1013 kB - Anaesthesia in scoliosis
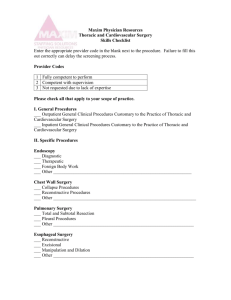
advertisement

Anaesthesia in scoliosis Dr. S. Parthasarathy MD., DA., DNB, MD (Acu), Dip. Diab.DCA, Dip. Software statistics PhD (physio) Mahatma gandhi medical college and research institute, puducherry, India What is it ?? • Scoliosis is a lateral curvature and rotation of the thoraco-lumbar vertebrae(commonly) with a resulting rib cage deformity. When it is problematic – cobb angle • > 10 * abnormal • > 65* respiratory • > 100 * Rt HF • > 40 * - surgery • 1 to 2 degrees/year The initial classification was given by Schulthess W • • • • • Cervico thoracic Thoracic Thoracolumbar Lumbar Combined double primary The list is very big • Idiopathic common – 70 % cases • Neuropathic Poliomyelitis Syringomyelia Friedreich’s ataxia • Myopathic Myopathies • Osteopathic vertebral anomalies – infection, TB, tumors Incidence • 10 -- 30 degrees – 3 % • more than 30 degrees -- 0.3 % • Adolescents • Female : male -- 3:1 Why to correct ?? • • • • to correct the curve fuse the spine, improving posture halting the progression of pulmonary dysfunction. • The approach may be • posterior, anterior or combined • depending on the cause and severity of the curvature Correction – example Preanaesthetic check up What is special ?? Location ?? Etiology?? Airway assessment • upper thoracic or cervical spine • Traction devices • Duchenne – tongue hypertrophy • discuss preoperatively the stability of the spine with the surgeon • previous radiotherapy of the head and neck can cause diffculty in direct laryngoscopy Airway assessment • Xrays and CT scan neck SOS • A decision must be made, whether to intubate the patient awake or asleep. Respiratory system • • • • Restrictive lung defect VC decrease TLC decrease RV may increase RV /TLC increase ? Allow full exhalation • Secretions retained infections • Resp. Rate may increase Scoliosis and loss of lung volume The problems are • abnormal thoracic cage geometry producing a marked decrease in chest wall compliance • There is a mechanical defect • Exceptions include congenital and infantile scoliosis where there is lung hypoplasia Factors • More than 70 degrees and • More than 7 vertebrae • Hypoxemia, progressing to PHT and Rt heart failure – not necessarily hypercarbia Responses abnormal ventilatory patterns in response to hypoxemia and hypercarbia Factors associated with postoperative mechanical ventilation requirements • pre-existing neuromuscular disease, • severe restrictive pulmonary dysfunction with a vital capacity(VC) of <35% predicted • congenital heart defects, • Right ventricular failure, • obesity, • anterior thoracic spine surgery • blood loss of >30ml/kg Preop correction • Infection • Bronchodilators • Incentive spirometry Cardiovascular system • Less common • But more dangerous Cardiovascular system • • • • ↑ PVR PHT and RVF. mitral valve prolapse restrictive pericarditis with a possible secondary pericardial effusion. • Limited cardiac filling decreases any potential increases in cardiac output – surgery and anaes ?? • Duschenne – cardiomyopathy • Marfan s – AR and MR ECG • • • • • Tachycardia, prolonged PR and QRS intervals, ST abnormalities, bundle branch block, Q waves in the left precordial leads and tall R waves in the right precordial leads. • Ejection fraction may be decreased on echocardiogram. Special in preop • When does it start • The number of alveoli increases from approximately 20 million at birth to 250 million at 4 years of age • Where is it ?? • Cervical or thoracic • Number of vertebrae ?? Preop summary • • • • Airway CVS RS Neuro • History examination and document Investigations • • • • • • • Routine Xrays ECG Echo PFT Blood grouping and typing rehearse the wake-up test during the preoperative visit . Premedication • Antisialogogue – FOL , position • Antibiotics and bronchodilators • Preop prophylaxis with high dose corticosteroids should be considered for patients with a preexisting neurologic deficit. • Sedatives and heavy narcotics ? • DVT --- The use of compression stockings and/or pneumatic boots is recommended Anaesthetic techniques General anaesthesia Induction • Intravenous is ideal • no to Scoline • hyperkalemic response in presence of myopathies or denervation. • It may also cause malignant hyperthermia in certain syndromes Intubation • FOL awake • NDPs • Double lumen tube in anterior approach to thoracic spines Positions • Anterior approach to thoracic spine • Posterior approach to lumbar spine • Anterior approach to lumbar spine • Position changes intraop • Peripheral nerves, eyes, genitals and bony points should be padded and protected Monitoring • ECG ,SPO2,Temperature,ETCO2, urine output , blood loss , NMJ monitoring • CVP monitoring according to necessity • Open chest and prone position – role of CVP ?? • TEE better than CVP in prone position ?? • Catheter and output – monitor both !! Arterial line • The prolonged anaesthesia in unusual positions, combined with significant blood loss, haemodynamic effects of thoracic surgery and need for deliberate hypotension mandate an invasive arterial line. • Also serial blood gas measurements may be done where required spinal cord monitoring – stagnara • The ‘wake-up’ test provides a snapshot of spinal cord motor function. • Surgery is halted, the volatile agent switched off and emergence allowed. • The patient is asked to move their feet, ok then anesthesia can be recommenced • Beware of tubes, catheters • Any paraperesis – remove hardware, stabilize hemodynamics Defects in wake up test ?? • • • • • • Sensory deficits - ?? Preoperative paraperesis ?? Intra operative recall -- !! Temporary test – problem can come later ? Squeeze hand and then proceed !! If he does , immediate give propofol / agent/ narcotics SSEP monitoring • SSEP monitoring involves stimulating a peripheral nerve often the posterior tibial nerve, and then detecting a response with epidural or scalp electrodes. • The evoked potentials are averaged more than 2– 3 min to eliminate background noise then displayed as voltage against time. SSEP • • • • A square wave stimulus 50-250 micro sec duration, strength 20-50 mA, stimulation rate 16 Hz is commonly used. • Hypothermia, hypotension may influence SSEP SSEP • Baseline data obtained after skin incision • Responses are recorded intermittently during surgery • A reduction in the amplitude by 50% and an increase in the latency by 10% are considered significant. • SSEP tests only dorsal column function not motor • Rarely - post operative neurologic deficit reported despite preservation of SSEP intraoperatively SSEP > 10 % < 5 0 % SSEP • 0.5–1.0 MAC isoflurane, desflurane or sevoflurane. -SSEP – OK – monitoring Nitrous oxide potentiates the depressant effect of volatile anesthetics IV anesthetics generally affect SSEPs less than inhaled Etomidate ,ketamine increases cortical SSEP amplitude Opioids – not much change Neuromuscular blocking agents may reduce background noise SSEP • Bolus IV anaesthetics ?? • Wait for 5- minutes to stabilize after vaporizer dial change • Sevoflurane better if rapid changes are needed • If in doubt , perform wake up test Clonus test • Clonus can normally be elicited in patients with intact spinal reflexes and lack of central inhibition • Coming out of GA • It does not require patient cooperation • clonus can be elicited – may be an injury to cord • absence of clonus does not reliably predict injury Motor evoked potentials (MEPs) • MEP monitoring involves stimulating the motor cortex by electrical impulses transcranially and detecting the resulting signal at spinal level with epidural electrodes or from muscles as a compound muscle action potential (CMAP) • MEPs are markedly depressed by almost all anaesthetic agents • Minimum dose ketamine and record • May not absolutely reliable Motor cortex Stimulation – biceps brachii CMAP Something becomes abnormal in cord monitoring ?? • • • • Maintain BP 100 % oxygen Iv fluids Blood to correct anemia • Perform wake up test , adjust or remove instrumentation Temperature • Body temperature can decrease considerably during the operation. • Temperature monitoring, i.v. fluid warmers and warm air blankets should be commenced at induction surgery. and continued throughout Blood conservation: • Major scoliosis surgery – 10 – 30 ml /kg go upto 50 ml • Decrease surgical time • Position proper, relax abdominal muscles • Antifibrinolytic agents e.g. aprotinin inhibits plasmin and kallikrein and preserves platelet function – use as an infusion • Autologous blood donation • Hypotensive anaesthesia Postop pain relief is painful • • • • Children Large incisions Cognitive impairment Preop painful conditions Post op pain relief • Good postoperative analgesia is essential to allow frequent physiotherapy and early mobilization, and so reduce the risk of respiratory complications • Systemic opioids , NSAIDs (after 24 hours) , PCA, • paravertebral block, Epicath – can be kept by the surgeon end operatively Post op paralysis • The incidence of motor deficit or paraplegia after surgical correction of scoliosis in the absence of spinal cord monitoring, has been quoted as between 3.7 and 6.9%. • This can be reduced by intra operative monitoring to 0.5% Some more perioperative complications • • • • • • Fat embolism Air embolism Coagulopathy Visual loss Necessity for postoperative ventilation Hyponatremia Summary • • • • • • • Definition and incidence Cobbs angle and severity Etiology Pre op : : airway, RS, CVS, Neuro , premed Induction , airway, scoline ?? Monitors Blood loss Emergence and post op problems