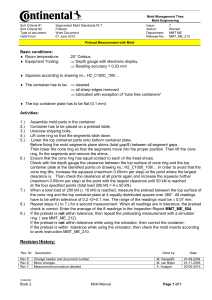
Folie 1 - Pulsion
advertisement

Haemodynamic Monitoring Theory and Practice Haemodynamic Monitoring 2 A. Physiological Background B. Monitoring C. Optimising the Cardiac Output D. Measuring Preload E. Introduction to PiCCO Technology F. Practical Approach G. Fields of Application H. Limitations Measuring Preload Volumetric Preload Parameters, Volume Responsiveness and Filling Pressures Preload Filling Pressures CVP / PCWP 3 Volumetric Preload parameters GEDV / ITBV Volume Responsiveness SVV / PPV Measuring Preload Role of the filling pressures CVP / PCWP Correlation between Central Venous Pressure CVP and Stroke Volume Kumar et al., Crit Care Med 2004;32: 691-699 4 Measuring Preload Role of the filling pressures CVP / PCWP Correlation between Pulmonary Capillary Wedge Pressure PCWP and Stroke Volume Kumar et al., Crit Care Med 2004;32: 691-699 5 Measuring Preload Role of the filling pressures CVP / PCWP The filling pressures CVP and PCWP do not give an adequate assessment of cardiac preload. The PCWP is, in this regard, not superior to CVP (ARDS Network, N Engl J Med 2006;354:2564-75). Pressure is not volume! Influencing Factors: -Ventricular compliance -Position of catheter (PAC) -Mechanical ventilation -Intra-abdominal hypertension 6 Measuring Preload Role of the volumetric preload parameters GEDV / ITBV Preload Filling Pressures CVP / PCWP 7 Volumetric Preload parameters Volume Responsiveness GEDV / ITBV SVV / PPV Measuring Preload Role of the volumetric preload parameters GEDV / ITBV GEDV = Global Enddiastolic Volume Lungs Pulmonary Circulation Right Heart Left heart Body Circulation Total volume of blood in all 4 heart chambers 8 Measuring Preload Role of the volumetric preload parameters GEDV / ITBV GEDV shows good correlation with the stroke volume Michard et al., Chest 2003;124(5):1900-1908 9 Measuring Preload Role of the volumetric preload parameters GEDV / ITBV ITBV = Intrathoracic Blood Volume Lungs Pulmonary Circulation Right heart Left heart Body Circulation ITBV =GEDV + PBV Total volume of blood in all 4 heart chambers plus the pulmonary blood volume 10 Measuring Preload Role of the volumetric preload parameters GEDV / ITBV ITBV is normally 1.25 times the GEDV ITBVTD (ml) 3000 2000 1000 0 ITBV = 1.25 * GEDV – 28.4 [ml] 0 1000 GEDV vs. ITBV in 57 Intensive Care Patients Sakka et al, Intensive Care Med 2000; 26: 180-187 11 2000 3000 GEDV (ml) Measuring Preload Role of the volumetric preload parameters GEDV / ITBV The static volumetric preload parameters GEDV and ITBV • Are superior to filling pressures for assessing cardiac preload (German Sepsis Guidelines) • Are, in contrast to cardiac filling pressures, not falsified by other pressure influences (ventilation, intra-abdominal pressure) 12 Measuring Preload Role of the dynamic volume responsiveness parameters SVV / PPV Preload Filling Pressures CVP / PCWP 13 Volumetric Preload parameters GEDV / ITBV Volume Responsiveness SVV / PPV Measuring Preload Physiology of the dynamic parameters of volume responsiveness Fluctuations in blood pressure during the respiration cycle Early Inspiration Intrathoracic pressure „Squeezing “ of the pulmonary blood Left ventricular preload Left ventricular stoke volume Late Inspiration Intrathoracic pressure Venous return to left and right ventricle Left ventricular preload Left ventricular stroke volume Systolic arterial blood pressure Inspiration PPmax 14 Reuter Expiration PPmin et al., Anästhesist 2003;52: 1005-1013 Systolic arterial blood pressure Inspiration PPmax Expiration PPmin Measuring Preload Physiology of the dynamic parameters of volume responsiveness Fluctuations in stroke volume throughout the respiratory cycle SV SV SV V V Preload Mechanical Ventilation Intrathoracic pressure fluctuations Changes in intrathoracic blood volume Preload changes Fluctuations in stroke volume 15 Measuring Preload Role of the dynamic volume responsiveness parameters SVV / PPV SVV = Stroke Volume Variation SVmax SVmin SVmean • The variation in stroke volume over the respiratory cycle • Correlates directly with the response of the cardiac ejection to preload increase (volume responsiveness) 16 mean Measuring Preload Role of the dynamic volume responsiveness parameters SVV / PPV SVV is more accurate for predicting volume responsiveness than CVP Sensitivity 1 0,8 0,6 0,4 - - - CVP ___ SVV 0,2 0 0 Berkenstadt et al, Anesth Analg 92: 984-989, 2001 17 0,5 Specificity 1 Measuring Preload Role of the dynamic volume responsiveness parameters SVV / PPV PPV = Pulse Pressure Variation PPmean PPmax PPmin • The variation in pulse pressure amplitude over the respiration cycle • Correlates equally well as SVV for volume responsiveness 18 Measuring Preload Role of the dynamic volume responsiveness parameters SVV / PPV A PPV threshold of 13% differentiates between responders and non-responders to volume administration respiratory changes in arterial pulse pressure (%) Non – Responders n = 24 Responders n = 16 Michard et al, Am J Respir Crit Care Med 162, 2000 19 Measuring Preload Role of the dynamic volume responsiveness parameters SVV / PPV The dynamic volume responsiveness parameters SVV and PPV - are good predictors of a potential increase in CO due to volume administration - are only valid with patients who are fully ventilated and who have no cardiac arrhythmias 20 Extra Role of extravascular lung water EVLW EVLW = Extravascular Lung Water Lungs Pulmonary circulation Left Heart Right Heart Body circulation Extravascular water content of the lung 21 Extra Role of extravascular lung water EVLW The Extravascular Lung Water EVLW - is useful for differentiating and quantifying lung oedema - is, for this purpose, the only parameter available at the bedside - functions as a warning parameter for fluid overload 22 Measuring Preload Summary and Key Points • The volumetric parameters GEDV / ITBV are superior to the filling pressures CVP / PCWP for measuring cardiac preload. • The dynamic parameters of volume responsiveness (SVV and PPV) can predict whether CO will respond to volume administration. • GEDV and ITBV show what the actual volume status is, whilst SVV and PPV reflect the volume responsiveness of the heart. • For optimal control of volume therapy simultaneous monitoring of both the static preload parameters and the dynamic parameters of volume responsiveness is sensible (F. Michard, Intensive Care Med 2003;29: 1396). 23