Allergy PPT
advertisement

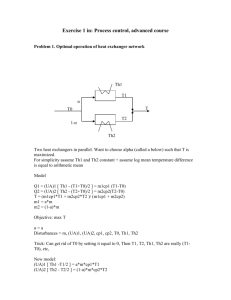
Mechanisms of Allergic Immunity crah1@le.ac.uk Normal larynx Laryngeal oedema Cellular culprits of allergy: Mast cells • Most informative early analysis conducted in patients with asthma • Early studies (pre-1980) implicated mast cells and histamine as part of an archetypal immediate type I hypersensitivity • Provoked by allergenic and non allergenic substances • Explained atopic and non-atopic asthma • Explained why mast cell stabilising drugs worked Cellular culprits of allergy: Mast cells?? • Corticosteroid treatment worked, but had no effect on histamine release • Anti-histamine treatment had little effect on asthma • Could not explain ‘organ specificity’ of asthma • Could not explain the hyperresponsive airway in asymptomatic asthmatics • Fibreoptic bronchoscopy - immunohistology, biopsy and analysis of bronchoalveolar lavage (BAL) cells (1980’s - present) Cellular culprits of allergy: T cells The early evidence: • Eosinophil & mononuclear cells infiltrate the bronchi of asthmatics • Activated T cells elevated in the peripheral blood of severe acute asthmatics • Activated T cells in peripheral blood correlated with airway narrowing • Bronchial CD4 lymphocyte numbers correlated with eosinophil numbers • Elevated IL-5 expressing T cells in asthmatic bronchial mucosa and BAL • T cells that release IL-5 co-localise with eosinophils • Eosinophils cause airway hyperresponsiveness, inflammation desquamative bronchitis, mucous hypersecretion and smooth muscle contraction • IL-5 promotes differentiation and regulates the survival of eosinophils • Steroid treatment associated with a decrease in IL-5 producing cells Cellular culprits of allergy: T cells Wider analysis of cytokines in atopy showed that BAL T cells that expressed elevated levels of IL-5, also expressed IL-4 - a profile typical of Th2 cells in mice IL-3 Growth of progenitor haemopoeitic cells GM-CSF Myelopoiesis. IL-4 IL-5 IL-10 TGF- B cell activation and growth IgE isotype switch. Induction of MHC class II. Macrophage inhibition Eosinophil growth IL-6 B cell growth Acute phase protein release Inhibits macrophage activation Inhibits Th1 cells Inhibits macrophage activation Th2 Lebman & Coffman 1988 J Exp Med 168, 853-862 ‘Textbook’ scheme of allergic immunity is centred around polarised Th cells -ve Ig isotype switch Th2 B Th1 -ve Differentiation and development IgE MF Mast cell Eosinophil Where do Th2 cells come from? Why are they so dominant in allergic individuals? What are they really for? The discovery of Th1 and Th2 subsets Journal of Immunology 136, 2348-2357 1986 In vitro - Th1 and Th2 subsets T cell clones that make IFN-g, but not IL-4 Do not provide help to IgE and IgG1 secreting B cells T cell clones that make IL-4, but not IFN-g Provide help to IgE and IgG1 secreting B cells Enhances IgE & IgG1 IFN-g IL-4 Relevance in vivo - Infection Non-healing BALB/c Resistant C57BL/6 Draining LN T cells express IL-4 mRNA Draining LN T cells express IFN-g mRNA Irradiated BALB/c recipient T Leishmania specific T cells Resistance Reiner & Locksley Annu. Rev. Immunol. 13, 151-177, 1995 Relevance in vivo - Infection IFN-g / IL-12 or anti-IL-4 Pro-Th1 treatments or anti-Th2 treatments protect against infection Leishmania resistance - mechanism IFN-g Th1 Inflammatory Th1 T cell Macrophage and Leishmania Macrophage infected with Leishmania kills pathogen when activated Macrophage activation is dependent upon Th1 cells Relevance of Th subsets in humans Lepromatous and tuberculoid leprosy Infection with Mycobacterium leprae shows two main clinical forms associated with Th1 and Th2 responses Tuberculoid leprosy Lepromatous leprosy Low infectivity Localised infection Normal serum Ig Normal T cell response High infectivity Disseminated infection Hypergammaglobulinaemia Unresponsive Th1 Poor growth of mycobacteria in macrophages Th2 Florid growth of mycobacteria in macrophages Tuberculoid leprosy Lepromatous Leprosy ‘Textbook’ scheme of allergic immunity is centred around polarised Th cells Immunological fashions •1960’s & 1970’s Immunoglobulin E •1970’s & 1980’s Mast cells & Eosinophils •1980’s & 1990’s Environment – ante-natal & adult, allergens, Th2 cells •1990’s & 2000’s Microbial experience, Epithelium, Tregs Although undoubtedly a useful model, the textbook ‘skew to Th2’ model is too simplistic to explain allergy Allergy is a disease of impaired immune regulation Where is the regulatory lesion? Allergic immune responses are much like any other immune response and involves the same regulators Non self protein from allergen or pathogen Barrier: Skin, gut, lung, eye, nose etc Inflammation inc. MIP-1a, MCP-1 MIP-1 Activation and migration of dendritic cells to site of inflammation Tracheal Dendritic Cells Langerhan’s cells In-vitro differentiated monocyte-derived Dendritic Cell Migration of immature DC to sites of inflammation Sallusto et al., Eur. J. Immunol. 1998 28 2760-2769 Immature DC migrate into inflamed tissue in response to MIP-1a, MCP-1 MIP1- which bind to, and trigger CCR1, CCR2 and CCR5 respectively. [Ca2+]i Time (s) Immature DC do not respond to the lymph node derived CCR7 ligand MIP-3 [Ca2+]i [Ca2+]i Time (s) Time (s) Migration of mature DC to 2º lymphoid tissue Sallusto et al., Eur. J. Immunol. 1998 28 2760-2769 Mature DC stop migrating into inflamed tissue and make no response to MIP-1a, MCP-1 MIP1- [Ca2+]i Time (s) Mature DC respond to the lymph node derived CCR7 ligand MIP-3 [Ca2+]i [Ca2+]i Time (s) Time (s) DC – T cell interactions in the lymph node Mempel, T.R et al Nature 427: 154-159, 2004. Anti OVA 323-329 TcR transgenic mouse Pulsed with Ag OVA 323-329 DC labelled RED Splenic DC Not pulsed with Ag T cells labelled GREEN Imaging at various timepoints -18hr 0hr 2hr Anti-L selectin Ab Early entry of DC to the lymph node Mempel, T.R et al Nature 427: 154-159, 2004. 1. DCs strategically cluster around HEV 18hr after entering the LN 2. Distribution of Ag-loaded DCs and T cells is ordered 4-5hr after T cells are injected 3. DC become highly migratory & change shape (20hr) 4. T cells cover large territories in LN 6. Short, serial T cell-DC contacts of ~ 5 minutes (2-4hrs after injection of T cells) 7. Stable T cell-DC conjugates of 30-180 minutes (8-12hr after injection of T cells) 8. Simultaneous stable and dynamic interactions between DC and T cells T cells start to proliferate and produce cytokines 44hr after transfer 5. 44hr after injection of T cells, DCs decrease motility and become anchored to reticular fibres, T cells rapidly migrate again More information than is provided by the antigen is exchanged between the DC and T cell DC have a profound influence on the properties of the T cell that develops Signals 1, 2 and 3 Signal 1 antigen & antigen receptor DC Th Signal 2 B7 - CD28 Costimulation Signals 1 & 2 activate T cells to proliferation and effector function But what ‘tunes’ the response to Th1 or Th2? Signal 3 - pathogen polarised DC Polarised DC subsets Signal 1 DC Th Signal 2 Signal 3 Th polarising signal Integration of signals from pathogen/allergen and the extracellular milieu polarise the DC to produce qualitatively different signals 3 The properties of the allergen, or allergen carrier influences the DC to drive the development of appropriate Th cells Microbial Patterns Janeway & Medzhitov 2002 Ann Rev Immunol 20 197-216 Pathogen-associated molecular patterns (PAMPS) • Conserved microbial molecules shared by many pathogens • Include: Bacterial lipopolysaccharides Peptidoglycan Zymosan Flagellin Unmethylated CpG DNA Pattern Recognition Receptors (PRR) • Include: Toll like receptors Receptors for apoptotic cells Receptors for opsonins Receptors for coagulation and complement proteins Type 1 and 2 DC Polarising PAMPS + + Type 1 PAMPS bind to PRR Th1 polarising factor IL-12 CD80/CD86 Class II CD40 Type 2 PAMPS bind to PRR Th2 polarising factor CCL2 (MCP-1) + T Type 1 PAMPS and their PRR Peptidoglycan (Gram + bacteria) Lipoproteins Lipoarabinomannan (Mycobacteria) LPS (Leptospira) LPS (Porphyromonas) Glycophosphatylinositol - (T. Cruzi) Zymosan (Yeast) dsDNA LPS Lipotechoic acid (Gram + bacteria) RSV F protein CD14 TLR 2 TLR 1 TLR 6 TLR 2 Low level IL-12p70 Some ligands induce IL-10 or IL-12p35 Unmethylated CpG DNA MD-2 TLR 3 TLR 4 TLR 9 High IL-12p70 IFN-a High IL-12p70 High IL-12p70 IFN-a Type 2 PAMPS and their PRR ? ? Endogenous molecular patterns Endogenous molecular patterns •Include: Heat shock proteins (HSP60 HSP70 GP96) Extracellular matrix proteins (hyaluronan, fibronectin, fibrinogen) Immune complexes Surfactant protein A Necrotic cell components Pattern Recognition Receptors (PRR) • Include: Toll like receptors Receptors for apoptotic cells Receptors for opsonins Receptors for coagulation and complement proteins Indirect activation of DC by ‘modulatory tissue factors’ Direct activation by PAMP-PRR interactions Allergen Necrotic/apoptotic cell death - neo expression of PRR ligands Heat shock proteins Extracellular matrix components Necrotic cell lipids Cytokines Chemokines Eicosanoids Coagulation components Complement components Activates the expression of costimulatory molecules on DC DC polarisation by modulatory tissue factors DC polarising factors IFN-g IFN-a IFN- Th0 to Th1 polarising cytokines IL-12p70 IL-27 TNF- IL-18 DC polarising factors CCL7 (MCP-3), CCL13 (MCP-4), PGE2, Histamine Th0 to Th2 polarising cytokines CCL2 (MCP-1), ?IL-4 Lack of high level IL-12p70 IL-27 TNF- IL-18 Could be argued that the development of Th2 cells is the default pathway Sources of modulatory tissue factors Viruses Fungi Parasites Bacteria Epithelium IFN-a IL-18 Th1 Viruses IFN-g NK Viruses Fungi Parasites Histamine Mast Th2 PGE2 CCR2L Viruses Fibroblast Explains how Th2 arise, but… …does not explains why some individuals are allergic and others are not and why the incidence of allergy is increasing. Reduced numbers of IL-12 producing cells? Reduced ability to produce or respond to IL-12? Reduced stimulation of IL-12 by microbial substances? The hygiene hypothesis (Strachan, 1989) Based upon the epidemiology of hay fever “Declining family size, improved household amenities, and higher standards of personal cleanliness have reduced the opportunities for cross-infection in young families families. This may have resulted in more widespread clinical young expression of atopic disease" ..can be interpreted in terms of a failure to microbially modulate default Th2 responses in childhood Neonatal & infant immune systems Serial infections Immune response Th1 Th2 Th2 Age The intrauterine environment is powerfully Th2 – this imprints Th2 dominance upon the neonate Balanced Th1/Th2 at ~2yr Delayed maturation of Th1 capacity Few serial infections – hygiene, small family size etc Immune response Th1 Th2 Age Longer period of time in which to make and establish Th2 responses to environmental antigens (i.e. allergens) Unbalanced Th1/Th2 Th2 dominance at ~2yr Do infections only reduce Th2 dominance by inducing Th1 responses? Aerosolised ovalbumin (OVA) Vaccinate with mycobacteria OVA – allergic mice with asthma-like symptoms Eosinophils in airway, dominance of OVA-specific Th2 cells, OVA-specific IgE No asthma-like symptoms Have the Th1 cells induced by the mycobacteria downregulated the activity of the Th2 responsible for the symptoms? Do infections only reduce Th2 dominance by inducing Th1 responses? Vaccinate with mycobacteria Th No asthma-like symptoms CD4+ cells specific for OVA that produce high levels of the immunosuppressive cytokines TGF and IL-10 Mycobacteria induced REGULATORY T cells Th cell polarisation DC mediated – decision influenced by infection Extracellular milieu - mediated Journal of Immunology 1994 152 4755-4782 0 1 10 Factor increase over control Priming conditions Control Ab Anti-IFNg Ab IL-4 + control Ab IL-4 + anti-IFNg Ab 0 1 10 Factor increase over control IFNg U/ml IL-4 pg/ml 5892 1534 1740 348 256 624 839 1245 IL-4 from the innate immune system IL-4 is not only a product of Th2 cells Resting Mast cell Degranulated mast cell Mediators released include: Leukotriene C4 & D4, Prostaglandin D2 Platelet Activating Factor, Chymase, Tryptase, Heparin, Histamine IL-4, IL-4, IL-5 IL-5, IL-6, IL-8, TNF-a Tryptase Sequential 2mm sections from a mucosal biopsy of a patient with asthma IL-4 Journal of Experimental Medicine, 1992 176 1381-1386 What properties and characteristics make a substance an allergen? How do these properties disregulate the processes described? L. destructor D. pteronyssinus D. pteronyssinus G. domesticus A. siro T. putrescentiae Allergens of Dermatophagoides pteronyssinus Der p 1 Der p 2 Der p 3 Der p 4 Der p 5 Der p 6 Der p 7 Der p 8 Der p 9 Der p 10 Der p 14 Cysteine protease ? Trypsin (serine protease) Amylase ? Chymotrypsin (serine protease) ? Glutathione transferase Collagenase (serine protease) Tropomyosin Apolipophorin like protein Proteinase allergens are common and widespread: Fungi, insects, plants, parasites, drugs (but…most allergens are not proteases) Protease allergens can breach epithelial barriers Wan et al., Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions J Clin Invest, 1999, 104, 123-133 Leads to immune sensitisation without the ‘deliberate’ invasion and infection mechanisms of a pathogen Proteases as activators of cells Inactivators Protease Activated Receptors PAR Activators Inactivators PAR1 Thrombin, Trypsin Granzyme A PAR2 PAR3 PAR4 Trypsin, Tryptase, Factor Xa, Proconvertin Thrombin Thrombin, Trypsin, Cathepsin G Cathepsin G, Elastase, Plasmin Proteinase 3 Cathepsin G,, Plasmin, Proteinase 3 Cathepsin G, Elastatase ? Journal of Immunology 2001 167 1014-1021 PAR are also involved in: • Induction of of epithelial cell & fibroblast proliferation • Induction of cytokines & chemokine expression • Induction of pharmacological mediator release • Induction of metalloproteases • Regulation of smooth muscle tone Do protease allergens induce IL-4 release by Mast cells Resting Mast cell Degranulated mast cell Mediators released include: Leukotriene C4 & D4, Prostaglandin D2 Platelet Activating Factor, Chymase, Tryptase, Heparin, Histamine IL-4, IL-4, IL-5, IL-6, IL-8, TNF-a Journal of Leukocyte Biology 2003, 73 165-171 Constitutive & Induced Cytokine Expression by KU812 Basophils Constitutive 516bp PMA/Ionomycin Induced 516bp -actin IL-3 IL-4 IL-5 IL-6 IL-8 IL-13 IFN-g Der p1 Induces Cytokine Type-2 Cytokine mRNA Expression in KU812 516bp IL-4 516bp IL-5 516bp IL-13 516bp IFN-g 516bp +ve -ve Inhibitors Inhibited Der p1 Der p1 0 -actin Protease Inhibitors Do Not Prevent Cytokine mRNA Expression by KU812 516bp IL-13 516bp -actin - - + - + - + + PMA/Ionomycin Inhibitors Non-Proteolytic Antigens Do Not Induce Cytokine mRNA Expression by KU812 516bp IL-13 516bp -actin Time (hr) 1 1 4 4 + PMA/Ionomycin - + - + - - - - - Tetanus toxoid 4 -ve Der p1 induces IL-4 and IL-13 protein expression in Freshly isolated Basophils Necator Americanus Proteases Induce Type-2 Cytokine Expression by KU812 516bp IFN-g 516bp IL-5 516bp IL-4 516bp IL-13 516bp -actin -ve +ve 200ng/ml ES 1000ng/ml ES + Inhibitors 0 ES 100ng/ml ES 1000ng/ml ES 200ng/ml ES 100ng/ml ES 0 ES - Inhibitors Der p1 and hookworm excretory/secretory products induce IL-4 and IL-13 protein expression in KU812 Basophils The switch to IgE Lebman & Coffman 1988 J Exp Med 168, 853-862 Switch regions Cm Sm Cd Cg3 Sg3 Cg1 Sg1 Ca1 Sa1 Cg2 Sg2 Cg4 Ce Sg4 Se Ca2 Sa2 Cd • Switch regions - repetitive regions of DNA that physically recombine • Upstream of C regions • The Sm consists of 150 repeats of [(GAGCT)n(GGGGGT)] where n is between 3 and 7. • Switching is mechanistically similar to V(D)J recombination. Cm VDJ Cg3 VDJ Cg3 IgG3 produced. Switch from IgM Switch recombination to IgE A three signal process: 1. Antigen – controls entire process 2. Soluble help via IL-4 or IL-13 from T helper cells 3. Cognate help via CD40 L from T helper cells T cell help to B cells IL-4 and IL-13 B Th Th Y Antigen CD40 CD40 Ligand Switch recombination to IgE A three signal process: 1. Antigen 2. Soluble help via IL-4 or IL-13 from T helper cells 3. Cognate help via CD40 L from T helper cells Soluble help via IL-4 or IL-13 from T helper cells IL-4R IL-13R IL-4 IL-13 IL-4 IL-13 gC IL-4Ra JAK1 JAK3 P TYK1 IL-4Ra JAK1 P Stat-6 Stat-6 P P Stat-6 P P TYK2 PDimerised Stat-6 P Stat-6 Stat-6 translocates to nucleus P Stat-6 P Stat-6 P IL-13Ra1/2 Switch recombination to IgE A three signal process: 1. Antigen 2. Soluble help via IL-4 or IL-13 from T helper cells 3. Cognate help via CD40 L from T helper cells Cognate help via CD40 L from T helper cells Ligation promotes aggregation in lipid rafts CD40 2 3 5 6 TNF receptor associated factors IkB Uninhibited NFkB translocates to the IkB nucleus NF kB NF kB Activation of the Ie promoter Activation/cytokine responsive promoter Ie C/EBP Stat6 AP-1 Se PU.1 NFkB Ce1 Ce2 Ce3 Ce4 BSAP Ie Induced by IL-4/IL-13 and CD40 ligation BSAP – B cell specific activator protein. C/EBP CCAAT/enhancer binding protein. PU.1 – Spi1 equivalent in humans, ets transcription factor Germline IgE transcripts Transcription C/EBP Stat6 PU.1 NFkB Ie Se Ce1 Ce2 Ce3 Ce4 DNA Ie Se Ce1 Ce2 Ce3 Ce4 RNA Germline transcripts Ie Ce Spliced RNA Why has this mechanism evolved to transcribe just the C region? VHDHJH is needed to make a functional IgE Why is the epsilon switch region spliced out? What do germline transcripts do? Ie Se Ce1 Ce2 Ce3 Ce4 Ie Stat6 PU.1 Spliced RNA Ce RNA Se C/EBP RNA S region RNA hybridises with template DNA NFkB Ie Se Ce1 Ce2 Ce3 Ce4 Mechanism of class switch recombination Single stranded DNA 1. S region in the genomic DNA ‘melts’ Se Ie R Se loop Ce1 Se 5’ Se 3’ 2. S region RNA spliced from germline RNA transcript hybridises to single-stranded DNA 3. ssDNA R loop formed – a substrate for AID - ACTIVATIONINDUCED CYTIDINE DEAMINASE Activation-induced cytidine deaminase B cell activation by antigen leads to: Soluble help via Th cell IL-4 or IL-13 Cognate help via Th cell CD40 L from T helper Induces Stat 6 Releases NFkB from IkB Stat6 NFkB Activation-induced cytidine deaminase gene AID gene is expressed under the same conditions as B cells induced to switch Ig isotype Activation-induced cytidine deaminase • Expressed only in B cells • Involved in isotype class switching & somatic hypermutation • AID knockout mice do not class switch Ig isotype • Ectopic expression in non B cells causes class switch • Mutation in the AID gene can cause hyper IgM syndrome • Deaminates cytidine on ssDNA, i.e. substitutes U for C Preferred Se region target sequence for AID IgE S region GGGCTGGGCTGAGCTGRGCTGAGCTGRGCTGAGCTRARNT CCCGACCCGACTCGACYCGACTCGACYCGACTCGAYTYNA Non-template strand is G-Rich and contains RGYW (A/G G T/C A/T) motifs Replication protein A (RPA) targets AID to ssDNA in R loops by binding to RGYW motifs AID RPA RPA GGGCTGGGCTGAGCTGRGCTGAGCTGRGCTGAGCTRARNT Activation induced cytidine deaminase Activation induced cytidine deaminase GGGCTGGGCTGAGCTGRGCTGAGCTGRGCTGAGCTRARNT Non-template ssDNA GGGCTGGGCTGAGCTGRGCTGAGCTGRGCTGAGCTRARNT RNA/template CCCGACCCGACTCGACYCGACTCGACYCGACTCGAYTYNA DNA hybrid NH2 HN AID N O O N Cytidine O N Uridine AID may also deaminate C on the template strand ?RNAase? AID mediated deamination of cytidine to Uridine G - U mismatch repair GGGUTGGGUTGAGUTGRGUTGAGUTGRGUTGAGUTRARNT CCCGACCCGACTCGACYCGACTCGACYCGAUTCGAYTYNA S region DNA now contains mismatched G – U pairs that must be repaired e.g. by the base excision repair mechanism Uracil-DNA glycolase (UNG) removes uracil to leave abasic sites in S region UNG UNG UNG UNG UNG UNG UNG GGGUTGGGUTGAGUTGRGUTGAGUTGRGUTGAGUTRARNT CCCGACCCGACTCGACYCGACTCGACYCGAUTCGAYTYNA UNG P P P P P P GGGUTGA CCCGACT Base is removed, but backbone remains intact P P P P P P G - U mismatch repair OH Abasic site is processed by the apurinic/apyrimidimic endonuclease 1 (APE1) APE1P P P P P P P GGGUTGA CCCGACT P P P P P P DNA is now nicked to produce a single strand break GGGCTGGGU TGAGCTGRGCTGAGCTGRGCTGAGCTRARNT APE1 CCCGACCCGACTCGACYCGACTCGACYCGAU TCGAYTYNA GGGUTGGGUTGAGUTGRGUTGAGUTGRGUTGAGUTRARNT CCCGACCCGACTCGACYCGACTCGACYCGAUTCGAYTYNA Similar mechanism on the template strand creates a staggered double strand break APE1 Processing of staggered ends GGGCTGGG TGAGCTGRGCTGAGCTGRGCTGAGCTRARNT CCCGACCCGACTCGACYCGACTCGACYCGA TCGAYTYNA GGGCTGGG Exonuclease activity CCCGACCCGACTCGACYCGACTCGACYCGA End fill-in reactions Cm Sm Cd TGAGCTGRGCTGAGCTGRGCTGAGCTRARNT ACTCGACYCGACTCGACYCGAC TCGAYTYNA Cg3 Sg3 Cg1 Sg1 Ca1 Sa1 Cg2 Sg2 Cg4 Sg4 Ce Se Ca2 Sa2 Process occurs in two S regions simultaneously • • • • • Activation of Im & Ie promoter by Ag, IL-4/13 and CD40L Production of germline transcripts and splicing of Sm and Se Deamination of ssDNA in Sm and Se by AID Base excision and mismatch repair Blunt-ended ds breaks and synapsis of Sm to Se by non-homologous end joining Cm Cd Sm Cg3 Sg3 Cg1 Sg1 Ca1 Sa1 Cg2 Sg2 Sg4 Ce Se Ca2 Sa2 Cg1 Ca1 Cg1 Ca1 Cg3 Cg2 Cd Cg4 Excised episomal circle of intervening DNA Cg3 Cg2 Cd Cg4 Cm Cm VDJ Cg4 Ce Ca2 VDJ Ce Ca2 Non-homologous end joining in class switch Closely resembles another B cell Ig gene mechanism Ig gene recombination 7 23 9 12 7 V 9 After N and P nucleotides have been inserted, several other proteins, (Ku70:Ku80, XRCC4 and DNA dependent protein kinases,ARTEMIS exonuclease, DNA ligase IV) bind to the hairpins and the heptamer ends. Defects in NHEJ proteins impair class switch D J BCL-6 BCL-6 binds to the Stat-6 binding site and represses switching • BCL-6 -/- mice have enhanced IgE isotype switching • BCL-6 -/- Stat6 -/- mice have no IgE • An RFLP has been mapped to the first intron of the BCL-6 gene that is significantly associated with atopy - but not IgE levels Stat6 BCL-6 Transcription blocked C/EBP Stat6 BCL-6 PU.1 NFkB BSAP Stat6 is involved in Th2 cell differentiation, the expression of CD23 (the low affinity IgE receptor) and VCAM expression BCL-6 may exert it’s anti/pro-allergic activities via these genes Additional areas to think about Can’t get over a 2.2 mark without showing evidence of outside reading in answers • Relationship between isotype switch, somatic hypermutation and proliferation of B cells in the germinal centre • What is the relationship between the deliberately mutagenic mechanisms of isotype switch and somatic hypermutation in B cells and the propensity of B cells to form tumours • Where are the holes in the ‘skew to Th2’ model of allergy? • What are allergic responses really for? What are allergic immune responses really for? Ascaris Onchocerca Toxoplasma Enterobious Plasmodium Trichuris Hookworm Schistosome Trypanosoma Leishmania Taenia Wuchereria Text book view Helminth infections induce IgE, mastocytosis and eosinophilia A classic Th2-driven response Eosinophils killing a schistosome egg in vitro However…….. Heavily parasitised individuals exist - despite Th2 responses and eosinophilia. Scarce in vivo evidence of eosinophil and IgE control of helminth infection Yet IL-4 may be involved - Trichuris muris model Susceptible mice Resistant mice Else et al., 1994 J. Exp Med 179 347-351 Th2 cells themselves may not be needed Nippostrongylus infection IL-4 IL-4 from any source is sufficient to induce worm expulsion Urban et al., 1995 J. Immunol. 154, 4675-4684