Forensic Pathology
advertisement

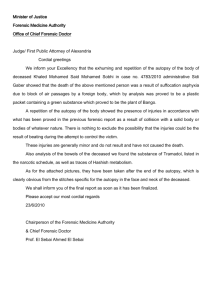
Forensic Pathology (aka Medicolegal Pathology) What is Pathology? Pathology: The scientific study of the nature of disease, its causes and consequences. – Subdisciplines are Clinical, Anatomical and Forensic Pathology. Forensic Pathology A branch of medicine that applies the principles and knowledge of the medical sciences to problems in the field of forensics (medicolegal). Investigates and determines cause and manner of death. Forensics: The scientific application of methods, techniques and procedures to the resolution of problems pertaining to the law. History of Death Investigations Death investigation techniques used in the U.S. today originated in England. A Death Investigator was given the title of Coroner (crown) – Elected to protect the crown’s interests from corrupt sheriff’s. A Coroner could arrest suspects including the sheriff. – This is still the case in Missouri. The Inquest The coroner was required to assemble a group of peers to judge a suspect’s guilt or innocence. The group also considered the necessity of a postmortem (after death) examination or autopsy. – Antemortem (prior to death) History of the Medical Examiner New York city established the 1st city wide death investigations division. In 1939, Maryland developed the 1st statewide death investigations division. Today death investigations are performed differently from state to state and county to county. Coroner/ME Jurisdiction Sudden or Unexpected Death Violent Deaths, e.g. homicide, suicides Unattended Deaths – The person had not seen a physician for more than 20 days prior to death Contagious Diseases, e.g., AIDS Occupational Diseases, e.g. COPD Coroner/ME System California has Coroner/ME System separated by county. – We have more Coroner than ME systems. Some States have either a CO or ME system or it is split by Region. Coroner/ME System Across the U.S., there are MORE Coroner Systems; these are generally represented under the setting of the Sheriff’s Office. – Some Coroner’s offices are also the local Funeral Homes. U.S. (Federal) Government has their own system. Coroner Usually an elected official May be appointed by the Sheriff’s department May be a physician – May be a medical examiner It all depends on the county/state Medical Examiner (also known as a Forensic Pathologist) Must be a Pathologist who is a M.D. or D.O. A doctor must have advanced training to become a ME or Forensic Pathologist. To Become a Forensic Pathologist – – – – Four years of undergraduate school Four years of medical school Internship and residency in pathology Residency in Forensic pathology Less than 1,000 board certified forensic pathologists in the U.S. Medical Examiner’s Duties Visits death scene on request – responds or has an investigator respond to all homicide related deaths Reviews field investigative information Performs autopsy (aka “posts”) –Autopsy means to “see for yourself” Orders all ancillary tests & exams Provides consultation to DA Provides conclusions as to cause and manner of death What types of death need investigating? Violent Deaths (homicide, accidents, suicide) Suspicious Deaths Sudden and unexpected Deaths without a physician in attendance Death in custody Deaths during or after a medical or surgical procedure Death Investigator Works for Coroner/ME Office Reports to the medical examiner or pathologist performing the autopsy. Goes to the death scene and make an evaluation. Gathers relevant medical history as well as talks to witnesses and relatives about the decedent’s last whereabouts. Reports death to the next of kin. Death Investigator Usually an individual with law enforcement training or a: – Licensed registered nurse or – Trained mortician Must attend the PC 832 course. Must attend the coroner’s investigations academy after being hired by the coroner’s office. Crime Scene Technician Usually a member of local law enforcement. – Typically civilian personnel The technician’s expertise includes: – Photographing and diagramming the death scene. – Collecting all potentially important evidence. – Recovering fingerprints – Recovering other prints such as shoes and tires Criminalist The expert who works in the forensic lab. – Has a Master’s degree in criminalistics/forensic science – Most criminalists work with one particular type of evidence, such as: Blood Bullets Ammunitions Fibers Hair Impressions Other Types of Forensic Investigators Other specialists include: – – – – – – – – – Serologists Questioned Document Examiner Toxicologist Anthropologist Odontologist Radiologist Entomologist Botanist Meteorologist Forensic Pathologist – At scene of death controls body – Performs autopsies – Determines cause of death Death Investigator – Works for the CO/ME office – Investigates cause of death Crime Scene Investigator – Works for law enforcement – Collects evidence – Takes photographs Criminalistic Specialist – Processes evidence in the laboratory Forensic medicine is the application of various medical specialties to legal issues. Pathology refers to the study of disease. Forensic Pathologist is a medical doctor who studies injuries and disease to determine the cause and manner of death. (in suspicious deaths) Medical Examiner is a forensic pathologist who conducts autopsies to determine the cause, manner, and mode of death by examining the internal organs of the corpse. Coroner is a public officer whose primary function is to investigate by inquest any death thought to be of other than natural causes. Is a coroner the same as a medical examiner? Each state has a law requiring that either a coroner or a medical examiner oversee the investigation of unexpected deaths. Click here to watch video-clip Medical Examiners vs Coroners As you watch the video record the differences and similarities between medical examiners and coroners Forensic Evidence Evidence: Anything that can be used to determine whether a crime has been committed. – May exonerate the innocent – Corroborate or refute an alibi or statement of a witness – Identify a perpetrator or victim – Induce a confession Forensic Evidence Direct Evidence: Establishes a fact – Eyewitness testimony – Confession Circumstantial Evidence: Requires that a judge and/or jury make an indirect judgment or inference about what happened. No absolute proof; provides a general idea of what happened. Often much more reliable than Direct Evidence. – Fingerprints – Hair – Fibers Forensic Evidence Forensic evidence can’t find and convict the criminal unaided. It provides an additional weapon in the detective’s armory. – It can offer clues to help the detectives track down the criminal and – It can help detectives prove a suspect was present at the crime scene or committed a particular act of violence. Medicolegal Investigations Duties of the medicolegal system – Determine cause, manner, mechanism and time of death Four important medicolegal elements of death investigation. – – – – – Identify the deceased if unknown Collect evidence from body Document injuries or lack thereof Deduce how injuries occurred Provide expert testimony if case goes to trial Definition of Death In 1968 Black’s Law Dictionary defined Death as: the cessation of life; the ceasing to exist; defined by physicians as the total stoppage of the circulation of the blood, and cessation of vital functions consequent thereon, such as respiration, pulsation, etc. What is Death? Cellular Death – The tissues and their constituent cells are dead. No longer function or have metabolic activity, primarily aerobic respiration From cardiorespiratory failure Different tissues die at different rates Definition of Death Clinical Death – The cessation of respiration and circulation functioning. Resuscitation may or may not be possible. Anoxia and hypothermia – May live for more than 5 minutes after cessation of respiration and circulation. What is Death? Somatic Death – Irreversible loss of personality, being unconscious, unable to be aware of or communicate with one’s environment, unable to appreciate any sensory stimuli or to initiate any voluntary movement. – Reflex nervous activity may persist and circulatory and respiratory functions continue either spontaneously or with artificial support so that the tissues and cells of the body, other than those already damaged in the central nervous system, are alive and functioning. Definition of Death Brain Death – An irreversible process. – Irreversible cessation of all brain functions, including brain stem. – PVS – Persistent Vegetative State = permanent damage to frontal lobe function and not brain stem. Definition of Death Brain Death is determined by: – – – – – Coma and cerebral responsiveness Apnea Fixed and Dilated Pupils Absence of Cephalic Reflexes (brainstem) Absence of Electrical Impulses in the Cerebrum(no EEG pattern) Two physicians required to pronounce brain death; one must be a neurologist in California. Death Certificate Medicolegal certificate requirement of the death – Cause and – Manner of Death Death Certificate The death certificate has two major groupings for the cause of death: – Primary or immediate cause of death – Secondary cause of death Primary Cause of Death The Primary cause of death is subdivided into a three-link sequential chain – Primary cause of death: Hypoxemic necrosis of brain (brain death) due to Exsanguination due to Gunshot wound (GSW) of abdomen Secondary Cause of Death Includes conditions which are not related to the primary cause of death but are substantially contributory to the individual’s demise – Emphysema of the lungs – Arteriosclerotic cardiovascular disease Cause of Death The reason someone dies is the cause of death Proximate cause of death refers to an underlying cause of death as opposed to the final cause. – The “original” underlying medical condition which initiates a lethal chain of events culminating in death. i.e.. a shotgun blast to the head, stab wound to the chest or coronary atherosclerosis. Immediate cause of death – What kills a person now, but was originally precipitated by something else (proximate) Mechanism or Mode of Death An abnormal physiological state that pertained at the time of death – i.e. coma, congestive heart failure, cardiac arrest, pulmonary edema, septicemia and hemorrhage Mechanism of death describe the specific change in the body that brought about the cessation of life. – **usually only “Cause” and “Mechanism” are listed on the dead certificate** Manner of Death The circumstances surrounding a death or how the cause of death came about. Circumstantial events or manner of death may be: – Natural due to disease or – Unnatural due to: Accident, Suicide, Homicide, Questionable/Undetermined. NASH/Q Certification of Death Five Classifications of Death (NASH/Q) Referred to Manner of Death – – – – – Natural: pathology; death caused by disease. Accident: not intentional or by a criminal act. Suicide: death by one’s own hand. Homicide: death by another. Questionable: cause and/or motive is not known; generally when other classifications are not used. Also “Undetermined” death is used. “Equivocal” has also been used as well. Examples: Manner of death: - homicide Cause of death: - smothering Mechanism of death: - asphyxia Manner of death: - homicide Cause of death: - stabbing Mechanism of death: - loss of blood Man shot during robbery. Man stabilizes. Develops pneumonia. Followed by kidney failure, liver failure, heart failure, death. Had prior lung and heart disease, and probably would have survived if not for these diseases. Manner of death: - homicide Cause of death: - gunshot Mechanism of death: - heart failure REVIEW CAUSES AND MECHANISMS OF DEATH Examples of causes of death: heart attack, gunshot wound, skull fracture, diseases or injuries, stroke, burning, drowning, strangulation, hanging, suffocation, massive trauma, bludgeoning Examples of mechanisms of death: Exsanguination (bleeding to death) Sepsis (infection in blood stream) Brain trauma (cerebral contusion) Brain bleeding (intra-cerebral bleed) Stop breathing (asphyxia) Pulmonary arrest Cardiac arrest Whitney Houston death certificate: No cause of death listed Click here ← to read the news article. The manner, cause and mechanism of death of: •Jon Bennet Ramsey –Manner – homicide –Cause – strangulation –Mechanism – asphyxiation - respiratory arrest •Whitney Houston –Manner – accidental –Cause – drowning –Mechanism – Pulmonary arrest • – – – Michael Jackson Manner – homicide Cause – acute propofol intoxication Mechanism – cardiac arrest • Hugo Chavez – Manner – natural – Cause – heart attack – Mechanism – Pulmonary arrest You try Write a short scenario that includes information about cause, manner and mechanism of death, without labeling them as such. Exchange your scenario with other students and try to classify theirs. Death Certificate Cause of death written on the death certificate: – Primary or Immediate – Secondary Death Certificate Primary cause of death – Subdivided into a three-link sequential chain, eg. Hypoxemic necrosis of brain (brain death) – Due to Exsanguination – Due to Gunshot wound Death Certificate Secondary cause of death – Includes conditions which are not related to the primary cause of death but are substantially contributory to the individual’s demise Emphysema of lungs, Hypothermia Arteriosclerotic cardiovascular disease Autopsy Reports Cause of death: Heart failure with cardiac arrhythmia due to a pulmonary emboli. Contributing cause: Intestinal dismobility, on chronic pain management. Manner of Death Undetermined. Autopsy Report A Psychological Autopsy may have to be done if manner of death is thought to be suicide. – An investigation of a decedent’s mental state prior to death. Autopsy Final photo of the King. Autopsy Autopsy Photo of Marilyn Monroe Identification of the Deceased Physical Description – Height – Weight – Color of eyes, hair and skin Scars and Marks – Birthmarks, scars, etc. – Tattoos Fingerprints Identification of Deceased Identification of Deceased Identification of the Deceased Photographs – The entire body should be photographed. Radiological Features – X-rays should be taken of the body. Identification of the Deceased Age Determination – Age may be roughly estimated by the teeth – Joining of the bones (epiphysis) – Ossification center Dental Features – The pattern of dental work may be determined by an Odontologist. – Eruption of Teeth Identification of Deceased Blood Factors – ABO groupings, Rh factors, DNA testing. Medical Indications – Postmortem may reveal preexisting diseases. Any Other Means Available – Clues may be found at the scene or in the personal effects. Definition of Murder P.C. 187: Unlawful killing of human being, or fetus, with malice aforethought. – 1st Degree: by any of the destructive devices or explosive, use of ammo designed primarily to penetrate metal or armor, poison, lying in wait, torture, other willful, deliberate, premeditated killing, committed or attempted during a burglary, arson, rape, robbery, mayhem, carjacking, kidnapping, train wrecking or a drive-by shooting with intent to kill. First-Degree Murder in California Law California law, there are three ways to be convicted of first-degree murder: – By committing the murder using: a destructive device or explosive, weapon of mass destruction, ammunition primarily designed to penetrate metal or armor or poison, or by lying in wait or by inflicting torture, – By killing in a way that is willful, deliberate and premeditated, OR – By way of the felony-murder rule (that is committing a specifically enumerated felony that automatically turns any logically relate death into first-degree murder). Second Degree Murder Willful murder but is not deliberate and premeditated. – Second-degree murder is any murder that isn't defined as first-degree murder. Shooting a gun into a crowded room and killing someone, even if that wasn't your intention Vehicular Manslaughter; intoxicated driver. Degrees of Murder – Manslaughter: Unlawful killing of a human being, without malice. Voluntary: A sudden quarrel or in the heat of passion. Involuntary: While committing an unlawful act, not a felony; or while committing a lawful act that might produce death, done in an unlawful manner; or without due caution and circumspection; provided that this subdivision shall not apply to acts committed in driving of a vehicle. Vehicular: Drives in an unlawful way that produces death Homicide Justifiable Homicide: – Public Officer: Homicide justifiable when committed by public officer, and those acting by their command in their aid and assistance. – Other Persons: (Including Peace Officers): When committed by a person in the following cases. Resisting an attempted murder or felony. In defense of habitation, property or person. In lawful defense of persons such as wife, husband, child or parent. In attempt to apprehend a person for committing a felony, lawfully suppressing a riot or lawfully keeping or preserving the peace. Case 1 A 25 year old man was shot in the abdomen with a handgun. He was taken to the hospital where he underwent an emergency exploratory laparotomy. All life-threatening injuries were repaired. His postoperative course, however, was complicated by peritonitis which led to sepsis and eventually death two weeks after surgery. An autopsy revealed an extensive abdominal infection. The medical examiner ruled the cause of death as a gunshot wound to the abdomen and the manner of death as a homicide. Case 1 During the trial, the pathologist was questioned about the cause of death. The pathologist reiterated his opinion that the decedent died from a gunshot wound. A fierce crossexamination followed. The defense attorney contended the man died as a result of an abdominal infection. Consequently, it was the physician, not his client, who was to blame for the death. Case 1 Who should the jury believe? Would the victim have died if the infection had been discovered sooner? Should the physician be responsible for the man’s death? Case Discussion Case 1 This man died as a result of a gunshot wound to the abdomen and the manner of death was homicide. It was a lifethreatening injury which would have caused his death within hours if he had not been treated. A well-recognized risk of abdominal surgery is peritonitis. If he had been admitted with a non-lethal injury, and the physician made an error in judgment which caused his death, then the manner of death would have been an accident, not homicide. Case Discussion Case 1 In this case, however, the pathologist correctly stated that the sequence of events was continuous from the time the man was shot until he died. In the state of California the statute of limitations for this type of crime leading to the person’s death is one year Case 2 A woman in her seventies was walking to a grocery store. An assailant pushed her onto the sidewalk as he grabbed her purse. She was apparently unharmed but obviously shaken by the experience. Within 10 to 15 minutes she developed shortness of breath, increased chest pain and was taken to a nearby emergency room. During her evaluation she developed an arrhythmia and died. Case 2 An autopsy revealed severe atherosclerotic disease in all coronary arteries and numerous infarcts of the left ventricle. There were no signs of injury from the fall. The medical examiner ruled the cause and manner of her death as heart disease and homicide, respectively. Case 2 During the trial, the defense attorney disagreed with the cause and manner of death. He stated this was not a homicide because the woman died of heart disease, and the fall to the sidewalk caused by his client was not a contributing factor. Was the pathologist correct? Should he have called the death a homicide? Did the man who took her purse actually cause her death? Case Discussion Case 2 This case is more complex than Case 1. The manner, not the cause, of this woman’s death is in dispute. Since there was no significant trauma, the cause of death had to be the heart disease. He was more concerned with the sequence of events and how the pathologist believed the robbery was directly related to the death. Case Discussion Case 2 There was only a 10-15 minute interval from the time the woman was knocked to the ground to when she experienced signs and symptoms of a heart attack or angina. Since the time period was short, the pathologist believed that the woman was still under stress and correctly interpreted the manner of her death as a homicide. The longer the time frame, however, between the incident and heart attack, the more difficult it would be to make this interpretation. Case Discussion Case 2 If, for example, the woman had gone home, had not been seen for a few hours, and then complained of chest pain, the same interpretation could not have been made. She would have been unwitnessed during that time and some other incident could have triggered a fatal arrhythmia. Consequently, in such a situation, her death could not be ruled a homicide.