Types of assistive gait devices
advertisement

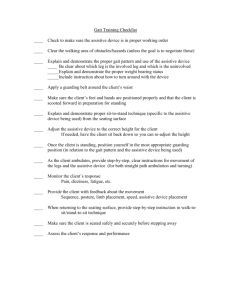
Using assistive gait devices in rehabilitation Reasons for using an assistive gait device are: Poor balance, Inability to bear weight on a lower extremity due to fracture or other injury, Paralysis involving one or both lower extremities, or Amputation of a lower extremity. Advantages to early ambulation following an injury: • Aiding circulation, • Preventing calcium loss in bones, and • Aiding the pulmonary and renal systems. General Principles The patient to be carefully evaluated in order to select the appropriate assistive device to meet the patient’s needs. The therapist must be aware of the patient’s total medical condition, weight-bearing status of the involved extremity when considering which type of assistive device to use with the patient. The therapist will need to determine the range of motion of the extremities and the strength of the primary muscles required for ambulation. The patient must press downward on the assistive gait device in order to move the body forward. The scapular, shoulder, and elbow musculature supports the body’s weight while the nonaffected lower extremity is moved forward. The finger flexors fold the hand-piece of the assistive gait device. The primary muscles required for ambulation with axillary crutches, using a three-point (non-weight bearing on one lower extremity) crutch gait pattern, are the scapula stabilizers, shoulder depressors, shoulder extensors, elbow extensors, and finger flexors for the upper extremity. The primary lower-extremity muscles in the weightbearing lower extremity are the hip extensors, hip abductors, knee extensors, knee flexors, and ankle dorsi-flexors. While the patient is standing on the unaffected lower extremity, the muscles of the hip and knee provide stability. The ankle dorsi-flexors position the foot so that it can clear the floor when the limb is swinging forward • Types of assistive gait devices • When choosing an assistive gait device, the therapist considers the amount of support the patient will need and the patient’s ability to manipulate the device. • The selection of an assistive gait device is based on the patient’s disability, coordination, and stability. • For example, you may have two patients with the same type of fracture. One of the patients may use crutches if he or she has adequate stability and coordination to safely use them. The other patient may require a walker due to poor stability and coordination. • As the patient’s abilities improve, they may advance to an assistive device providing less stability and support for easier maneuverability. • Types of assistive gait devices: • Assistive gait devices are designed to improve the patient’s stability by increasing the base of support. • The categories of assistive ambulation devices, in order from greatest to least amount of support, are: • • • • • • • Parallel bars, Walkers, Axillary crutches, Forearm (Loftstrand) crutches, Two canes, and One cane. All categories of assistive gait devices are adjustable and come in tall, adult, and child sizes. Additionally, a special platform can be attached to walkers or axillary crutches for patients who are unable to bear weight through the hand, wrist, or forearm. 1) Parallel bars Parallel bars are used when maximal patient support and stability are required. The gait pattern can be practiced in parallel bars and the fit of the assistive device can be checked. The parallel bars limit mobility. So once the patient becomes proficient with the appropriate gait pattern, the patient must be progressed to another assistive gait device to be mobile. Care must be taken so that the patient does not become dependent on the parallel bars. • The parallel bar height needs to be adjusted to provide 15 to 20 degrees of elbow flexion when the patient is standing erect and is grasping the bars about 6 inches anterior to the hips. The bars need to be approximately 2 inches wider than the patient’s hips when the patient is centered between the bars. 2) Walkers • Walkers provide maximum stability and support and allow the patient to be mobile. • Walkers are designed in many styles, but all have four legs. • Some may have two or four wheels. • Wheels allow the patient to gently push the device forward as opposed to picking the walker up to move it forward. • Another variation in the design of the walker is the ability to fold the walker when it is not being used. This feature allows for easier transportation in a car and for storage. Disadvantages of using walkers: • Walkers are cumbersome and difficult to store and transport. Walkers are very difficult to use on stairs. Walkers reduce the speed of ambulation. The patient is unable to use a normal gait pattern by using walker. To properly fit a patient with a walker, adjust the height of the walker so that the patient has between 15 and 25 degrees of elbow flexion when grasping the handles of the walker. 3) Axillary crutches • Axillary crutches are used with patients who do not require as much stability or support as provided by a walker. • Axillary crutches allow the patient to perform a greater variety of gait patterns and ambulate at a faster pace. Disadvantages of axillary crutches: Axillary crutches are less stable than walker. Improper use of axillary crutches can cause injury to the neurovascular structures in the axillary region. Axillary crutches require good standing balance by the patient. Geriatric patient may fell insecure or may not have the necessary upper- body strength to use axillary crutches. • To properly fit a patient with axillary crutches, both the length of the crutches and the height of the hand piece must be properly adjusted. • The length of the axillary crutch should be adjusted so the therapist can fit two or three fingers between the top of the axillary crutch and the patient’s axilla. • When standing, the tips of the crutches should be approximately 6 inches from the toes of the patient’s shoes at a 45-degree angle. • The handpiece of the axillary crutch should be adjusted so the patient has 15 to 25 degrees of elbow flexion. 4) Forearm crutches Forearm crutches (Loftstrand or Canadian crutches) are used when the patient need crutches permanently, or for long periods of time. People who use Loftstand crutches must have the stability and coordination to use them. Using forearm crutches requires no more energy, increased oxygen consumption or heart rate than axillary crutches. This type of crutch has the advantage of being easily stored and transferred. There is no risk of injury to the neurovascular structures in the axillary region when using this type of crutches. Disadvantages of forearm crutches: Forearm crutches are less stable than a walker. They require good standing balance and upper-body strength. Geriatric patient sometimes feel insecure with these crutches. They may not have the necessary upper-body strength to use forearm crutches. To fit the patient with forearm crutches: have the patient stand with arms hanging loosely by the side. Place the crutch parallel to the lateral aspect of the tibia and femur. Adjust the height of the hand-piece so that it is level with the ulnar styloid process. This will insure the elbow is flexed between 15 and 25 degrees. The top of the forearm cuff should be adjusted so that it is located 1 to 1.5 inches distal to the olecranon process of the elbow while the patient is grasping the hand-piece of the crutch with the wrist in neutral flexion-extension. 5) Canes Canes are used to compensate for impaired balance or to increase stability while ambulating. There are several styles of canes but the standard is known as the J cane. A cane is functional on stairs and in confined areas. It is also easily stored and transported. Disadvantage of a cane • It provides limited support due to its small base of support. To fit a patient with a cane: have the patient stand and place the can parallel to the lateral aspect of the tibia and femur. Adjust the hand piece of the cane so it is level with the ulnar styloid process. This will provide 15 to 25 degrees of elbow flexion when the patient grasps the handle of the cane. Basic gait patterns • The selection of the proper gait pattern is dependent upon the patient’s • • • • • balance, strength, coordination, functional needs, and weight-bearing status. 1. Four-point gait pattern A four-point gait pattern is used when the patient requires maximum assistance with balance. It requires the use of bilateral assistive gait devices (canes or crutches). The pattern begins with the forward movement of one of the assistive gait devices, and then the contralateral lower extremity, the other assistive gait device, and finally the opposite lower extremity (e.g., right cane, then left foot; left cane, then right foot). This is a slow gait pattern, but a stable one. 2. Two-point gait pattern The two-point gait pattern requires the use of bilateral assistive gait devices. This pattern is faster than the four-point gait. The two-point gait pattern closely approximates a normal gait pattern and should be encouraged. This pattern does require the patient to coordinate moving an assistive gait device and the contralateral lower extremity at the same time. This pattern is less stable than the four-point pattern. 3. Modified four-point and two-point Gait patterns The modified four-point and two-point gait patterns require only one assistive gait device. The assistive device is used with the opposite upper extremity to the involved lower extremity, if possible. This widens the base of support, increase stride lengths, cadence, and walking velocities than when using the cane on the same side as the involved lower extremity. 4. Three-point gait pattern The three-point pattern requires two crutches or a walker, but it cannot be performed with two canes. This pattern is used when the patient is only able to bear full weight on one lower extremity. When using axillary crutches and a three-point gait pattern, between 44.4 and 49 percent of the patient’s body weight is transmitted through the upper extremities. So the strength of the upper extremities and uninvolved lower extremity must be assessed prior to attempting ambulation. The energy cost (oxygen consumption) for this type of gait is about twice as high as normal walking. The walker or crutches are moved forward first. Next, the involved lower extremity is advanced. Then the patient presses down on the assistive gait device and advances the uninvolved lower extremity. If the uninvolved lower extremity is advanced to where it is parallel to the involved lower extremity, then this would be a “swing to” pattern. If the uninvolved lower extremity is advanced ahead of the uninvolved lower extremity, then this would be a “swing through” pattern. 5. Modified three-point gait pattern The modified three-point gait pattern requires two crutches or a walker. This pattern is used when the patient can bear full weight with one lower extremity but is only allowed to touch the involved lower extremity to the floor. This is known as touchdown weight bearing (TDWB). The term “partial weight bearing” (PWB) refers to when the involved lower extremity is allowed only part of the patient’s weight to be transferred through it. In this pattern, the walker or crutches are advanced first, and then the involved lower extremity is advanced forward. The patient presses down on the assistive gait device and advances the uninvolved lower extremity using either a “swing to” or “swing through” pattern.