PC Mod 5 - PC617StudyGuides
advertisement

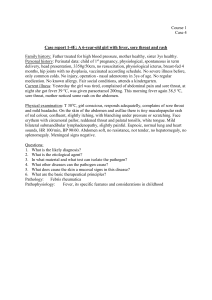
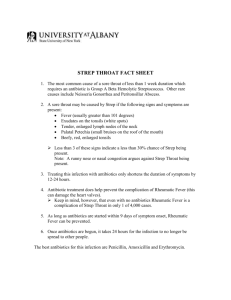
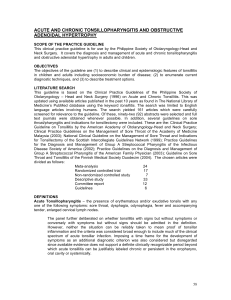
EXAM 3 Study Guide Module 5 Common Eye Problems Blepharitis Doug is a 68 year old single, homeless man who is being examined before entering a shelter. The NP discovers that in addition to mild seborrhea, Doug has an inflammation of his eyelids that affects only the eyelash hair follicles. There is no ulceration or masses in the eyelids and the pre-auricular lymph nodes are non-palpable. How should Doug’s eyes be treated since there is no infection? What solution can be used for lid scrubs for this patient? Is his condition infectious? Will he be allowed to enter the shelter? Hordeolum Maria is a 21 year old Latina who is 14 weeks estimated weeks gestation (EGA) in her third pregnancy. During her prenatal visit today the CNM notices that she has a hordeolum that points to the lower lid margin of her right eye. 1. What additional history does the CNM need in order to safely treat the hordeolum? Onset, duration, had before?, remedies tried, current meds, allergies 2. Describe pharmacologic management of this common eye lesion. Tobramycin, or if frequent problem or does not respond to therapy use Ofloxacin or ciprofloxacin drops Use 4 times daily for one week. 3. How would the management change if the lesion was a chalazion? Steroid injections sometimes needed to resolve. 4. Maria speaks Spanish and does not understand English. Using an interpreter, what are the most important aspects of self-care education related to the eye lesion? Use warm, moist compresses 3-4 times daily. Use antibiotics as prescribed for the full course. Discard all eye and face makeup, opened contact lens solution and used cases because it could be contaminated and reinfection can occur. Conjunctivitis Rebecca S. is a 30 year old single mother of two who works in an auto parts store. She is complaining of bilateral red eye. The problem developed two days after her son, Johnny, was sent home from school with “pink eye”. 1. What further subjective data (history) do is needed? 2. Describe the ocular examination to be conducted. What would be the rationale for palpation of the pre-auricular lymph nodes? Does visual acuity need to be tested? 3. Rebecca has a viral conjunctivitis. How should this be treated? 4. Describe the education Rebecca needs concerning viral conjunctivitis. Hunter with an eye complaint Martin H., a 47 year old, has come to the clinic from a hunting trip where a tree branch, “got me in the eye”. He is tearing and holds the right eye closed. “It feels like I have grit in my eye.” 1. Describe the physical examination that needs to be done, including all the steps to fluorescein staining. (see Medline Plus Medical Encyclopedia for this information. Retrieved 7/13/07 http://www.nlm.nih.gov/medlineplus/ency/article/003845.htm A piece of blotting paper containing dye will be touched to the surface of the eye. Ask pt to blink, blink spreads the dye around and coat the “tear film” (oil, water, and mucus that protects and lubricates the eye) covering the surface of the cornea. Blue light is directed at eye and problems on the surface of the cornea will be stained by the dye and appear green under the blue light. Likely cause of the cornea problem can be determined depending on the size, location and shape of staining Prepare for test by asking pt to remove contact lens If eye are dry the paper may be scratchy. The dye may cause a mild and brief stinging sensation Test is used to reveal scratches or foreign bodies Normal result dye does not adhere to the eye itself but stays on the tear film Abnormal results: o Corneal abrasion (scratch) o Foreign bodies (eyelash or dust) o Infection o Injury or trauma o Severe dry eye associated with arthritis Risks-may touch skin and cause slight, brief discoloration 2. The NP determines that there is a small corneal abrasion in the lower portion of the right cornea. Is it appropriate to treat this minor abrasion in the primary care setting? Yes, if not improving or healed within 1 to 2 days refer. 3. How should Martin’s small corneal abrasion be managed? As a mild bacterial conjunctivitis. 4. What is the follow-up plan for Martin? RTO in 2 days or earlier if there is increase in pain, purulent drainage, redness or decreased vision. Under what conditions would Martin be referred for care? Abrasion not healed in 1 to 2 days. 5. Should Martin's eye be patched? Why or why not? No, Patching does not hasten healing time, lesson pain or decrease repost of blurred vision. Compliance with medication is increased if eye is not patched. Emergent Eye Conditions 1. Describe signs and symptoms of Iritis uveitis angle-closure glaucoma. 2. Describe ciliary flush (AKA limbal flush). 3. How should these conditions be managed by the APN? Common Ear Problems Auricular Disorder Jessica, age 21, has a problem with her newly pierced ears. She tells the NP that she thought the drainage from the piercing would have stopped after a couple of days. On examination, the NP determines that the piercings may be mildly infected. 1. What two treatments may be recommended for Jessica? Alcohol and antibiotic ointment (erythromycin) 2. What is the best follow-up plan for Jessica? RTC if symptoms worsen. ??? This wasn’t really touched on. Otitis Externa Chloe, age 19, is complaining of ear fullness and pain. It began about a week ago with her ear itching so she used a q-tip to clean her ear. Now it is painful, she is having some difficulty hearing and feels slightly dizzy. There has been discharge, but it is clear and odorless. On physical examination Chloe is afebrile. There is tenderness on movement of the tragus and pinna and the auditory canal appears inflamed and swollen. 1. Outline the rest of the history and physical examination needed for this patient. 2. What is the diagnosis? 3. How is this condition best treated? 4. Discuss the patient education needed? 5. What is the best follow-up plan for this patient? 6. Under what conditions would Chloe be referred to an MD? 7. What are the outcome criteria for evaluating the care given to Chloe? Otitis Media David, age 18, has been having “a cold.” He has been very congested. Last night he awoke with his right ear hurting and “throbbing.” The NP performs an otoscopic examination and determines that he has a right otitis media. 1. What otoscopic findings would indicate that this is an otitis media? (Please write this as you would in the chart notes.) TM red and bulging 2. What is the best pharmacologic management for this problem? Tylenol and NSAIDS for pain. If antibiotics are indicated Amoxicillin should be used if no allergies to PCN 3. What should the patient education for David include? If smoker, cessation Avoid exposure to second hand smoke Not infectious If using antibiotics, proper administration RTO in no improvement in 48-72 hours Follow up in 14 days if responding to treatment Two days later, Dave calls asking to be seen. The ear is hurting again after only one day of some relief. 1. What could be the reason that Dave's infection is not getting better? Possible amoxicillin resistance 2. How will the management of Dave’s complaint change at this time? Change antibiotic to Augmentin XR 3. What is the best follow-up plan for Dave? Follow up in 2 weeks 4. At what point should Dave be referred to ENT Specialist? Explain. Not responding to therapy. 5. Write a brief referral note to this ENT physician as you might do in clinical practice for a patient with otitis media and serous otitis that are not responding to treatment. Request for urgent referral for patient to be seen by Dr. Nosy ENT for Otitis media (or serous oritis) not responding to primary and secondary antibiotic therapy. Common Nose Problems Rhinitis Billy Bob T., age 25, has an itchy, runny nose and sneezes a lot. It is worse every year in May when the trees bloom. You suspect allergic rhinitis. 1. What physical findings will confirm your preliminary diagnosis? 2. What additional history do you need in order to properly treat Billy Bob? Be sure to rule out the historical factors that would indicate an alternate cause for his rhinitis. 3. Billy Bob loves his dog and is not willing to give him up. What are some things he can do with “Buddy” that will decrease doggy allergens? 4. What pharmacologic interventions do you suggest for Billy Bob? (Hint: Level 4 evidence demonstrates that intranasal corticosteroids are more effective than antihistamines.) 5. The down side…what are the potential side effects of nasal corticosteroids and how long will it take for the symptoms to be relieved? Epistaxis Nine year old Jeff has a seemingly spontaneous nosebleed and his mother calls the NP asking how to deal with it. 1. Where in the nose do most spontaneous nosebleeds originate? Kiesselbach’s plexus, a vascular plexus on the anterior nasal septum, and is associated with irritated mucous membranes and trauma. What is the usual cause of anterior and posterior epistaxis? Anterior nosebleeds are usually caused from irritation and trauma. Posterior nosebleeds occur within the posterior branches of the sphenopalatine artery and are idiopathic or associated with vascular disease and can be difficult to control. 2. What is the first step in stopping a nosebleed? Have pt sit in upright position, lean forward to decrease swallowing blood and apply direct pressure to the anterior portion of the nose for a minimum of 10 minutes. 3. How should Jeff sit while waiting for the bleeding to stop? Upright and leaning forward postion. 4. What key components of patient education are needed by Jeff and his mother? After bleeding stops Jeff should avoid vigorous exercise for several days. If bleeding reoccurs in the in the next 72 hours call healthcare provider Avoid tobacco, hot, spicy food that can cause vasodilation Avoid trauma~ do not pick nose :D Lubricate mucous membrane with Vaseline or bacitracin ointment Increasing humidity in home can help decrease irritation 5. Under what conditions should Jeff be brought to the emergency room? If bleeding is severe and does not stop within 30 minutes Jeff should be evaluated by a health care provider. Sinusitis Ms. Jones is a 40 year old history teacher who comes to clinic complaining of a frontal headache, nasal congestion, yellowish nasal drainage, and a temperature of 100* F. Her symptoms began about a week after she first noticed “cold” symptoms and have steadily worsened. The headache worsens when she bends forward. 1. What additional history is needed and why? 2. Describe the focused physical examination for Ms. Jones. 3. Your diagnosis is sinusitis. Describe your treatment for this patient. Will you include sinus washes? If so, how is this done? Will you include an antibiotic? If so, what antibiotic will you use – give the dosage, timing of doses, and duration of therapy for Ms. Jones. 4. Ms. Jones returns in 5 days telling you that she was better for a couple of days but is getting worse again. How will your change your treatment? (consider lactimase producing bacteria or other forms of resistance) 5. When Ms. Jones recovers, she may benefit from neti, a Yoga method for prevention of post-nasal drip and sinusitis. Describe how this is done. Common Throat and Mouth Problems Pharyngitis and Tonsillitis Stephen is a 16 year old who is being seen today because of sore throat and a temperature of 101*F. His mother tells you that he was complaining of his throat when he came home from school yesterday and has steadily gotten worse. 1. What further history do you need? Does pt have rhinorrhea, cough, hoarseness, headache, watery eyes, sneezing, nausea, abd pain, conjunctivitis, myalgias? History of strep? Exposure to environmental irritants that may have been inhaled? Current medication? Allergies? Anyone else in home or friends at school been sick? What will you include in your review of systems? 2. There are several etiologies for sore throat. Give physical findings for viral pharyngitis, infectious mononucleosis, and GABHS infection. 3. Vital signs Eyes-drainage Ears-TM for otitis media Nose-drainage, turbinate (suggest allergies) Facial sinuses tenderness for possible URI Throat/Neck-tonsil size, erythema, exudates, uvula swelling, swollen, tender lymph nodes Chest/lungs-congestion, rhonchi, wheezes Heart-murmur Abdomen-bowel sounds, tenderness, hepatomegaly and splenomegaly (later symptoms of Mono) Skin-rashes Viral Pharyngitis o Mild erythema with little or no pharyngeal exudates o Pharynx may appear swollen, boggy or pale Infectious mononucleosis o Pharyngeal erythema o Tonsillar hypertrophy o White to gray-green exudates o Petechiae at the junction of the hard and soft palate o Posterior cervical adenopathy o Hepatomegaly and splenomegaly GABHS infection o Marked erythema of the throat and tonsils o Patchy discrete white and yellowish exudates o Tender anterior cervical adenopathy o Pressure on the tonsillar pillars may produce purulent drainage o Uvula may be edematous o Fever greater than 101 o Occasionally GABHS may be seen erythematous, persistent sore throat with little fever and no exudates What diagnostic studies will you do? Why? Rapid antigen detection test (RADT) for GABHS. If neg RADT and GABHS is still suspected throat culture is performed for confirmation. CBC often reveals leukocytosis with GABHS. 4. If Stephen has GABHS pharyngitis – what will be his treatment? 5. What if he is allergic to penicillin? 6. Erythromycin or zithromax If Stephen has viral pharyngitis, what will be his treatment? 7. Pen VK QID for 10 days Rest Fluids humidification voice rest warm saline gargles for comfort Tylenol and Motrin for fever and discomfort Topical sprays and throat lozenges Under what conditions would you refer Stephen for emergency treatment? Difficulty breathing Allergic reaction to medication such as 8. Uticaria shortness of breath wheezing tightness in the chest What are the complications of GABHS pharyngitis? Upper airway obstruction Sleep apnea Sleep disturbances Peritonsillar cellulitis Abscess Retropharyngeal abscess Scarlet fever Acute rheumatic fever Poststreptococcal glomerulonephritis Which one of these complications may occur even if Stephen is properly treated? Poststreptococcal glomerulonephritis 9. What education (treatment and health promotion) is important for Stephen and his family? Importance of adhering to antibiotic therapy Pt infectious until 24 hours after start of antibiotics Full course of antibiotics is needed to prevent reinfection or complications Side effects of antibiotic therapy o Allergic reactions o Nausea o Vomiting o Diarrhea o Abd pain o Lethargy o Secondary yeast infection o Vaginitis (in women) 10. If Stephen has GABHS, how soon after beginning therapy will he feel better? 24-48 hours after the start of antibiotic therapy Aphthous Ulcer Eddie, a 30 year old African American, has developed a single, painful mouth sore during the last 2 days. He has never experienced anything like this before. He denies use of tobacco in any form, alcohol or illicit drugs. He is normally healthy and takes no medications. 1. What further history is needed? 2. Describe the physical findings if Eddie has an aphthous ulcer. 3. How are aphthous ulcers treated? Are they likely to recur? Stomatitis and Glossitis Grace, a 67 year old female who is taking chemotherapy for chronic lymphocytic leukemia, complains of sore, dry mouth and loss of appetite. She is unable to wear her dentures. On examination, her mouth and tongue are red, the tongue is swollen, and the corners of her mouth are fissured. The NP determines that Grace has oral candidiasis secondary to her lowered immune status. 1. What is the best choice for medication for the stomatitis and glossitis? Nystatin oral syspension 2. What is the recommended topical medication for the angular stomatitis? Acemannan oral gel prn to sooth irritated tissue. ???? 3. Describe the patient education needed including the use of the medications prescribed. 4. Nystatin swish and swallow 4 times daily for 48 hours after the lesions have resolved OR Nystatin powder applied to dentures 3-4 times daily. In not responding to therapy notify care provider Avoid irritants like hot food, beverages and chemicals. Iron supplement (?) d/t chronic lymphocytic leukemia Report S&S of stomatitis or glossitis immediately What is the best follow-up plan for Grace? Monitor frequently for sign and symptoms of thrush and treat accordingly 5. List the outcome criteria for evaluating your care for Grace. Relief of symptoms Infectious Mononucleosis Becky is a 16 year old who is complaining of sore throat, fever, and "swollen glands". She is concerned that she may have mononucleosis since several of her cheer leading friends are sick with it. 1. Describe the history and physical examination the CNM will conduct. 2. What diagnostic test is the most useful in diagnosing mononucleosis? 3. Describe the best management plan for Becky. 4. Describe the education Becky and her family will need. 5. What are some indications for referral when a teen ager has mononucleosis?