Abnormal psychology and therapy (1)
advertisement

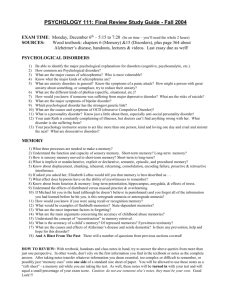
Abnormal Psychology and Therapy By Jake Russell, Jesus Davis, and Thomas Shaw Abnormal Behavior • • • • • • • Behavior that is deviant, maladaptive, or personally distressful over a long period of time atypical from the majority of what society considers acceptable interferes with person’s ability to function in the world person engaging in behavior is troubled by it includes Anxiety, Somatoform, Factitious, Dissociative, Mood, Schizophrenia, Eating, and Sleep disorders abnormal behavior classification can lead to a stigma stigma is a mark of shame that causes others to act negatively toward individual Approaches To Abnormal Behavior • • • • • Biological approach emphasizes medical model, which describes psychological diseases as having a biological origin Disorders referred to as mental illnesses Sociocultural approach stresses how culture and socioeconomic background influence disorders Social, economic, technological, religious factors affect frequency and intensity of disorders Bio psychosocial approach states that disorders caused by sociocultural, psychological, and biological factors working together Classifying Abnormal Behavior • • • • • • • DSM-IV classification system classifies based on 5 axes axis I: all diagnostic categories except personality disorders/mental retardation axis II: personality disorders and mental retardation axis III: general medical conditions axis IV: psychosocial/environmental problems axis V: current level of functioning critiques include the manual classifies based on medical model, and focuses solely on problems instead of strengths as well Therapy • • Biological Therapies- also called biomedical therapies, treatments that reduce or eliminate the symptoms of psychological disorders by altering aspects of body functioning. Antianxiety Drugs- Commonly known as tranquilizers, drugs that reduce anxiety by making the individual calmer and less excitable. • Antidepressant Drugs- drugs that regulate mood, to help alleviate depressed mood through their efforts on neurotransmitters in the brain. Therapy (Continued) • Antipsychotic Drugs- Powerful drugs that diminish agitated behavior, reduce tension, decrease hallucinations, improve social behavior, and produce better sleep patterns in individuals with a severe psychological disorder, especially schizophrenia. • Electroconvulsive Therapy(ECT)- Also called shock therapy, a treatment, commonly used for depression, that sets off a seizure in the brain. This idea of setting off a seizure has actually been around since Hippocrates. https://www.youtube.com/watch?v=9L2-B-aluCE Increase Suicide Risk in Children • • • The FDA reviewed clinical trials of antidepressant use with children, who were randomly assigned to receive either an antidepressant or a placebo. • • None of the children in the studies committed or attempted suicide. “Adverse event reports” were also examined- spontaneous statements of thoughts about suicide reported by the participants or their parents. • Research did show an increase in adverse event reports in the participants. Placebo participants showed 2% of spontaneous reports of suicidal thoughts, participants taking antidepressants showed 4%. This finding was the basis of the FDA’s action to require prescription antidepressants to carry the severest “black box” warning. Drug Chart Psychosurgery • • A biological therapy, with irreversible effects, that involves removal or destruction of brain tissue to improve the individual’s adjustment. Antonio Egas Moniz developed a surgical procedure, where an instrument is inserted into the brain and rotated, severing fibers that connect the frontal lobe and the thalamus. • • Moniz believed that the procedure should be use with extreme caution and only be used as a last resort, due to the fact that it can leave some patients in a “vegetable-like state.” Maybe performed for OCD, major depression, or bipolar disorders. Schizophrenia Symptoms • ● Schizophrenia - Severe psychological disorder characterized by highly disordered thought processes, referred to as psychotic because they are so far removed from reality Positive Symptoms - Distortion or excess of normal function ○ Hallucinations - Sensory experiences in the absence of real stimuli ○ Delusions - False, unusual, and sometimes magical beliefs that are not part of an individual’s culture ○ Referential thinking - Ascribing personal meaning to completely random events ○ Catatonia - State of immobility and unresponsiveness for long periods of time ● Negative Symptoms - Social withdrawal, behavioral deficits, loss or decrease of normal functions ○ Flat affect - The display of little or no emotion -- common ● Cognitive Symptoms ○ Difficulty keeping attention ○ Memory problems ○ Inability to interpret information and make decisions Causes of Schizophrenia • Heredity o ● Research supports it is at least partially caused by genetic factors. As genetic similarities to a person with it goes up so does the risk of getting it. Researchers are seeking the location of genes involved in susceptibility to schizophrenia. ● Structural Brain Abnormalities ○ Enlarged ventricles in the brain. Indicates deterioration in other brain tissue. Small prefrontal cortex and lower activity in the area. Microscopic studies of brain tissue after death shows small changes in the distribution or characteristics of brain cells. Problems appear prenatal. Neurotransmitter Regulation Problems ○ Linked excess dopamine production to schizophrenia. First noticed with study involving the drug L-dopa and Parkinson’s disease. The person is bombarded with thoughts and they might think those thoughts are someone else’s voice talking inside their head. But when levels are balanced they might still hang on to their prior beliefs. Kapur says delusions serve as explanatory schemes that have helped the person make sense of the random and chaotic experiences caused by all of the dopamine. Factors of Schizophrenia • Psychological Factors o Diathesis- Stress Model - View of schizophrenia emphasizing that a combination of biogenetic disposition and stress causes the disorder o Used to explain schizophrenia as rooted in an individual’s difficult childhood experiences with parents ● Sociocultural Factors ○ They appear to affect the course of the disorder. Influence how schizophrenia progresses. ○ Individuals with schizophrenia in developing, non industrialized nations tend to have better outcomes than those in developed, industrialized nations Schizophrenia Case Study and Video Jack is a 27 year old man diagnosed with schizophrenia. He has been referred to Top Quality Rehabilitation (TQP) to provide supported employment services. Jack graduated from high school and got a job working in a video store. After working for about 6 months Jack began to hear voices that told him he was no good. He also began to believe that his boss was planting small video cameras in the returned tapes to catch him making mistakes. Jack became increasingly agitated at work, particularly during busy times, and began "talking strangely" to customers. For example one customer asked for a tape to be reserved and Jack indicated that that tape may not be available because it had "surveillance photos of him that were being reviewed by the CIA". After about a year Jack quit his job one night, yelling at his boss that he couldn't take the constant abuse of being watched by all the TV screens in the store and even in his own home. Jack lived with his parents at that time. He became increasingly confused and agitated. His parent took him to the hospital where he was admitted. He was given Thorazine by his psychiatrist, this is a very powerful psychotropic medication. However, he had painful twisting and contractions of his muscles. He was switched to Haldol and had fewer side effects. From time to time Jack stopped taking his Haldol, and the voices and concerns over being watched became stronger. During the past 7 years Jack was hospitalized 5 times. He applied for and now receives SSI, and with the assistance of a case manager has moved into his own apartment. He is now a member of a psychosocial "clubhouse" for people with mental illness. He attends the clubhouse 3 times a week. He answers the phone, and helps write the clubhouse newsletter. He has a few friends at the clubhouse, but he has never had a girlfriend. Jack told his case manager he would like to get a job so he can earn more money and maybe buy a car. Jack is very worried about looking for a job. He doesn't know how to explain his disorder to a potential employer, and he is afraid of becoming overwhelmed. He likes movies and would like to work with them in some manner. http://www.youtube.com/watch?v=bWaFqw8XnpA Mood Disorders • • Are psychological disorders in which there is a primary disturbance of mood: prolonged emotion that colors the individual's entire emotional state. Can include cognitive, behavioral, and somatic symptoms, as well as interpersonal difficulties. Two main types are depressive and bipolar disorder. Often leads to suicide. Depressive Disorders are mood disorders in which the individual suffers from depression: an unrelenting lack of pleasure in life. They are common. o Major depressive disorder (MDD) involves a significant depressive episode and depressed characteristics, such as lethargy and hopelessness, for at least two weeks. o Dysthymic disorder (DD) is mood disorder that is generally more chronic and has fewer symptoms than MDD; the individual is in a depressed mood for most days at least two years as an adult or at least one year as as a child or an adolescent. Factors of Depressive Disorders Biological Factors Psychological Factors • • • Genetics influences , such as specific brain structures and neurotransmitters, play a role in depression. Depressed individuals show lower levels of brain activity in a section of the prefrontal cortex that is involved in initiating behavior. Depression likely involves problems in the body’s regulation of a number of neurotransmitter. Individuals with major depressive disorder appear to have difficulty regulating the neurotransmitter serotonin or too few receptors for serotonin and norepinephrine. • When people cannot control their stress, they eventually feel helpless and stop trying to change their situations, this learned helplessness turns into hopelessness. Depression is thought to be related to a pessimistic attributional style: blaming oneself for negative events and expecting the negative events to recur in the future. Sociocultural Factors • Individuals with a low socioeconomic status (SES), especially people living in poverty, are more likely to develop depression than their higher-SES counterpart. Depression Among Men & Women Across Cultures • • Beirut, Lebanon has the highest depression and Korea has the lowest. Florence, Italy has the biggest difference in depression by 12.5 males. Depressed Children • • • The Prevalence of major depressive disorder among children ranges from 1.5-2.5% in school-age children and 15-20% in adolescents. Higher risk of substance abuse, academic problems, increased physical illness, and others. Provide the child with love, encouragement, and a role model or a strong extended family that supports the child’s attempt to cope with difficulties. Bipolar Disorder • • • Is a mood disorder that is characterized by extreme mood swings that include one or more episodes of mania, an overexcited, unrealistically optimistic state. Bipolar I Disorder- individuals who have manic episodes during which they may experience hallucinations. Bipolar II Disorder- the individual may not experience full-blown mania but rather a less extreme level of https://www.youtube.com/watch?v=fyJn_3LkE8w euphoria. Suicide • • • Not a diagnosable disorder but a tragic consequence of psychological disorders, most commonly depression and anxiety. Biological Factors- Tends to run in the family, have low serotonin levels, and poor physical health. Psychological Factors- Mental disorders and traumas such as sexual abuse. • Sociocultural Factors- Chronic economic hardship can be a factor in suicide, and cultural and ethnic contexts also are related to suicide attempts. Mood Disorders (Continued) Symptoms: feelings of sadness hopelessness helplessness suicidal thoughts fatigue mania changes in appetite • • • • • • • Treatments: support groups individual therapy antidepressants cognitive behavioral therapy psychodynamic therapy family therapy • • • • • • Mood Disorder Case Study Jessica is a 28 year-old married female. She has a very demanding, high stress job as a second year medical resident in a large hospital. Jessica has always been a high achiever. She graduated with top honors in both college and medical school. She has very high standards for herself and can be very self-critical when she fails to meet them. Lately, she has struggled with significant feelings of worthlessness and shame due to her inability to perform as well as she always has in the past. For the past few weeks Jessica has felt unusually fatigued and found it increasingly difficult to concentrate at work. Her coworkers have noticed that she is often irritable and withdrawn, which is quite different from her typically upbeat and friendly disposition. She has called in sick on several occasions, which is completely unlike her. On those days she stays in bed all day, watching TV or sleeping. At home, Jessica’s husband has noticed changes as well. She’s shown little interest in sex and has had difficulties falling asleep at night. Her insomnia has been keeping him awake as she tosses and turns for an hour or two after they go to bed. He’s overheard her having frequent tearful phone conversations with her closest friend, which have him worried. When he tries to get her to open up about what’s bothering her, she pushes him away with an abrupt “everything’s fine”. Although she hasn’t ever considered suicide, Jessica has found herself increasingly dissatisfied with her life. She’s been having frequent thoughts of wishing she was dead. She gets frustrated with herself because she feels like she has every reason to be happy, yet can’t seem to shake the sense of doom and gloom that has been clouding each day as of late. This demonstrates major depressive disorder where it’s only a 2 week long episode with a feeling of hopelessness. Anxiety Disorders • • Involve fears that are uncontrollable and disproportionate to the actual level of danger, and disruptive of day-to-day life characterized into five typesgeneralized anxiety disorder, panic disorder, phobic disorder, obsessive-compulsive disorder, and post-traumatic stress disorder Are Psychological Disorders a Myth? • • • • • • NAMI, American Psychiatric Association, and NHMA all agree that mental illnesses are very real medical conditions Some claim that mental illnesses are better labeled “problems of living” Number of ADHD diagnoses caused some to wonder if normal behavior is being labeled as psychology NIMH sponsored a conference to review the scientific evidence conference concluded that ADHD was a real disorder controversy serves as a reminder of the role of research in clarifying and defining diagnostic categories GAD (Generalized Anxiety Disorder) • • • • marked by persistent anxiety for at least 6 months unable to specify reason for anxiety nervous all the time worry about work, relationships, health GAD (cont.) • • excessive worrying can cause fatigue, muscle tension, stomachaches, and difficulty sleeping factors include genetic predisposition, sympathetic nervous system activity, harsh/impossible self standards,overly strict parents, and history of uncontrollable traumas/stressors (abusive parent) Anxiety Disorder Case Study Nancy L., a 45-year-old married lawyer, presented with exacerbation of her chronic generalized anxiety and recurrent depressive symptoms in January 2005. Nancy had a history of anxiety dating back "as far as I can remember." She was an anxious young girl with separation anxiety and shyness that manifested in elementary school. As she grew up, she experienced ongoing anxieties about the health of her parents (worrying that her parents would die, even though they were in good health) and her school performance (though she was a good student). She remembers marked fears, including fears of the dark and thunder, most of which she "outgrew" except for a persistent fear of insects, particularly spiders. Her anxiety became more prominent and persistent after she left home at age 18 and entered college. She sought care at the university health service and received a prescription for diazepam that she used over the next 4 years on an as-needed basis during periods of increased anxiety such as examinations; she also met episodically with a therapist at the counseling center. In the spring of her freshman year, she experienced her first major depressive episode following a break-up with a boyfriend. She was prescribed imipramine, which she took for a couple of months but then discontinued because of intolerable side effects (dry mouth and lightheadedness). The depression gradually resolved over the next 6 months. Nancy continued to be plagued by persistent feelings of anxiety and worry associated with insomnia, irritability, tension, and fatigue. Over the years, her friends and family chided her for "worrying too much," and she reported difficulty controlling her anxiety over her financial situation, job security, and her children's safety, despite evidence that none of these were problematic. Her husband reported that he found her persistent anxiety and ongoing need for reassurance "exhausting" and that he noticed himself withdrawing from her, which led to significant tension between them. The high quality of her work at the law firm was recognized and she was well-compensated financially, yet she continued to worry about her performance and was, in fact, passed over for promotion to team leader because, as one of her annual reviews stated, her "constant anxiety makes everyone else too nervous." In addition, over the last 25 years, she has had 5 or 6 episodes of major depression lasting from 3 to 4 months to over a year. These episodes have sometimes, but not always, been triggered by situational stressors; one occurred during a postpartum period. After college, she was treated intermittently with benzodiazepines at low doses (eg, diazepam 5-10 mg), which she took on an as-needed rather than daily basis when the anxiety worsened because of her concerns about addiction. As noted, she was briefly on imipramine during college but discontinued it because of side effects. About 10 years before the January 2005 examination, she was started on fluoxetine 20 mg/day by her primary care doctor. She discontinued it after a few days because it made her feel jittery and more anxious. She had been in supportive therapy on and off since college to help her deal with situational stressors. Other relevant aspects of her medical and psychiatric history include the fact that her overall health had been generally good, although she had presented numerous times to her primary care physician with a variety of somatic complaints, including headaches, gastrointestinal disturbance, and muscular aches and pains with no clear etiology. She had repeated thyroid testing with normal results. Her mother had had a history of menopause in her early 40s and the patient noted that her menstrual cycles had become more irregular over the last couple of years, and her anxiety and irritability become notably worse premenstrually. She smoked a pack of cigarettes a day and reported that having a cigarette would sometimes temporarily decrease her tension and anxiety. She attempted to quit smoking several times and noted that the increased anxiety and tension she experienced during these attempts contributed to her lack of success in these efforts. She typically had 1 or 2 glasses of wine at social occasions or on the weekends; she has no history of abuse or dependence on alcohol but did say that a glass of wine made her feel temporarily less anxious. She carefully monitored her intake because of worry that she would become an alcoholic. She smoked marijuana a few times in college but it made her feel dysphoric and more anxious, and she had not used it or other illicit drugs since that time. Social and Family History After finishing college, Nancy went to law school, where she met her husband. She reported being attracted to his sense of calm and stability. He reported that part of what drew him to her was the sense of how much she seemed to need and depend on him. They were married shortly after graduation and had 2 children over the next 5 years. After the birth of her second child, she developed a postpartum depression that lasted almost a year and for which she didn't seek treatment. She said that her youngest child "is just like I was -- she's afraid of her own shadow." She grew up in a middle-class home, the second of 3 children. She reported that childhood was "generally happy," although she was troubled by anxiety starting early in life. There was no history of physical or sexual abuse. Both parents were still alive in January 2005, although they had significant medical conditions and she was worried about their health. She noted that her mother and father were both "nervous" people, and though never formally diagnosed and treated, her maternal grandmother had a history of depression Panic Disorder ● person experiences sudden, recurrent onsets of intense apprehension or terror ● often without warning/specific cause ● symptoms: ● severe palpitations, shortness of breath, chest pains, trembling, sweating, dizziness, feeling of helplessness Panic Disorder (cont.) • • Biological: • • Sociocultural: genetic predisposition, overly active autonomous nervous system, problems with norepinephrine/GABA American Women twice as likely as men to experience panic attacks, biological differences in hormones/neurotransmitters Phobic Disorder • • • • irrational, overwhelming, persistent fear of a particular object or situation GAD sufferers cannot pinpoint source of anxiety, those with phobias can fear changes to phobia when individual goes to extreme lengths to avoid it typically begin in childhood Phobic Disorder (cont.) ● Biological: ● neural circuit for phobias that includes thalamus, amygdala, and cerebral cortex ● number of neurotransmitter, especially serotonin ● Psychological: ● phobias could be learned fears Obsessive Compulsive Disorder (OCD) • • • • • • • anxiety-provoking thoughts that will not go away urges to perform repetitive, ritualistic behaviors rituals prevent future situations Obsessions are recurrent thoughts Compulsions are recurrent behaviors repeat routines up to 100s of times a day most do not enjoy ritualistic behavior OCD (cont.) • • • • • Biological: Genetic component, neurological links, frontal cortex and basal ganglia are so active that impulses reach the thalamus, amygdala may be smaller, low levels of serotonin/dopamine Psychological: occurs during period of life stress individuals do not have the ability to turn off negative thoughts Post Traumatic Stress Disorder (PTSD) ● ● develops through exposure to traumatic event that overwhelms abilities to cope ● can follow immediately after or years after ● traumas include war/combat, natural disasters, sexual abuse/assault, unnatural disasters such as car crashes/terrorist attacks PTSD (cont.) • • • • • • • flashbacks avoidance of emotional experiences reduced ability to feel emotions, inability to experience happiness/desire excessive arousal, exaggerated startle response/inability to sleep difficulties with memory/concentration feelings of apprehension impulsive outbursts of behavior PTSD (cont.) • • • • primary cause is traumatic event itself other factors can influence vulnerability history of previous traumatic events conditions such as abuse/psychological disorders http://www.youtube.com/w atch?v=-Fc6_aTnRXQ Reference Slide Thomas Shaw: Presented the topics of abnormal behavior and anxiety disorders( #’s 1&2) and created guided notes. Jesus Davis: Presented the topics of therapy and mood disorders( #’s 3&8) and mood disorder case study. Jake Russell: Presented the topic of Schizophrenia(# 5) and Schizophrenia case study.