Gait Training Using Partial Body Weight Support During Over
advertisement
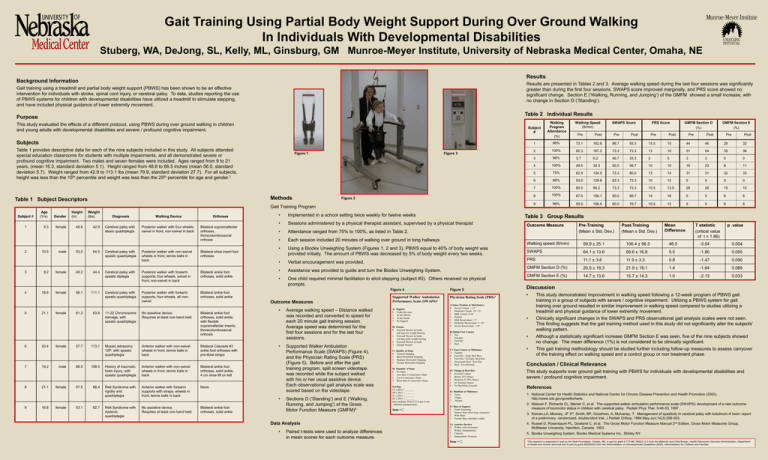
Gait Training Using Partial Body Weight Support During Over Ground Walking In Individuals With Developmental Disabilities Stuberg, WA, DeJong, SL, Kelly, ML, Ginsburg, GM Munroe-Meyer Institute, University of Nebraska Medical Center, Omaha, NE Results Background Information Results are presented in Tables 2 and 3. Average walking speed during the last four sessions was significantly greater than during the first four sessions. SWAPS score improved marginally, and PRS score showed no significant change. Section E (‘Walking, Running, and Jumping’) of the GMFM showed a small increase, with no change in Section D (‘Standing’). Gait training using a treadmill and partial body weight support (PBWS) has been shown to be an effective intervention for individuals with stroke, spinal cord injury, or cerebral palsy. To date, studies reporting the use of PBWS systems for children with developmental disabilities have utilized a treadmill to stimulate stepping, and have included physical guidance of lower extremity movement. Table 2 Individual Results Purpose This study evaluated the effects of a different protocol, using PBWS during over ground walking in children and young adults with developmental disabilities and severe / profound cognitive impairment. Subject # Walking Program Attendance (%) 1 Subjects Table 1 provides descriptive data for each of the nine subjects included in this study. All subjects attended special education classrooms for students with multiple impairments, and all demonstrated severe or profound cognitive impairment. Two males and seven females were included. Ages ranged from 9 to 21 years, (mean 16.3, standard deviation 5.1). Height ranged from 48.8 to 66.5 inches (mean 56.0, standard deviation 5.7). Weight ranged from 42.9 to 113.1 lbs (mean 79.9, standard deviation 27.7). For all subjects, height was less than the 15th percentile and weight was less than the 25th percentile for age and gender.1 Figure 1 Methods Table 1 Subject Descriptors Figure 3 Figure 2 Gait Training Program Subject # 1 2 3 4 5 6 7 8 9 Age (Yrs) Gender Height (in) Weight (lbs) 9.3 female 48.8 42.9 10.6 9.2 18.6 21.1 20.4 19.2 21.1 16.8 male female female female female male female female 53.5 49.2 56.1 61.3 57.7 66.5 57.5 53.1 64.5 44.4 111.1 83.8 113.1 108.5 88.4 62.7 Diagnosis Walking Device Cerebral palsy with ataxic quadriplegia Posterior walker with four wheels, swivel in front, non-swivel in back Cerebral palsy with spastic quadriplegia Orthoses Bilateral supramalleolar orthoses, thoracolumbosacral orthosis Posterior walker with non-swivel wheels in front, tennis balls in back Bilateral shoe insert foot orthoses Cerebral palsy with spastic diplegia Posterior walker with forearm supports, four wheels, swivel in front, non-swivel in back Bilateral ankle foot orthoses, solid ankle Cerebral palsy with spastic quadriplegia Posterior walker with forearm supports, four wheels, all nonswivel Bilateral ankle foot orthoses, solid ankle 11-22 Chromosome damage, with spastic quadriplegia No assistive device. Requires at least one hand held. • Implemented in a school setting twice weekly for twelve weeks • Sessions administered by a physical therapist assistant, supervised by a physical therapist • Attendance ranged from 75% to 100%, as listed in Table 2. • Each session included 20 minutes of walking over ground in long hallways • Using a Biodex Unweighing System (Figures 1, 2 and 3), PBWS equal to 40% of body weight was provided initially. The amount of PBWS was decreased by 5% of body weight every two weeks. • Verbal encouragement was provided. • Assistance was provided to guide and turn the Biodex Unweighing System. • One child required minimal facilitation to elicit stepping (subject #3). Others received no physical prompts. Figure 4 Outcome Measures Bilateral ankle foot orthoses, solid ankle, with flexible supramalleolar inserts, thoracolumbosacral orthosis Mosaic tetrasomy 12P, with spastic quadriplegia Anterior walker with non-swivel wheels in front, tennis balls in back Bilateral Cascade #3 ankle foot orthoses with pre-tibial straps History of traumatic brain injury, with spastic quadriplegia Anterior walker with non-swivel wheels in front, tennis balls in back Bilateral ankle foot orthoses, solid ankle, 4 cm shoe lift on left Rett Syndrome with rigidity and quadriplegia Anterior walker with forearm supports with straps, wheels in front, tennis balls in back None Rett Syndrome with dystonic quadriplegia No assistive device. Requires at least one hand held. Bilateral ankle foot orthoses, solid ankle • • • Average walking speed – Distance walked was recorded and converted to speed for each 20 minute gait training session. Average speed was determined for the first four sessions and for the last four sessions. Supported Walker Ambulation Performance Scale (SWAPS) (Figure 4), and the Physician Rating Scale (PRS) (Figure 5). Before and after the gait training program, split screen videotape was recorded while the subject walked with his or her usual assistive device. Each observational gait analysis scale was scored based on the videotape. Sections D (‘Standing’) and E (‘Walking, Running, and Jumping’) of the Gross Motor Function Measure (GMFM)4 Data Analysis • Paired t-tests were used to analyze differences in mean scores for each outcome measure. Supported Walker Ambulation Performance Scale (SWAPS)2 A) 0 1 2 3 Support Under the arms At the Elbows At the Hands No Support B) Posture 0 Forward Flexion in trunk, and legs low weight-bearing 1 Forward Flexion in trunk, and legs good weight-bearing 2 Forward Flexion in trunk 3 Upright Posture C) 0 1 2 3 Quality of Steps Vertical Stepping Short Horizontal Stepping Medium Horizontal Stepping Normal Horizontal Stepping D) 0 1 2 3 Quantity of Steps No Steps Less than 3 Consecutive Steps 3 to 6 Consecutive Steps More than 6 Consecutive Steps Scoring: (A x 40)/3 =________ (B x 20)/3 =________ (C x 20)/3 =________ (D x 20)/3 =________ (also multiply D by 0.75 if gait is not initiated spontaneously) Sum = Walking Speed (ft/min) SWAPS Score PRS Score Post Pre GMFM Section D (%) Post Pre GMFM Section E (%) Pre Post Pre Post Pre Post 96% 73.1 162.6 86.7 93.3 15.5 15 44 46 28 32 2 100% 92.3 167.2 73.3 73.3 13 10 51 54 35 36 3 96% 3.7 6.2 46.7 33.3 3 5 3 3 0 0 4 100% 49.5 34.3 50.0 56.7 10 10 15 23 8 11 5 75% 62.9 104.5 73.3 80.0 13 14 31 31 32 33 6 86% 53.9 129.8 63.3 73.3 10 12 5 5 0 0 7 100% 80.5 90.2 73.3 73.3 10.5 13.5 26 26 15 15 8 100% 67.5 156.1 50.0 66.7 14 16 5 5 6 6 9 96% 55.5 106.5 60.0 76.7 10.5 12 5 5 8 8 Table 3 Group Results Figure 5 Physician Rating Scale (PRS)3 A) Knee Position at Mid-Stance: 0 Severe Crouch > 15o 1 Moderate Crouch 10o -15o 2 Mild Crouch 0-10o 3 Neutral 2 Mild Recurvatum < 5o 1 Moderate Recurvatum 5o -10o 0 Severe Recurvatum >10o B) Initial Foot Contact 0 Toe 1 Forefoot 2 Foot-flat 3 Heel C) -1 0 1 2 3 Foot Contact at Midstance Equinus Foot-Flat / Early Heel Rise Foot-Flat / No Early Heel Rise Occasional Heel / Foot-Flat Heel / Toe (Normal) D) 0 1 2 3 0 Timing of Heel Rise No Heel Contact Before 25% Stance Between 25-50% Stance At Terminal Stance No Heel Rise (Crouch) E) 0 1 2 Hindfoot at Midstance Varus Valgus Neutral F) 0 1 2 3 Base of Support Frank Scissoring Narrow Base (Poor knee clearance) Wide Base Normal Base (shoulder width) G) 0 1 2 3 Assistive Devices Walker with Assistance Walker (Independent) Crutches Independent 10 meters Sum = Outcome Measure Pre-Training (Mean ± Std. Dev.) Post-Training (Mean ± Std. Dev.) Mean Difference T statistic (critical value of t = 1.86) p value Walking speed (ft/min) 59.9 ± 25.1 106.4 ± 56.3 46.5 -3.54 0.004 SWAPS 64.1 ± 13.6 69.6 ± 16.8 5.5 -1.80 0.055 PRS 11.1 ± 3.6 11.9 ± 3.3 0.8 -1.47 0.090 GMFM Section D (%) 20.5 ± 18.3 21.9 ± 19.1 1.4 -1.64 0.069 GMFM Section E (%) 14.7 ± 13.6 15.7 ± 14.3 1.0 -2.13 0.033 Discussion • • • • This study demonstrated improvement in walking speed following a 12-week program of PBWS gait training in a group of subjects with severe / cognitive impairment. Utilizing a PBWS system for gait training over ground resulted in similar improvement in walking speed compared to studies utilizing a treadmill and physical guidance of lower extremity movement. Clinically significant changes in the SWAPS and PRS observational gait analysis scales were not seen. This finding suggests that the gait training method used in this study did not significantly alter the subjects’ walking pattern. Although a statistically significant increase GMFM Section E was seen, five of the nine subjects showed no change. The mean difference (1%) is not considered to be clinically significant. This gait training methodology should be studied further including follow-up measures to assess carryover of the training effect on walking speed and a control group or non treatment phase. Conclusion / Clinical Relevance This study supports over ground gait training with PBWS for individuals with developmental disabilities and severe / profound cognitive impairment. References 1. National Center for Health Statistics and National Center for Chronic Disease Prevention and Health Promotion (2000), http://www.cdc.gov/growthcharts. 2. Malouin F, Richards CL, Menier C, et al. The supported walker ambulation performance scale (SWAPS); development of a new outcome measure of locomotor status in children with cerebral palsy. Pediatr Phys Ther. 9:48-53, 1997. 3. Koman,LA, Mooney, JF 3rd, Smith, BP, Goodman, A, Mulvaney, T. Management of spasticity in cerebral palsy with botulinum-A toxin: report of a preliminary, randomized, double-blind trial. J Pediatr Orthop. 1994 May-Jun;14(3):299-303. 4. Russel D, Rosenbaum PL, Gowland C, et al. The Gross Motor Function Measure Manual 2nd Edition, Gross Motor Measures Group, McMaster University, Hamilton, Canada, 1993. 5. Biodex Unweighing System, Biodex Medical Systems Inc., Shirley NY. This research is supported in part by the Watt Foundation, Omaha, NE, in part by grant 5 T73 MC 00023-13 0 from the Maternal and Child Bureau, Health Resources Services Administration, Department of Health and Human Services and in part by grant 90DD0533 from the Administration on Developmental Disabilities (ADD), Administration for Children and Families.