recycling causes a build up of urea in the
renal medulla
• Solute concentration of the interstitial fluid in the
kidney increases from about 300 mOsm/liter in
the renal cortex to about 1200 mOsm/liter deep
in the renal medulla.
• The three major solutes that contribute to this
high osmolarity are Na, Cl , and urea.
• Two main factors contribute to building and
maintaining this osmotic gradient:
(1) differences in solute and water permeability and
reabsorption in different sections of the long
loops of Henle and the collecting ducts, and
(2) the counter current flow of fluid through tubeshaped structures in the renal medulla.
Overview of Countercurrent
Multiplication Mechanism
• Descending limb extracts water and
concentrates the ultrafiltrate
• Thick ascending limb extracts NaCl
– Concentrates medullary interstitium
– Dilutes ultrafiltrate
Generating a Concentrated Medullary
Interstitium - Key Steps
Cortical Collecting Duct
Urea
Cortex
2
H2O
1
Outer
Medulla
H2O
Na+
K+
2Cl-
NaCl
H2O
Medullary
Collecting Duct
4
Inner
Medulla
H2O
NaCl
Urea
NaCl
NaCl
5
3
NaCl
NaCl
Loop of Henle
H2O
Urea
Urea
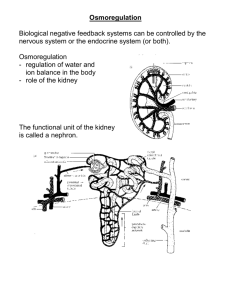
Counter current multiplication
• Is the process by which a progressively
increasing osmotic gradient is formed in the
interstitial fluid of the renal medulla as a
result of countercurrent flow.
Countercurrent Multiplication Schematic Model
PT
DT
300
300
Initial
Conditions:
Assume all
fluid starts
out isotonic
300
300
300
300
300
300
300
300
300
300
300
300
300
300
300
300
LH
300
300
300
300
300
300
300
300
Countercurrent Multiplication Schematic Model
PT
Flow Stopped:
NaCl and H2O
movements
occur (assume
200 mOsm/L
gradient is
established by
thick AL pump)
DT
400
400
400
400
400
400
400
400
400
400
400
400
400
400
400
400
LH
200
200
200
200
200
200
200
200
Countercurrent Multiplication Schematic Model
PT
DT
300
200
Flow Occurs:
Fluid leaves
ascending limb
and new fluid
enters descending
limb from PT
200
200
200
200
400
400
400
400
300
300
300
300
400
400
400
400
LH
Countercurrent Multiplication Schematic Model
PT
Flow Stopped:
NaCl and H2O
movements
occur
DT
350
350
350
350
500
500
500
500
350
350
350
350
500
500
500
500
LH
150
150
150
150
300
300
300
300
Countercurrent Multiplication Schematic Model
PT
DT
300
150
Flow Occurs:
Fluid leaves
ascending limb
and new fluid
enters descending
limb from PT
150
150
300
300
300
300
500
500
300
300
350
350
350
350
500
500
LH
Countercurrent Multiplication Schematic Model
PT
Flow Stopped:
NaCl and H2O
movements
occur
DT
325
325
425
425
425
425
600
600
325
325
425
425
425
425
600
600
LH
125
125
225
225
225
225
400
400
Countercurrent Multiplication Schematic Model
PT
DT
300
125
Flow Occurs:
Fluid leaves
ascending limb
and new fluid
enters descending
limb from PT
125
225
225
225
225
400
400
600
300
325
325
425
425
425
425
600
LH
Countercurrent Multiplication Schematic Model
PT
Flow Stopped:
NaCl and H2O
movements
occur
DT
312
375
375
425
425
513
513
700
312
375
375
425
425
513
513
700
Etc., etc.!
LH
112
175
175
225
225
313
313
500
Countercurrent Exchange
• Is the process by which solutes and water are
passively exchanged between the blood of the
vasa recta and interstitial fluid of the renal
medulla as a result of countercurrent flow
Slow flow:
• Flow through the loop is relatively slow. This is
also a characteristic of flow through the capillary
loops (vasa recta). Increased tubular fluid flow
diminishes the ability of the loop to generate and
maintain the osmolar interstitial gradient.
• Increased flow through the vasa recta washes
out the metabolites.
• Loss of the high medullary osmolarity reduces the
ability of the kidneys to form a concentrated
urine
Urea Recycling
A normal 70-kilogram human must excrete
about 600 milliosmoles of solute each day. If
maximal urine concentrating ability is 1200
mOsm/L, the minimal volume of urine that
must be excreted, is called the obligatory urine
volume, and can be calculated as
Role of ADH
• The osmoreceptor neurons in the hypothalamus are
extremely sensitive and are able to maintain ECF
osmolarity within a very narrow range.
• There is a resetting of the osmostat downward in
pregnancy, the men-strual cycle, and with volume
depletion. In the latter case osmoregula-tion is
secondary to volume regulation; a return of
circulating volume will occur even as osmolarity
decreases.
• Volume receptors are less sensitive than
osmoreceptors and a change of 10–15% in volume is
required to produce a measureable change in ADH.
• Cortisol and thyroid hormone restrain the release of
ADH.
Effect of Alcohol and Weightlessness
on ADH Secretion
• Ingesting ethyl alcohol or being in a weightless
environment suppresses ADH se-cretion.
• In weightlessness, there is a net shift of blood
from the limbs to the abdo-men and chest.
• This results in greater stretch of the volume
receptors in the large veins and atria, thus
suppressing ADH secretion
Q
ADH will be released from the posterior pituitary
when there is a decrease in
a. Plasma Na+ concentration
b. Plasma volume
c. Plasma K+ concentration
d. Plasma pH
e. Plasma Ca2+concentration
At the kidney (collecting duct)
ADH
cAMP
V2
Nephron
lumen
Vesicles
containing
AQP2
’s AQP2
production
Interstitial
Space
ACTIONS OF ADH
1.ACTION ON KIDNEY
Maintenance of ECF volume & Osmolarity
Acts on DCT and CD of kidney Reabsorbs water
Maintenance of volume more important that
maintenance of osmolarity
2.VASOCONSTRICTOR EFFECT (V1 receptors)
3.ACTION ON ANTERIOR PITUITARY-cause increased
ACTH secretion from the corticotroph
Q. In the presence of ADH, the filtrate will be
isotonic to plasma in the
a. Descending limb of the loop of Henle
b. Ascending limb of the loop of Henle
c. Cortical collecting tubule
d. Medullary collecting tubule
e. Renal pelvis
PATHOPHYSIOLOGIC CHANGES IN
ADH SECRETION
Central diabetes insipidus
• Sufficient ADH is not available to affect the
renal collecting ducts.
• Causes include familial, tumors
(craniopharyngioma), autoimmune, trauma
• Pituitary trauma – transient diabetes insipidus
• Sectioning of pituitary stalk – triphasic
response: diabetes insipidus, followed by
SIADH, followed by a return of diabetes
insipidus
Nephrogenic diabetes insipidus
• Due to inability of the kidneys to respond to
ADH
• Causes include familial, acquired, drugs
(lithium)
Syndrome of Inappropriate ADH Secretion(SIADH
• Excessive secretion of ADH causes an inappropriate increased
reabsorption of water in the renal collecting duct.
• Causes
Ectopic production of ADH (small cell carcinoma of the lung)
Drug induced
Lesions in the pathway of the baroreceptor system
• Pathophysiology
Increased water retention, hyponatremia, but clinically euvolumic
Volume expansion increases ANP, decreases renin creating a
natriuresis, which contributes to the hyponatremia.
Inappropriate concentration of urine, can be greater than plasma
osmo-larity
• Treatment- Fluid restriction but not salt restriction
Serum
Osmolarity/S
Urine
Serum ADH erum [Na+] Osmolarity
Primary
polydipsia
Central
diabetes
insipidus
↓
↓
Urine Flow
Rate
CH2O
Hyposmotic
High
Positive
Increased
Hyposmotic
(because of
excretion of too
much H2O)
High
Positive
Hyposmotic
High
Positive
Hyperosmotic
Low
Negative
Decreased
Hyperosmotic
(because of
reabsorption of
too much H2O)
Low
Negative
Decreased
Nephrogenic ↑ (because of Increased
increased
(because of
diabetes
plasma
excretion of too
insipidus
osmolarity)
much H2O)
Water
deprivation
↑
SIADH
↑↑
High-normal
The following information was obtained in a 20-year-old college
student who was participating in a research study in the Clinical
Research Unit:
Plasma
Urine
[Inulin] = 1 mg/mL
[Inulin] = 150 mg/mL
[X] = 2 mg/ml
[X] = 100 mg/mL
Urine flow rate =
1 mL/min
Assuming that × is freely filtered, which of the following statements is
most correct?
(A) There is net secretion of X
(B) There is net reabsorption of X
(C) There is both reabsorption and secretion of X
(D) The clearance of × could be used to measure the glomerular
filtration rate (GFR)
(E) The clearance of × is greater than the clearance of inulin
Renal Tubular Acidosis Type II
• Due to a diminished capacity of the proximal
tubule to reabsorb bicarbonate.
• Transient appearance of bicarbonate in the urine
until the filtered load is reduced to match the
reduced capacity of reabsorption.
• Steady-state characterized by a low plasma
bicarbonate and an acid urine.
• An example would be Fanconi syndrome, which
involves a general defect in the proximal tubular
transport processes and carbonic anhydrase
inhibitors.
Renal Tubular Acidosis Type I
• Due to an inability of the distal nephron to
secrete and excrete fixed acid, thus an inability to
form an acid urine. Urine pH > 5.5 – 6.0
• Mechanisms would include impairment of the
transport systems for hydrogen ions and
bicarbonate and an increased permeability of the
apical membrane allowing the back diffusion of
the hydrogen ions from the tubular lumen.
• The result would be a metabolic acidosis with an
inappropriately high urine pH.
OVERVIEW OF RENAL FAILURE
• Categorization of renal dysfunction based on
location and cause:
• Prerenal originate because of a hypoperfusion of
kidney, e.g., structural lesions of the renal
vasculature, generalized hypotension, drug
effects on nephron perfusion.
• Intrarenal originate from direct damage to the
nephron system, either the glomerulus or the
nephron itself.
• Postrenal originate from urinary tract
obstruction, e.g., kidney stones, prostate
enlargement or spasm.
Renal Functions Affected
1. Elimination of waste products
• Uremia (↑ BUN, ↑ creatinine)—Urea and
creatinine are themselves nontoxic but
function as indices of the accumulation of
toxic waste products of metabolism.
• Uremia is a syndrome with specific clinical
manifestations including vomiting, dyspnea,
headache, and leading to, if untreated,
convulsions and coma.
2. Salt and water balance
• Inability to regulate sodium and water excretion. This
can lead to hyponatremia and volume overload as well
as hypernatremia and volume depletion very quickly
following vomiting and diarrhea.
• An inability to regulate potassium excretion leads to
hyperkalemia.
3. Acid–base regulation
• A reduction in the ability to excrete fixed acid end
products of metabolism leads to a metabolic acidosis
and a widening of the anion gap.
4. Hormonal secretion
• Hypocalcemia due the failure to activate vitamin D
• Anemia due to lack of erythropoietin
• Vascular consequences due to altered renin release
Acute Renal Failure
• It is a rapid loss of renal function and results in the accumulation of
waste products in the blood that are normally excreted by the kidney
(↑BUN, ↑creatinine)
• Prerenal: decreased renal perfusion as would occur with a decreased
renal perfusion pressure, e.g., hypovolumia of hemorrhage, diarrhea,
vomiting; congestive heart failure
Initially no renal injury and reversible if corrected early.
• Intrarenal: glomerulonephritis, interstitial nephritis, ischemia,
rhabdomyolysis, sepsis.
Tends to quickly lead to acute tubular necrosis
• Postrenal: obstruction of the outflow tract
• All eventually lead to acute tubular necrosis, which is a direct tubular
damage.
• Tubular cells lose their ability to attach to other cells and many slough
into the filtrate and appear in the urine. It may be reversible or
irreversible depending on the extent and duration of injury
Chronic Renal Failure
• In chronic renal failure there is an irreversible loss of
nephrons. The remaining nephrons, in order to
compensate, have an increase in glomerular capillary
pressure and hyperfiltration.
• One way of looking at this is a “hypertension” at the level
of the nephron.
• The hyperfiltration combined with the increased work load
promotes further injury leading to fibrosis, scarring, and
loss of additional nephrons.
• Chronic renal failure is categorized based on the level of
GFR and the presence or absence of proteinuria.
• When GFR decreases to about 20% of normal the BUN
starts to rise but the patients may still be asymptomatic
• Most patients have some sodium and water
retention. This can lead to hypertension,
congestive heart failure, and peripheral edema.
• Compensatory increases in aldosterone initially
prevent hyperkalemia but beyond a certain point
this becomes a problem.
• Additionally, phosphate retention and loss of
vitamin D activity cause a secondary
hyperparathyroidism and bone loss; anemia is
due to loss of erythropoietin.
Diabetic Nephropathy
• Diabetes is the most common cause of chronic renal
failure.
• Characterized by proteinuria, glomerular lesions that
are associated with eventual capillary collapse,
glomerulosclerosis, and loss of GFR.
• Hyperglycemia and insulin deficiency play a major role
in diabetic nephropathy at least in the development of
“nephron hypertension” and hyperfiltration.
• In many instances the patient begins with an abovenormal GFR.
• The first sign of renal disease is microalbuminuria.
• As GFR decreases the proteinuria increases.
• A young man comes to his family physician
because of recently developed pitting edema on
the lower extremities. Blood pressure is normal.
• Laboratory results include the following:
Blood chemistry
Creatinine = 0.89 mg/dL
BUN = 13 mg/dL
Albumin = 1.6 g/dL
Calculated urine excretion of protein = 7.4 g/day
Urine sediment = occasional hyaline casts, red cells
rare, oval fat bodies
• This individual displays the classic proteinuria (>3.5
g/day) of nephrotic syndrome.
• Some patients are asymptomatic but this individual
displays the more severe consequences, i.e., the
hypoalbuminemia and edema due to fluid retention
and urinary losses of protein.
• Nephrotic syndrome reflects a noninflammatory
injury to the glomerular membrane system.
• The damage is usually to the epithelial podocytes or
the basement membrane. .
• Creatinine is usually close to normal, however, there
is a decreased surface area for filtration and some
decrease in GFR. There also tends to be a high blood
cholesterol.
A young man comes to his family physician
because he noticed the appearance of a dark
maroon urine. His blood pressure is 148/107
mm Hg. Laboratory results reveal the
following:
Creatinine = 2.6 mg/dL
BUN = 36 mg/dL
Albumin = 4.1 g/dL
Urine analysis shows a small amount of protein
but many red cells.
Nephritic Syndrome
• Typically there is injury to the endothelium or the
basement membrane that results in an active
inflammatory response.
• The significant fall in GFR is due to the decrease in
surface area available for filtration because of closure
of capillary lumens by the inflammatory response.
• Sodium retention can lead to hypertension.
• As a result of the inflammation of the capillary
endothelium, the membrane system fails to act as an
effective filtration barrier to blood cells and protein.