Umetsu - Stanford University
advertisement

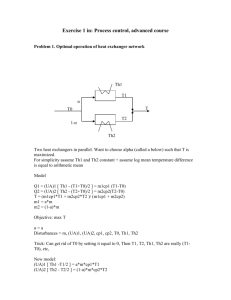
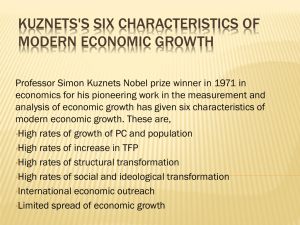
Advanced Immunology Th Cell Subsets and Cytokines Dale T. Umetsu, MD, PhD Stanford University February 26, 2003 Humoral immunity is essential for the elimination of extracellular bacterial infections www.cellsalive.com Bacteria are opsonized with antibody and complement Cellular immunity is required for infections with intracellular pathogens Reciprocal relationship between humoral and cellular immunity Humoral immunity Cell mediated immunity Dose of Flagellin Parish and Liu, 1972 Adaptive Immunity Humoral Immunity (CD4) (extracellular organisms) – IgG, IgA, IgM, IgE Cell-mediated Immunity (intracellular organisms) – Delayed type hypersensitivity (CD4) – Cytotoxic responses (CD8) Th Cell Subsets and Cytokines Characteristics of Th1/Th2 subsets. Situations in which Th subsets are important. How these subsets arise and differentiate. Modifications of the Th1/Th2 paradigm. – Related T cell subsets – Regulatory T cell subsets. Expression of cytokines by CD4 T cell subsets Cytokine IFN-g Lymphotoxin IL-2 IL-3 GM-CSF TNF-a IL-4 IL-5 IL-9 IL-10 IL-13 Th1 Th2 Th0 Thp + + + + + + - + + + + + + + + + + - + + + + + - Effector Functions of Th1 Cells IFN-g IFN-g IFN-g 1 IFN-g IgG2a, IgG3 Effector Functions of Th2 Cells Generation of Th Cell lines Isolate clonotypic CD4+ T cells DO11.10 OVA-specific TCR Tg OVA + APC rIL-12 Anti-IL-4 mAb Th1 OVA + APC rIL-4 Anti-IL-12 mAb Th2 OVA + APC rIL-4 rIFN-g Th0 Markers of Th1 and Th2 Cells Th1 Th2 IFN-g IL-12R2 IL-18R P- and E- selectin receptors CXCR3, CCR5 IL-4 IL-1R, IFN-g receptor T1/ST2 (homolog of IL-1R) Tim3 Tim1 ICOS Stat6, GATA-3, c-maf Stat4, T-bet CCR4, CCR8 TIM family of genes TIM-1 encodes a 305 aa protein, regulates the development of asthma and allergy (McIntire, et al. 2001. Nature Immunol. 2:1109) (McIntire, et al. 2003. Nature 425:576) . In mice, TIM-3 encodes a 281 aa protein, regulates the development of autoimmune diseases (Monney et al. 2002. Nature. 415:536). TIM-1 is preferentially expressed in Th2 cells. TIM-3 is preferentially expressed in Th1 cells (Sanchez-Fueyo, et al. Nature Immunol. Oct 2003). TIM: T cell, Immunoglobulin domain, Mucin domain. Infection with Leishmania Strain result cytokines produced C3H/HeN resistant IFN-g, IL-2 BALB/c IL-4, IL-5, IL-13 susceptible Disease States Attributed to an Imbalance in Th1/Th2 Cells Over production of Th2 cytokines Infections Leishmania TB, leprosy Fungal infection HIV Allergy and asthma Ulcerative colitis Over production of Th1 cytokines Autoimmune diseases Multiple sclerosis Rheumatoid arthritis Diabetes mellitus Crohn’s disease Graft rejection Recurrent abortions (Helminth infection) T Cell Subsets: when are they important? During chronic antigen stimulation – Chronic infection – Chronic response to auto antigens. – Chronic exposure to allergens. Not following a single antigenic stimulation, not with fulminant infections. Th1 Cells Cross Regulate Th2 Cells Th1 cytokines IL-2 IFN-g IL-12 IL-4 IL-10 Th2 cytokines IL-4 IL-5 IL-13 IL-12 IFN-g What are the instructive signals for the development of Th1/Th2 cells Cytokine microenvironment Antigen dose/TCR signaling – Altered peptide ligands APC type – Route of antigen administration Costimulatory signals Host genetic factors Signals that influence Th1 differentiation IL-18 CD8a+ DC B7.1, DC1 (human) IL-12 IL-12, TGF- IFN-g IL-4, IL-10, TGF- inhibits IL-27 Heterodimeric cytokine, related to IL-12. p28 (IL-12p35-related) + EBI3 (IL-12p40related) = IL-27. Long chain four-helix bundle cytokine. Early product of activated APC. Drives expansion of naïve but not memory CD4 T cells. Synergistic with IL-12 in triggering IFN-g production in naïve T cells. Pflanz et al. 2002. Immunity. 16:779. IL-23 p19 subunit + IL-12 p40 subunit = IL-23 IL-23 binds to IL-12R1 + another novel subunit. Produced by activated dendritic cells. Induces proliferation and IFN-g production by memory (Th1) cells. Some shared activities with IL-12 (p35/p40). Oppmann et al. 2000. Immunity. 13:715 Signals that influence Th2 differentiation TSLP (humans) Humoral responses Allergic responses B7.2, OX40L, ICOSL CD8a- DC, DC2 (human) IL-12, IL-18, TGF- inhibits IL-25 Related to IL-17. Produced by Th2 cells. Induces production of IL-4, IL-5, IL-13, eotaxin, and increases IgE, IgG1, eosinophilia. Induces IL-13 and IL-5 from accessory cell population. Affects lungs, GI tract; effects dependent on IL4Ra signaling. Fort et al. 2001. Immunity. 15:985 Thymic Stromal Lymphopoietin (TSLP) Short-chain four a-helical bundle cytokine. Produced by human epithelial cells. Binds to TSLPR + IL-7Ra. Activates DCs, which then induce Th cell production of IL-4, IL-5, IL-13, reduces production of IL-10 and IFN-g, and induces production of Th2 attracting chemokines. Highly expressed in skin of patients with atopic dermatitis. Soumelis et al. 2002. Nature Immunol. 3:673 Role of Immature Dendritic Cells CD8a CD40 CD86 Anergy ICOS-ICOSL pathway ICOS is the third member of the CD28 family. – Expressed on activated T cells (particularly on Th2 cells). ICOS binds to ICOS-ligand (B7h, B7RP-1, B7-H2). ICOS upregulates CD40L. – Important for isotype switch. ICOS engagement promotes Th cell differentiation and effector function – Induces IL-4, IL-5, esp. IL-10 APC production. – Also important for tolerance induction. T Cell Nature Rev. Immunol. 2002. 2:116. Inhibitory receptors may influence Th cell differentiation B7 binds CTLA-4. PD-L1 (B7-H1) and PD-L2 (B7-DC) bind to PD-1. PD-1-/- mice develop SLE glomerulonephritis. B7x (B7-H4) binds to BTLA, the 5th member of the CD28 family. BTLA-/- mice develop enhanced sensitivity to EAE. B7-H3 (inhibitory pathway) B7x BTLA B7-H3 APC T Cell Nature Rev. Immunol. 2002. 2:116. Tc1 and Tc2 Polarized CD8 Cells CD8 cells cultured with IL-12 produce IFN-g. CD8 cells cultured with IL-4 produce IL-4 and IL-5, IL-10 and some IFN-g. – CD8 cells make 100 fold less IL-4 than CD4 cells. – CD8 cells make 3-5 fold less IL-5 than CD4 cells. Tc1 CD8 but not Tc2 effector cells protect against viral infection. Croft et al. 1994.. J Exp Med. 180:1715. Cerwenka et al. 1999. J Exp Med. 189:423 Be1 and Be2 Polarized Cell Subsets Harris et al. 2000. Nature Immunol. 1:465. Signals that influence Th differentiation NK T cell NK T cell eosinophil iNKT Cells Express cell surface markers characteristic of both NK cells and conventional T cells. In mice, most NKT cells express an invariant Va14Ja18 TCR (Va14 iNKT cells) (Va24Ja15 in humans). Recognize glycolipid antigens presented by the MHC class I protein, CD1d. When activated, NK T cells rapidly produce large amounts of IL-4 and IFN-g. NKT cells regulate the development of autoimmune diseases, such as diabetes, EAE, cancer and asthma. NKT Cells in Autoimmunity (tolerance?) and Cancer Type 1 diabetes – Reduced number of NKT cells in NOD mice and patients with diabetes. – Treatment of NOD mice with aGalCer protects. EAE – Treatment with aGalCer protects, but not in IL-4-/- or IL-10/- mice. – Reduced number of NKT cells in MS patients. Tumor immunity – Lack of iNKT cells increased tumor metastasis (melanomas and hepatomas). – In one system, IL-13 production by NKT cells inhibited tumor immunity. NK T Cell Subsets CD4+ NK T cells produce IL-4, IL-5, IL-13, IFN-g CD4- CD8- NK T cells produce IFN-g Gumperz et al. 2002. J Exp Med. 195:625. NKT Cells are Required for Oxazolone Colitis, a Th2 Colitis Model Immunity. 2002. 17:629. NKT Cells are Required for the Development of AHR 10 BALB/c PBS BALB/c OVA 7.5 CD1 KO PBS PenH CD1 KO OVA 5 2.5 0 0 10 20 30 40 50 Methacholine (mg/ml) Akbari. Nature Medicine. 2003. 9:582. NKT Cells Bridge Innate and Acquired Immunity Transcription factors that influence Th differentiation Pearce, EL et al. 2003. Control of effector CD8 T cell function by the transcription factor eomesodermin. Science 302:1041. Agarwal, Rao. 1998. Immunity. 9:765 Acylated histones Normal inactive chromatin (ground state) nucleosome DNA Stat6, GATA3 Monoallelic Gene Expression IL-4 Gene Allele 1 activation sustained activation Allele 2 Both alleles inactive One allele expressed (monoallelic expression) Both alleles expressed Genetic Effects Individuals differ in their susceptibility to autoimmune disease, infection, and allergic disease. Susceptibility is in part regulated by differences in the capacity to generate Th1 or Th2 cytokines. Susceptibility genes are identified by DNA sequence differences between individuals (humans) or strains (mice). Some Gene Polymorphisms Affecting Cytokine Production IL-4 receptor a (SNPs present in coding region). IL-13 (SNPs present in coding region) MHC linked to some autoimmune diseases. NOD2 linked to Crohn’s disease (LPS receptor) (Nature 2001. 411:603). CTLA-4 alternative splice form (chromosome 2q33) (Graves disease, hypothyroidism, type 1 diabetes). (Nature 423:506) TIMs (Nature. 2003. 425:576) Th1(5x106) Th2 (5x106) Th1(0.2x106) Th2(0.2x106) Lafaille, et al. J. Exp. Med 186:307, 1997. Induce Th2 response Control Attempts to tolerize with MOG results in exacerbation. Genain, et al. 1996. Science. 274:2054 Transfer of diabetes with both Th1 and Th2 cells Pakala, et al. 1997. JEM. 186:299. Th1 cells do not inhibit Th2 cell-induced airway hyperreactivity 800 transferred cells: 600 % above baseline Th2 Th1+Th2 (1:1) 400 Th1+Th2 (2:1) Th1 200 none 0 0 10 20 30 Methacholine (mg/ml) 40 50 Hansen, et al J.C.I. 1997 The Th1/Th2 Paradigm and Disease Regulation Both Th1 and Th2 cells can cause disease. The “opposite” of a Th1 cell is not always a Th2 cell. The Th1/Th2 paradigm cannot fully explain immune regulation in all situations. Additional regulatory cells must exist to regulate immune responses. Other CD4 Subsets that “Regulate” Th3 CD4 + CD25+ cells TR1 TR NKT cells Th3 Cells Generated by oral tolerance induction with low dose antigen. Produce TGF-, IL-4 Express regulatory/suppressive activity. TGF- production may be enhanced by cross-linking of CTLA-4. Chen, Y, et al 1994. Regulatory T cell clones induced by oral tolerance: suppression of autoimmune encephalomyelitis. Science 265:1237. MBP specific Th3 Cells Inhibit EAE Th3 cells + anti-TGF Th3 cells Science. 1994. 265:1237. low CD45RB Cells, CD25+ Cells CD25+ (IL-2Ra-chain), CTLA-4, GITR, foxp3. When transferred, have strong regulatory/suppressive activity for colitis, diabetes, thyroiditis. Appear to require TGF-, IL-10 and CTLA-4 to function. In vitro activity depends on cell contact. Antigen specificity? Tr1 Cells Develop after stimulation with IL-10. Produce IL-10, IL-5, (TGF-). Low proliferative capacity. Inhibitory for experimental colitis. Anti-IL-10 mAb reverses inhibitory effect. Groux et al. 1997. Nature. 389:737. Intracellular staining tin -a c 10 IL- A OVA( i.p.+i.n.) RN tin -a c 10 IL- RN A tin -a c 10 IL- IL- OVA-Alum i.d. PBS i.n. A 10 -a cti n RN A OVA i.n. RN a DCs from mice exposed to i.n. OVA produce IL-10 Intracellular staining 33% 2 .3 % IL-1 0 Akbari, et al. 2001 Nature Immunol. IL-10 producing DCs induce development of T cell lines producing IL-10 IL-10 IL-4 IFN-g Akbari, et al. 2002, Nature Medicine Summary-T cell subsets A major theme in immunology, and documented feature of the immune system. Subsets of T cells express restricted cytokine profiles Cells with restricted cytokine profiles (CD4, CD8, NK, NK T, B) have distinct effector functions and regulate immune responses. Questions that remain What regulatory cells “balance” Th1 and Th2 cells? What downregulates polarized responses? How Th subsets are involved in tolerance? What additional molecular mechanisms regulate cytokine synthesis? Are there Th2 PAMPs? What activates NKT cells? What are the host/genetic factors that regulate cytokine production? References Hawiger D, Inaba K, Dorsett Y, Guo M, Mahnke K, Rivera M, et al. Dendritic cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. J Exp Med 2001; 194:76979. Steinman R, Hawiger D, Nussenzweig M. Tolerogenic dendritic cells. Annu Rev Immunol 2003; 21:685-711 Sharpe AH, Freeman GJ. The B7-CD28 superfamily. Nat Rev Immunol 2002; 2:116-26. Weiner HL. The mucosal milieu creates tolerogenic dendritic cells and Tr1 and Th3 regulatory cells. Nature Immunol. 2001; 2:671-2. Hori S, Nomura T, Sakaguchi S. Control of Regulatory T Cell Development by the Transcription Factor Foxp3. Science 2003; 299:1057-61. Pasare C, Medzhitov R. Toll pathway-dependent blockade of CD4+CD25+ T cell-mediated suppression by dendritic cells. Science 2003; 299:1033-6. Wilson SB, Kent SC, Patton KT, Orban T, Jackson RA, Exley M, et al. Extreme Th1 bias of invariant Va24JaQ T cells in type 1 diabetes. Nature 1998; 391:177-81. Wakkach A, Fournier N, Brun V, Breittmayer JP, Cottrez F, Groux H: Characterization of dendritic cells that induce tolerance and T regulatory 1 cell differentiation in vivo. Immunity 2003, 18:605617. References Heller F, Fuss I, Nieuwenhuis E, Blumberg R, Strober W. Oxazolone colitis, a Th2 colitis model resembling ulcerative colitis, is mediated by IL-13-producing NK-T cells. Immunity 2002; 17:629-38. Terabe M, Matsui S, Noben-Trauth N, Chen H, Watson C, Donaldson D, et al. NKT cellmediated repression of tumor immunosurveillance by IL-13 and the IL-4R-STAT6 pathway. Nat Immunol 2000; 1:515-20. Ansel KM, Lee, DU, Rao A. An epigenetic view of helper T cell differentiation. Nature Immunol. 4:616. Shimizu J, Yamazaki S, Takahashi T, Ishida Y, Sakaguchi S: Stimulation of CD25(+)CD4(+) regulatory T cells through GITR breaks immunological self-tolerance. Nat Immunol 2002, 3:135-142. Levings MK, Sangregorio R, Sartirana C, Moschin AL, Battaglia M, Orban PC, Roncarolo MG: Human CD25+CD4+ T suppressor cell clones produce transforming growth factor beta, but not interleukin 10, and are distinct from type 1 T regulatory cells. J Exp Med 2002, 196:1335-1346.