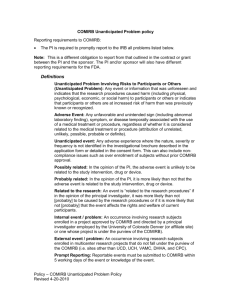
Using the short form and reporting adverse events
advertisement

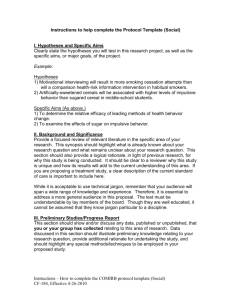
Using the short form and reporting adverse events Erin Coons, Senior IRB Specialist, COMIRB 1 The short form 2 …the consent form may be either of the following: 1. A written consent document that embodies the elements of informed consent required by [regulation]. This form may be read to the subject or the subject's legally authorized representative, but in any event, the investigator shall give either the subject or the representative adequate opportunity to read it before it is signed; or 2. A short form written consent document stating that the elements of informed consent required by [regulation] have been presented orally to the subject or the subject's legally authorized representative. When this method is used, there shall be a witness to the oral presentation. Also, the IRB shall approve a written summary of what is to be said to the subject or the representative. Only the short form itself is to be signed by the subject or the representative. However, the witness shall sign both the short form and a copy of the summary, and the person actually obtaining consent shall sign a copy of the summary. A copy of the summary shall be given to the subject or the representative, in addition to a copy of the short form. 21 CFR 50.27(b) and 45 CFR 46.117(b) 3 COMIRB Policy Non-English speaking subjects may not be enrolled with a short form process of consent documentation unless reviewed and approved in advance by the COMIRB. For studies reviewed by COMIRB, if a non-English-speaking subject is enrolled unexpectedly, researchers may rely on an oral translation of the English language consent form or the COMIRB template short consent form, but should take extra care in the informed consent process to ensure that the subject has understood the project. A statement in the research records (and on the English language consent form) should indicate that the translation took place, identify the translator, and document the translator‘s belief that the subject understands the study and the consent process. If the subject is a patient, a note about the translation should be made in the patient‘s medical records as well. Researchers should try to provide a written translation of the vital emergency contact information. 4 COMIRB Policy… A study is permitted to utilize the short form up to three times in the same language. If a 4th subject is to be enrolled then a translation of the entire consent form should be provided to COMIRB for approval. For studies with a separate HIPAA B form, the HIPAA B form in English (unless the Spanish translation is being used) must also be translated by the interpreter as part of the summary and the HIPAA B form must be signed and dated by the subject or representative. 5 Short forms available on COMIRB web site • Amharic • Arabic • Burmese • Chinese • French • Hindi • Korean • Laotian • Mandarin • Nepali (Coming soon) • Polish • Portuguese • Punjabi • Russian • Serbian • Spanish Adult • Swahili • Tagalog • Thai • Urdo • Vietnamese 6 • English example: http://gcrc.ucdenver.edu/comirb/Short-Form-AdultEnglish.doc 7 Reporting adverse events to COMIRB 8 • Unanticipated Problem Involving Risks to Participants or Others (Unanticipated Problem): Any event or information that was unforeseen and indicates that the research procedures caused harm (including physical, psychological, economic, or social harm) to participants or others or indicates that participants or others are at increased risk of harm than was previously known or recognized. • Unanticipated event: Any adverse experience where the nature, severity or frequency is not identified in the investigational brochure described in the application form or detailed in the consent form. This can also include noncompliance issues such as over enrollment of subjects without prior COMIRB approval. • Adverse Event: Any unfavorable and unintended sign (including abnormal laboratory finding), symptom, or disease temporally associated with the use of a medical treatment or procedure, regardless of whether it is considered related to the medical treatment or procedure (attribution of unrelated, unlikely, possible, probable or definite). 9 • Possibly related: In the opinion of the PI, the adverse event is unlikely to be related to the study intervention, drug or device. • Probably related: In the opinion of the PI, it is more likely than not that the adverse event is related to the study intervention, drug or device. • Definitely related: In the opinion of the PI, it is very likely that the adverse event is related to the study intervention, drug or device. • Related to the research: An event is related to the research procedures if in the opinion of the principal investigator, it was more likely than not [probably] to be caused by the research procedures or if it is more likely that not [probably] that the event affects the rights and welfare of current participants. 10 Adverse events that are • unexpected AND • probably or definitely related to the study procedures, drug, or device must be reported to COMIRB within 5 days 11 Adverse events that are • expected OR • not related or possibly related to the study procedures, drug, or device must be reported in summary form at the next continuing review 12 External events http://gcrc.ucdenver.edu/comirb/Decision-Tree-SafetyReport-Received-from-Sponsor.xls 13 COMIRB policy: Other events that require immediate reporting • • • An actual unforeseen harmful or unfavorable occurrence to participants or others that relates to the research protocol (injuries, psychological events, drug errors). An unforeseen development that potentially increases the likelihood of harm to participants or others in the future. Information that indicates a change to the risks or potential benefits of the research. For example: An interim analysis or safety monitoring report indicates that frequency or magnitude of harms or benefits may be different than initially presented to the COMIRB. A paper is published from another study that shows that the risks or potential benefits of your research may be different than initially presented to the COMIRB. • A problem involving data collection, data storage, privacy or confidentiality. • Incarceration of a participant in a protocol not approved to enroll prisoners. • Pregnancy of a participant or spouse in a protocol that specifically exclude pregnancy due to the potential risks of the intervention or treatment on the fetus. 14 COMIRB policy: Other events that require immediate reporting • Change to the protocol taken without prior COMIRB review to eliminate an apparent immediate hazard to a research participant. • Complaint of a participant when the complaint indicates unexpected risks or cannot be resolved by the research team. • Protocol violation (meaning an accidental or unintentional change to the COMIRB approved protocol) that harmed participants or others or that indicates participants or others may be at increased risk of harm. • Study related event that requires prompt reporting to the sponsor. • Sponsor imposed suspension for risk. • Non compliance by the PI or research team • Any other problem that caused a risk to the participant or others 15 The unanticipated problem form should also be used to submit the following documents to COMIRB for prompt review if they meet the criteria for an unanticipated problem: • Medwatch reports • IND reports • DSMB or other safety review reports • Investigational Brochures changes • Changes to Package Inserts • Audit reports • Complaints 16 What does not require immediate reporting to COMIRB? • Out of window visits that do not affect subject safety • Death due to disease progression • IND Safety Reports that do not meet the definition of an unanticipated problem • Drug side effects listed in the risk section of the consent form 17 Reporting adverse events to the sponsor and FDA – drug studies 18 • Sponsor (not the investigator) determines causality • For this reason, investigators must immediately report any serious adverse event to the sponsor, without regard to causality (21 CFR 312.64(b)) • However, it is also important for the sponsor to consider the investigator’s view when assessing the safety of the drug • Nonserious adverse events reported to sponsor per protocol • Follow the protocol! 19 An adverse event or suspected adverse reaction is considered “serious” if, in the view of either the investigator or sponsor, it results in any of the following outcomes: Death, a life-threatening adverse event, inpatient hospitalization or prolongation of existing hospitalization, a persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions, or a congenital anomaly/birth defect. Important medical events that may not result in death, be life-threatening, or require hospitalization may be considered serious when, based upon appropriate medical judgment, they may jeopardize the patient or subject and may require medical or surgical intervention to prevent one of the outcomes listed in this definition. 20 Examples • allergic bronchospasm requiring intensive treatment in an emergency room or at home • blood dyscrasias or convulsions that do not result in inpatient hospitalization • the development of drug dependency or drug abuse 21 The sponsor [including an investigator who holds an IND] must report to FDA and all participating investigators any suspected adverse reaction that is both serious and unexpected. Before submitting this report, the sponsor needs to ensure that the event meets all three of the definitions contained in the requirement: • Suspected adverse reaction • Serious • Unexpected If the adverse event meets all three of the definitions, it should be submitted as an expedited IND safety report (Medwatch report for drug studies without an IND, or VAERS report for vaccine studies without an IND) within 15 days. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegul atoryInformation/Guidances/UCM227351.pdf 22 Suspected adverse reaction means any adverse event for which there is a reasonable possibility that the drug caused the adverse event. For the purposes of IND safety reporting, ‘reasonable possibility’ means there is evidence to suggest a causal relationship between the drug and the adverse event. 23 Examples of types of evidence that would suggest a causal relationship between the drug and the adverse event • A single occurrence of an event that is uncommon and known to be strongly associated with drug exposure (e.g., angioedema, hepatic injury, Stevens-Johnson Syndrome) • One or more occurrences of an event that is not commonly associated with drug exposure, but is otherwise uncommon in the population exposed to the drug (e.g., tendon rupture) • An aggregate analysis of specific events observed in a clinical trial (such as known consequences of the underlying disease or condition under investigation or other events that commonly occur in the study population independent of drug therapy, e.g., MI in an elderly population) that indicates those events occur more frequently in the drug treatment group than in a concurrent or historical control group 24 An adverse event or suspected adverse reaction is considered “unexpected” if it is not listed in the investigator brochure or is not listed at the specificity or severity that has been observed; or, if an investigator brochure is not required or available, is not consistent with the risk information described in the general investigational plan or elsewhere in the current application. 25 Examples: • hepatic necrosis would be unexpected (by virtue of greater severity) if the investigator brochure referred only to elevated hepatic enzymes or hepatitis • cerebral thromboembolism and cerebral vasculitis would be unexpected (by virtue of greater specificity) if the investigator brochure listed only cerebral vascular accidents • adverse events or suspected adverse reactions that are mentioned in the investigator brochure as occurring with a class of drugs or as anticipated from the pharmacological properties of the drug, but are not specifically mentioned as occurring with the particular drug under investigation (e.g., angioedema with ACE inhibitors) 26 Reporting adverse events to the sponsor and FDA – Device studies 27 An investigator shall submit to the sponsor a report of any unanticipated adverse device effect occurring during an investigation as soon as possible, but in no event later than 10 working days after the investigator first learns of the effect. 28 Sponsors (including investigators who hold an IDE or lead a trial of a Non-significant Risk or exempt device) must immediately evaluate the reported unanticipated adverse device effect and report to FDA, responsible IRBs, and participating investigators within 10 working days. 29 Unanticipated adverse device effect means any serious adverse effect on health or safety or any lifethreatening problem or death caused by, or associated with, a device, if that effect, problem, or death was not previously identified in nature, severity, or degree of incidence in the investigational plan or application (including a supplementary plan or application), or any other unanticipated serious problem associated with a device that relates to the rights, safety, or welfare of subjects. 30 Summary of adverse event reporting • Unexpected and probably / definitely related, regardless of severity - to COMIRB within 5 days • Local events: Expected or unrelated events – to COMIRB in summary form at continuing review • External events: See decision tree • IND studies: Serious adverse events, regardless of causality or expectedness – to the sponsor immediately • All drug studies: Serious adverse events, reasonable probability related to drug, and unexpected – to the FDA and participating investigators by the sponsor within 15 days • IND studies: Nonserious adverse events per protocol • Device studies: Serious adverse events, related to or associated with device, and unexpected – to the sponsor within 10 days, and to the FDA and participating investigators by the sponsor within 10 days 31 References • COMIRB Policies and Procedures http://www.ucdenver.edu/academics/research/AboutUs/c omirb/forms/comirb%20forms/01COMIRB%20Policy%20and%20Procedures%20Docume nt.pdf • FDA Guidance – Adverse Event Reporting to IRBs (From 2009 - Drug information is outdated, use for devices only) http://www.fda.gov/downloads/drugs/guidancecomplianc eregulatoryinformation/guidances/ucm079753.pdf • FDA Guidance - Safety Reporting Requirements for INDs and BA/BE Studies http://www.fda.gov/downloads/Drugs/GuidanceComplian ceRegulatoryInformation/Guidances/UCM227351.pdf 32 Erin Coons Senior IRB Specialist, COMIRB erin.coons@ucdenver.edu 303-724-1551 http://www.ucdenver.edu/academics/research/AboutU s/comirb/Pages/comirb-home.aspx 33