Anxiety Disorders back to basics1
advertisement
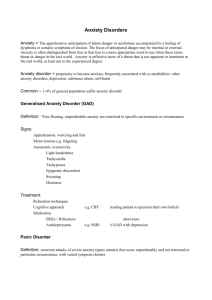
Anxiety Disorders Back to Basics 2012 Dr. Holly Dornan PGY-4 Psychiatry Resident University of Ottawa Anxiety LMCC Objectives Key Objectives In patients with many other medical complaints and/or excessive utilisation of medical health care, determine whether anxiety co-exists. Differentiate situational stress from true anxiety disorder and from drug and physical causes of anxiety. Objectives Through efficient, focused, data gathering: Review various physical symptoms briefly; elicit history of other nonpsychiatric illness, intake of alcohol and caffeine, and a brief history of any major life stresses. Elicit a history of excessive worry about events which is out of proportion to the impact of the event; history present for at least six months (anxiety). LMCC Objectives Determine whether there is restlessness, fatigue, inability to concentrate, irritability, muscle tension, sleep disturbance. Determine whether social, occupational, or function in general has been affected. Determine whether co-morbid psychiatric disorders exist, stress, substance abuse, past sexual, physical and emotional abuse, or neglect. Determine whether there is a discrete period of intense fear, recurrent panic attacks,>1 month of concern about more attacks, change in behavior in relation to attacks, along with cardiopulmonary, neurologic, psychiatric or other medical symptoms ± agoraphobia. LMCC Objectives List and interpret critical clinical and laboratory findings which were key in the processes of exclusion, differentiation, and diagnosis. Conduct an effective initial plan of management for a patient with anxiety or panic: Outline supportive therapy (e.g., psychosocial interventions) and counseling and list indications for drug therapy (e.g., selective serotonin re-uptake inhibitors). Select patients in need of specialized care. LMCC Objectives Applied Scientific Concepts 1. Explain that although the pathophysiology of panic disorder/attacks is incompletely understood, the amygdala, locus ceruleus, and hippocampus along with several neurotransmitters have been the focus of attention. LMCC Objectives Causal Conditions 1. Panic attack a. Cardiopulmonary symptoms - 40% b. Neurologic symptoms - 40% c. Gastrointestinal symptoms - 30% d. Psychiatric symptoms e. Autonomic symptoms 2. Panic disorder a. With agoraphobia/Without agoraphobia b. With social/Specific phobia c. Trauma/Stress related/Post traumatic stress disorder 3. Associated with other conditions a. Depression b. Obsessive compulsive disorder c. Substance abuse 4. Generalized anxiety disorder What is anxiety? A feeling state consisting of physical, emotional and behavioural responses to perceived threats1 Diffuse, unpleasant sense of apprehension accompanied by physical symptoms such as headache, sweating, palpitations, chest tightness, stomach upset, restlessness Normal and necessary part of everyday life 1 Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Anxiety vs. Fear Anxiety Fear Threat Threat Response to a threat that is unknown, internal, vague or conflictual Response to a known, external, definite threat Anxiety as a Disorder When does anxiety become a disorder? 1) Greater intensity and/or duration than expected given the circumstances 2) Leads to impairment or disability 3) Daily activities are disrupted by avoidance of certain situations or objects to decrease anxiety 4) Includes clinically significant unexplained physical symptoms, obsessions, compulsions, or intrusive recollections of trauma Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Anxiety Overestimated Anxiety = Likelihood x Harm Ability to cope Underestimated Beck et al. 1985 Pathophysiology of Anxiety Caudate nucleus has been implicated in OCD fMRI studies have found increased activity in the amygdala in PTSD Abnormalities in parahippocampal gyrus in Panic Disorder 3 major neurotransmitters involved are norepinephrine, serotonin, and GABA Kaplan and Sadock’s Synopsis of Psychiatry 10th edition * Slide courtesy of Dr. Elliott Lee Limbic cortex Nucleus accumbens Periaqueductal Gray matter Orbitofrontal cortex Amygdala Locus coeruleus Brain Stem Hippocampus Ventral Tegmental Area Anxiety Patients try to alleviate the unpleasant feeling of anxiety by: 1) Avoiding the trigger Developing a safety behaviour (i.e. having someone else accompany them) Using a substance or medication 2) 3) Anxiety Disorders in DSM-IV TR Panic Disorder with and without agoraphobia Agoraphobia without history of Panic Disorder Social Phobia Specific Phobia Obsessive Compulsive Disorder Generalized Anxiety Disorder Post Traumatic Stress Disorder Acute Stress Disorder Anxiety Disorder due to a General Medical Condition Substance-Induced Anxiety Disorder Anxiety Disorder NOS Epidemiology Lifetime prevalence for any anxiety disorder ranges from 10% to 29% 12 month prevalence 18% Common presentation in primary care 1:5 to 1:12 patients presenting to primary care will have an anxiety disorder Suicide rate 10 x higher than general population Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Initial Assessment of Patients with Anxiety Four scenarios: 1) Anxiety disorder is primary and there is no physical disorder present (any physical symptoms present are due to the anxiety) 2) The anxiety is secondary to a physical illness (e.g. hyperthyroidism) 3) The anxiety is secondary to a medication or substance 4) Both an anxiety and physical disorder are present by not causally related Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Medical conditions that mimic or worsen anxiety symptoms Endocrine conditions Cardiovascular Hyperthyroidism Hypothyroidism Pheochromocytoma Cushing’s disease Addison’s disease Menopause Acute Coronary Syndrome Arrhythmia CHF Hypertension Hypertension Mitral Valve Prolapse Medical conditions that mimic or worsen anxiety symptoms (con’t) Neurological Epilepsy Cerebrovascular disease Meniere’s disease Multiple Sclerosis Migraine Encephalitis Early dementia Metabolic Porphyria Diabetes Pulmonary Asthma COPD Pulmonary Embolism Pneumonia Medical conditions that mimic or worsen anxiety symptoms (con’t) Other Medications Anemia UTI (in elderly) Irritable Bowel Syndrome Heavy metal poisoning B12 deficiency Electrolyte disturbances Anti-cholinergics Steroids Stimulants (methylphenidate and amphetamine based) Theophylline Ventolin Nasal decongestants SSRIs Substance Abuse and Anxiety Substance abuse is often co-morbid with anxiety disorders as patients often try to self-medicate to cope with anxiety 37% of patients with GAD and 20-40% of patients with Panic Disorder have alcohol abuse/dependence Drug intoxication can mimic anxiety: - Amphetamines - Marijuana - Caffeine Nicotine Cocaine Phencyclidine - Hallucinogens - Ecstasy - Excessive alcohol consumption Substance Abuse and Anxiety (con’t) Drug withdrawal also associated with anxiety Alcohol Benzodiazepines Opiate Barbiturate Anti-hypertensives Key features Panic Disorder Fear of losing control, dying or going crazy • Avoid situations in which attacks may occur Agoraphobia • Fear of situations from which escape may be difficult or help unavailable (crowds, bus, bridge etc.) OCD • Intrusive, unwanted thoughts or urges (obsessions) and/or repetitive behaviours or mental acts (compulsions) • Fear of harm, uncertainty, uncontrollable actions • Key features Generalized • Anxiety regarding a number of everyday events Anxiety • Future and uncertainty difficult to accept Social • Fear of humiliation, embarrassment or Anxiety scrutiny by others PTSD Specific phobia Re-experiencing of trauma through flashbacks, dreams, recollections • Fear of a specific object, animal or situation • Generalized Anxiety Disorder – DSM IV TR Excessive anxiety and worry about a number of events or activities, occurring more days than not for at least 6 months Difficult to control the worry Associated with three of the following Restlessness, difficulty concentrating, muscle tension, fatigue, sleep disturbances, irritability Not due to a substance, medical condition or other mental disorder Causes clinically significant distress or impairment in functioning Generalized Anxiety Disorder 1Can Lifetime prevalence 6%1 68 % comorbidity with other psychiatric illness (depression, substance abuse, other anxiety disorder) Female to male ratio 2:11 25% of 1st degree relatives also have GAD2 Twin studies show concordance rate of 50%2 J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 2Kaplan and Sadock’s Synopsis of Psychiatry 10th edition Generalized Anxiety Disorder Chronic condition, usually lifelong Screening questions Do others call you a worry-wort? What kinds of things do you worry about? Usually seek treatment for somatic symptoms rather than anxiety Only 1/3 seek psychiatric treatment Often see specialists (GI, cardiology, internists) Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 GAD - treatment Pharmacotherapy: 1st line SSRI or SNRI 2nd line Benzodiazepine Only recommended for short term use due to side effects (cognitive impairment, ataxia, sedation) and dependence and withdrawal) Avoid in substance abuse and the elderly 3rd line Adjunctive olanzapine or risperidone Mirtazapine Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 GAD - treatment An optimal trial involves 8-12 weeks If there is not an adequate response, switch to another 1st line agent Reasonable to try another 1st line agent with a different mechanism of action Treatment resistant patients should be assessed for comorbid medical and psychiatric conditions Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 GAD - treatment Psychological treatment: CBT as effective as medication (also 1st line) CBT involves: Psychoeducation Cognitive interventions (addressing cognitive distortions, unrealistic beliefs) Exposure Relaxation strategies Problem Solving Assertiveness training Relapse Prevention Panic Attack – DSM-IV criteria A discrete period of intense fear or discomfort, in which 4 or more develop abruptly and reach a peak within ten minutes: Palpitations, increased heart rate Sweating Tremor or shaking Shortness of breath or smothering sensation Feeling of choking Chest pain Nausea or abdominal distress Feeling dizzy, lightheaded, or faint Derealization Depersonalization Parasthesias Chills or hot flushes Fear of losing control or going crazy Fear of dying Panic Disorder with or without agoraphobia – DSM-IV criteria The person has experienced both : Recurrent, unexpected panic attacks One or more of the attacks has been followed by either 1) Persistent concern about having another attack 2) Worry about the implications of the attack 3) Significant change in behaviour The presence (or absence of agoraphobia) Not due to a substance, medication or medical condition Not better accounted for by another mental disorder Panic Disorder Lifetime prevalence of Panic Disorder is 4.7% Lifetime prevalence of having a panic attack is 15% 1/3 to 1/2 of patients also have agoraphobia More common in women than in men Generally begins in late adolescence or early adulthood Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Panic Disorder 20 X the risk of suicidal ideation and suicide attempts as the general population Felt to be related to dysregulation of brain noradrenergic systems Abnormalities have been found in the autonomic nervous system of some patients (increased sympathetic tone, less adaptive to repeated stimulit) Kaplan and Sadock’s Synopsis of Psychiatry 10th edition Panic Disorder Initially, panic attacks are unexpected Can occur any time (even night) Can also develop panic attacks that have triggers (situationally-predisposed panic attacks) Patients begin to have anticipatory anxiety about having another panic attack This can lead to avoidance of situations where escape or help may not be readily available (agoraphobia) Panic Disorder - Treatment Pharmacotherapy: 1st line SSRI or SNRI 2nd line Benzodiazepines Only recommended for short term use due to side effects (cognitive impairment, ataxia, sedation) and dependence and withdrawal Avoid in substance abuse and the elderly ** Often clinically, a small dose of long acting benzodiazepine is started along with SSRI/SNRI to provide more immediate relief from distressing symptoms i.e. 0.5 mg clonazepam BID for 2-3 weeks, then tapered until it is stopped Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Panic Disorder - Treatment Psychological treatment: CBT most consistently efficacious psychotherapy for Panic Disorder, according to the literature Individual or group therapy, bibliotherapy CBT for Panic Disorder includes same CBT concepts of psychoeducation, cognitive approaches, relaxation, problem solving Also incorporates interoceptive exposure (exposure to feared symptoms therapist may ask patient to hyperventilate or spin to make themselves dizzy) Exposure to avoided situations is important Obsessive Compulsive Disorder – DSM IV criteria Either obsessions or compulsions Obsessions are defined as: Recurrent and persistent thoughts, images or impulses that are experienced as intrusive and inappropriate and cause marked anxiety/distress Not simply excessive worries about real-life problems Person attempts to ignore or suppress the obsessions, or neutralize them with other thoughts or actions Recognized as a product of the patient’s own mind Compulsions are defined as: Repetitive behaviours or mental acts that the person feels driven to perform in response to an obsession, or according to rigid rules Compulsions are aimed at reducing distress or preventing some dreaded event, however they are not connected in a realistic way to what they are meant to neutralize, or are clearly excessive Obsessive Compulsive Disorder – DSM IV criteria (con’t) At some point during the course of the disorder, the person recognizes that the obsessions and/or compulsions are excessive or unreasonable The obsessions and/or compulsions cause marked distress, are time consuming (> 1 h/day), or significantly interfere with functioning Not due to substance, or another medical or mental disorder Obsessive-Compulsive Disorder Estimated lifetime prevalence of 1.6% Median age of onset 19 years (range 14 – 30 years) 60% are female High psychiatric co-morbidity rate (56% -83%) Common co-morbidities include substance abuse, depression, social phobia, generalized anxiety disorder, panic disorder Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Obsessive-Compulsive Disorder In 50-70% of patients, onset of symptoms is following a stressful event (i.e. pregnancy, death) Course is usually long, can be constant or fluctuating 20-30 % have significant improvement 40-50% have moderate improvement 20-30% have no improvement or worsening Kaplan and Sadock’s Synopsis of Psychiatry 10th edition Obsessive-Compulsive Disorder 20-30% have tics, 6-7% Tourette’s Possible link between a subset of OCD and tics PET studies have shown increased activity in the frontal lobes, basal ganglia (caudate), and cingulum in patients with OCD PANDAS – Pediatric Autoimmune Neuropsychiatric Disorders associated with Streptococcal infections Streptococcus infection may trigger an autoimmune response which causes acute onset OCD symptoms and tics in children Kaplan and Sadock’s Synopsis of Psychiatry 10th edition Obsessive-Compulsive Disorder Most common obsessions include: Contamination (#1) Doubt/safety (idea that stove was left on, door unlocked etc.) (#2) Sexual and aggressive impulses (#3) Symmetry and exactness (#4) Somatic and religious preoccupations Most common compulsions include: Checking Washing Repeating Ordering Counting Hoarding OCD - treatment Pharmacotherapy: 1st line SSRI (serotonergic response needed) 2nd line : Clomipramine (2nd line due to side effects – cardiotoxicity, anticholinergic, drug interactions and lethality in overdose) Effexor XR, Mirtazapine Adjunctive Risperidone Dosages of meds e.g. SSRIs may need to be higher than in mood disorders Response may take 6 wks or longer (Guidelines state adequate trial 6-8 weeks) Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 OCD - treatment Psychological 1) Exposure with Response Prevention (ERP) – form of behavioural therapy 2) CBT which combines Exposure and Response Prevention with cognitive interventions Posttraumatic Stress Disorder DSMIV criteria The person has been exposed to a traumatic event which included both: 1) The person experienced or witnessed an event involving actual or threatened death or serious injury, or a threat to personal integrity of self or others 2) Response was fear, horror, or helplessness The traumatic event is re-experienced including at least one of: Distressing memories, dreams, acting or feeling as if event is recurring (illusions, dissociative flashbacks, hallucinations), intense psychological or physiological distress when exposed to cues that symbolize the trauma Posttraumatic Stress Disorder DSMIV criteria Persistent avoiding of stimuli associated with the trauma and numbing of responsiveness including at least 3 of: Efforts to avoid thoughts, feelings, conversations associated with the trauma Efforts to avoid people, places and activities associated with the trauma Inability to recall an important aspect of the trauma Feeling of detachment or estrangement from others Restricted range of affect Sense of foreshortened future Posttraumatic Stress Disorder DSMIV criteria Persistent symptoms of increased arousal including at least two of: Difficulty falling or staying asleep Irritability or outbursts of anger Difficulty concentrating Hypervigilance Exaggerated startle reflex Duration is more than 1 month Causes clinically significant distress or impairment in functioning Posttraumatic Stress Disorder Key features include exposure to trauma, reexperiencing of the trauma, avoidance and emotional numbing, and hyperarousal Examples of traumas include exposure to war, terrorist attacks, natural disasters, accidents involving serious injury or death, rape, torture If symptoms are present for less than one month, then the diagnosis may be Acute Stress Disorder Posttraumatic Stress Disorder Prevalence in Canada 2.4% (1 month prevalence) and 9.2% (lifetime prevalence) Higher among women than men Lifetime prevalence estimates 16-37% in areas of the world where conflict has occurred Frequent co-morbidity with depression, substance abuse, other anxiety disorders Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Posttraumatic Stress Disorder 6X increased risk of suicide attempts Predisposing factors include: Childhood trauma Inadequate support system Female Genetic vulnerability to psychiatric illness Excessive alcohol use (recent) Posttraumatic Stress Disorder Treatment 1Can Guidelines recommend SSRI/SNRI as first line treatment1 Recommended that patients with PTSD should continue medication for at least 1 year1 In practice, agents to help with insomnia are often added (i.e. Trazadone) J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Posttraumatic Stress Disorder Treatment Other meds sometimes used include: Clonidine (antiadrenergic agent) Prazosin for nightmares (alpha-1 adrenergic antagonist) Psychological treatment: CBT recommended Social Anxiety Disorder (Social phobia) – DSM IV criteria Marked and persistent fear of social or performance situations in which the person is exposed to unfamiliar people or possible scrutiny by others Fear that they will embarrass or humiliate themselves Exposure to the feared situation invariable produces anxiety which may be in the form of a panic attack The person recognizes that the fear is excessive or unreasonable Social Anxiety Disorder (Social phobia) – DSM IV criteria (con’t) The feared situations are avoided or endured with intense anxiety and distress The avoidance, anxious anticipation or distress interferes with functioning or causes marked distress In individuals under 18, duration is at least 6 months Not due to substance, medical condition or other mental disorder If a medical condition is present, the fear is not related to it (i.e. trembling in Parkinson’s) Social Phobia Most people in the general population experience a degree of discomfort with certain social situations Generalized type vs. non-generalized (a restricted number of situations i.e. public speaking) Differentiate from panic disorder (panic attacks in social phobia always occur in feared situations) Differentiate from normal shyness (shyness should not cause functional impairment or marked distress) Social Phobia Has significant impact on quality of life Lifetime prevalence of 8-12% 1 (one of the most common anxiety disorders) r Early onset, usually in childhood Chronic course, usually 20 years or longer Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Social Phobia Interferes with career, relationship, goals “illness of missed opportunities” Comorbid conditions include substance abuse, depression, or another anxiety disorder Key symptoms include blushing, sweating, palpitations, tremor and lightheadedness, panic attacks Situations are often avoided as an effort to alleviate distress Social Phobia - treatment Pharmacotherapy: 1st line SSRI or SNRI 2nd line Benzodiazepine Only recommended for short term use due to side effects (cognitive impairment, ataxia, sedation) and dependence and withdrawal Avoid in people with substance abuse and the elderly 3rd line Adjunctive Abilify or Risperidone Mirtazapine, wellbutrin ** Although not in guidelines, in practice, beta blockers have been used with effect for non-generalized type performance anxiety Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Social Phobia - treatment Psychological treatment CBT (group or individual) CBT for social phobia includes exposure to feared situations and social skills training Similar efficacy to pharmacotherapy In practice, CBT and medications are often combined After discontinuation of CBT or medications, gains with CBT last longer Specific Phobia – DSM IV criteria Excessive or unreasonable fear cued by the presence or anticipation of a specific object or situation (insects, flying, heights, blood) Exposure provokes an immediate anxiety response Fear is recognized as excessive or unreasonable Situation is avoided or endured with intense distress Marked distress or interferes with functioning Not due to a substance, medical condition or other mental disorder Specific Phobia Lifetime prevalence of 12% Most common mental disorder Begins at young age, 5-12 years old Treatment is exposure based therapy Graded exposure helpful Virtual reality or computer programs sometimes used for fear of heights, flying, dentist Can J Psychiatry Clinical Practice Guidelines for the Management of Anxiety Disorders July 2006 Questions