Mixed, Central, and Functional Hearing Loss
advertisement

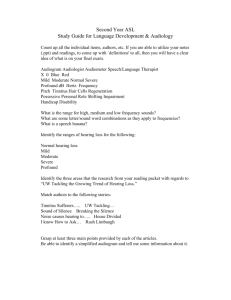
1 Mixed, Central, and Functional Hearing Loss & Tinnitus DR.S.H.HASHEMI 2 MIXED HEARING LOSS 3 MIXED HEARING LOSS Whenever the hearing loss of a patient includes a mixture of both conductive and sensorineural characteristics, is said to have a mixed hearing loss. Hearing deficiency may have started originally as a conductive failure (otosclerosis) and later developed a superimposed sensorineural component. The difficulty may have been sensorineural in the beginning ( presbycusis ), and a conductive defect (middle-ear infection ) may have developed subsequently. In some cases the conductive and the sensorineural elements may have started simultaneously ( severe head injury affecting both the inner ear and the middle ear ). 4 MIXED HEARING LOSS . . . In clinical practice, most cases with an original sensorineural etiology remain in that classification without an added conductive element. In contrast, most cases that start as conductive hearing impairment later develop some sensorineural involvement. Otosclerosis . . . + . . . presbycusis Chronic otitis media . . . + . . . Labyrinthitis Otosclerosis was at one time thought to retain its purely conductive character for years; today it is recognized that this condition develops sensorineural impairment in same cases. 5 * * * * History: A 67-year-old man with insidious deafness for 25 years No tinnitus or vertigo Otologic: Normal Audiologic: Reduced air and bone conduction thresholds with some air-bone gap in the right ear * Classification: Mixed hearing loss 6 * Diagnosis: Otosclerosis with secondary sensorineural involvement * * * * History: A 62-year-old woman with severe deafness Voice is normal. No tinnitus or vertigo Otologic: Normal Audiologic: Bone conduction is better than air, but patient denied hearing the tuning fork on the mastoid or the forehead but heard it fairly well on the teeth * Classification: Mixed hearing loss. * Diagnosis: Otosclerosis with sensorineural hearing loss * Comment: Both oval windows were overgrown with otosclerosis which required drilling 7 MIXED HEARING LOSS . . . Mixed hearing loss is becoming more common also in otosclerosis after stapedectomy . The sensorineural deficit may be caused by penetration of the oval window with exposure of the perilymph. Despite meticulous surgical care, the inner ear also can be traumatized readily and made more susceptible to infection . In surgical trauma to the inner ear, high-frequency hearing loss often falls below the preoperative level, and the patient may complain of reduced discrimination though his pure-tone threshold is improved. 8 * * * * * * History: A 60-year-old man with bilateral chronic otorrhea for 40 years Insidious hearing loss for many years . No tinnitus or vertigo Otologic: Putrid discharge with evidence of cholesteatoma Audiologic: Moderate to severe bilateral flat loss Classification: Mixed hearing loss Diagnosis: Chronic otitis media with neural or cochlear involvement 9 MIXED HEARING LOSS . . . In chronic otitis media some toxic inflammatory metabolite produces a cochleitis or labyrinthitis. 10 * * * * * * History: A 45-year-old man with fullness in both ears and hearing loss for one week No tinnitus or vertigo . No history of ear infections Otologic: Bilateral impacted cerumen. Removed, and eardrums normal Audiologic: Bilateral reduced air conduction thresholds with greater loss in high frequencies Classification: Mixed hearing loss before removal of cerumen. Sensorineural loss after removal of cerumen Diagnosis: Impacted cerumen with progressive nerve deafness 11 MIXED HEARING LOSS . . . This example a warning to physicians to avoid assuring any patient that his hearing loss can be corrected merely by removing cerumen, because mixed hearing loss may be found subsequently. 12 MIXED HEARING LOSS . . . In every case of mixed hearing loss one should determine how much of the deficit is conductive and how much is sensorineural. The prognosis depends largely on this estimate . The best way to approximate the conductive and the sensorineural components of a hearing loss is to perform all possible tests for estimating the patient’s sensorineural potential or “cochlear reserve.” In addition to routine bone conduction, speech discrimination scores are essential . If the patient hears and discriminates well when speech is made louder, then the conductive element probably is a major cause of the hearing difficulty, and there is a good chance that surgery will improve 13 the hearing. MIXED HEARING LOSS . . . If the patient does not understand any better with a hearing aid or when the voice is raised, hearing is not improved even if the conductive portion of the mixed hearing loss is corrected. Prognosis: In mixed hearing loss the prognosis depends on the relative proportion of conductive and sensorineural pathology. If the sensorineural component is slight, the surgical prognosis is good , and under favorable circumstances the hearing may approximate the level of the bone conduction. However, the discrimination is not improved much, even after correction of the conductive defect. 14 CENTRAL HEARING LOSS 15 CENTRAL HEARING LOSS If it is caused by a lesion that affects primarily the central nervous system from the auditory nuclei to the cortex.(auditory pathway) 16 CENTRAL HEARING LOSS . . . The auditory pathway consists of a series of transducers that repeatedly change the speech stimulus so that it can be handled effectively by the cortex. The eardrum and the ossicular chain modify the amplitude of the sound waves . The cochlea analyzes these waves and reflects them as impulses to the cortex. The chief function of the auditory cortex is to interpret and to integrate these impulses and to provide the listener with the exact meaningful information intended by the speaker, or to permit the listener to react appropriately to the actual 17 implication of the sound. CENTRAL HEARING LOSS . . . In unilateral central hearing loss the contralateral ear can be affected. In unilateral central hearing loss (e.g. brain tumor) the opposite ear, which presumably hears normally may have much poorer discrimination than the ear of a person who has normal hearing. A similar adverse effect is noted in the ear opposite the tumor when certain words are interrupted periodically or accelerated. The patient with central hearing impairment has no difficulty perceiving highfrequency sounds such as the letter s and f that are affected so characteristically in peripheral sensorineural lesions, but he/she has difficulty interpreting what is heard. 18 CENTRAL HEARING LOSS . . . Characteristic Features of central hearing loss : Hearing tests do not indicate peripheral hearing impairment. pure-tone threshold is relatively good compared with the ability of the patient to discriminate, and especially to interpret, what he/she hears. The patient has difficulty interpreting complex information. 19 CENTRAL HEARING LOSS . . . The prognosis for central hearing impairment is poor . There is no characteristic audiometric pattern, except that the disparity between the hearing level and the speech interpretation is quite marked. In certain cases, central hearing loss may mimic peripheral causes of deafness, including occupational deafness. The spheroid cells of the superior ventral cochlear nucleus (SVCN) show an anatomical frequency gradient, low ventral to high dorsal. 20 Superior ventral cochlear nucleus (SVCN) Erythroblastosis typically causes hearing loss that centers around 3000–4000 Hz. This may be caused by injury to SVCN spheroid cells, the second-order neurons of the ascending auditory pathway , even in the presence of normal hair cells in the organ of Corti . Central pathology must be included in the differential diagnosis of the hearing loss producing a 4000-cycle dip on the audiogram. 21 Central Auditory Processing Disorders (CAPD) CAPD characterized by decreased understanding of speech in the presence of background noise . Common complaints include inability to study or read in the presence of noise, slowing of reading speed caused by noise(vacuum cleaners or air conditioners ) and suspicion by family members that the patient has a hearing loss. If people talk to a person with CAPD while he or she is involved in auditory concentration such as listening to a television program, the person will often “not hear.” However, if one gets the persons attention by calling his or her name before speaking, the first sentence will not be missed, and hearing is normal. Treatment : altering the listening environment to obtain the best possible signal-to-noise ratio . 22 FUNCTIONAL HEARING LOSS 23 FUNCTIONAL HEARING LOSS Functional or psychogenic hearing loss is the customary diagnosis when there is no organic basis for the patient’s apparent deafness. The inability to hear results entirely or mainly from psychological or emotional factors, and the peripheral hearing mechanism may be essentially normal. The basis for functional hearing loss in most patients is psychogenic, the product of emotional conflict, ( neurotic anxiety ) . Tinnitus is a characteristic feature of “hysterical deafness,” and patients often claim that the noise is unbearable. Hearing acuity usually varies, depending on the patient’s emotional state at the time of testing. 24 FUNCTIONAL HEARING LOSS . . . Functional hearing loss is an unconscious device by which the patient seeks to escape from an intolerable problem that he/she cannot face consciously. Hysterical blindness and paralysis are other examples of the same type of somatization or “conversion reaction.” Military life during wartime Civilian life 25 Functional Overlay It is entirely possible for hearing loss of functional origin to be superimposed on true organic hearing impairment . The problem then is to recognize the two components in the patient’s hearing impairment. The history and the otologic examination important clues . often provide (e.g. the patient may claim that his/her hearing was excellent until a physician cleaned out his/her ears with such force that he/she suddenly went stone deaf.) 26 History: A 34-year-old woman with otosclerosis and hearing loss for over 10 years Refuse to use hearing aids She often says, “What?” even when addressed loudly. repeats a question before answering She appears to be frustrated and emotionally disturbed and does not use her residual hearing effectively Diagnosis: functional overlay on an organic otosclerosis 27 After positive suggestion this patient acquired a hearing aid and is doing much better FUNCTIONAL HEARING LOSS . . . Diagnosis by Specific Features: In an organic lesion, all tests must: Consistent results when they are repeated Correlate with one another A medical history could not possibly explain the patient’s condition (e.g. Sudden onset of profound deafness following instillation of drops into the ears ). Too spectacular an improvement with a hearing aid, especially when the patient has set the controls at minimal amplification, or a sudden disproportionate improvement in hearing after a simple procedure such as drum massage or insufflating the eustachian tube. 28 FUNCTIONAL HEARING LOSS . . . Diagnosis by Specific Features : . . . Decided fluctuations in hearing acuity as determined by any single test. Inconsistency in the results of two or more tests. In complete deafness the presence of cochlear nerve reflexes with loud noises indicates either malingering or hysteria. Psychogalvanic skin resistance test Impedance audiometry Otoacoustic emissions test Evoked-response audiometry 29 FUNCTIONAL HEARING LOSS . . . Psychogenically induced hearing loss usually is a uniform flattone loss in all frequencies, suggestive of a well-marked conductive impairment. In a patient with unilateral functional deafness there may be complete absence of bone conduction on the side of the bad ear, though the good ear has normal acuity. Such a patient even may deny hearing shouts directed at the bad ear in spite of the good hearing in the opposite ear. 30 Audiometric Patterns in Functional Hearing Loss There is no characteristic audiometric pattern in functional hearing loss , but the consistent inconsistencies serve to alert the physician. Usually, the hearing impairment is bilateral, and the bone conduction level is the same as the air conduction level. 31 History: A 21-year-old woman with a series of emotional conflicts : breakup with her fiance , flunking out of college, and pending divorce of her parents. Otologic: Normal. Audiologic: PTA: showed a severe hearing loss, she often seemed able to hear soft voices behind her back. PGSR :showed normal hearing. Classification: Functional 32 Etiology: Emotional disturbance. Her hearing returned to normal after psychotherapy. Malingering Malingering is the deliberate fabrication of symptoms that the patient knows do not exist. The patient is motivated by the desire to seek some advantage: Financial compensation Escape from military service Evasion of responsibility for failure Characteristically, the malingerer abandons the symptoms when he/she thinks he/she is no longer being observed. If the patient claims he has one “good” and one “bad” ear, and the examiner obstructs his “good ear” with a finger, then shouts into it loudly enough to be heard easily by bone conduction alone, the malingerer claims he hears nothing. 33 History: A 37-year-old construction worker knocked to ground by a beam No unconsciousness, but left ear required sutures Otologic: Normal. Normal caloric findings. Audiologic: varying and inconsistent hearing levels during repeated audiograms Classification: Functional hearing loss 34 Etiology: Malingering Tinnitus 35 Tinnitus is a term used to describe perceived sounds that originate within the person rather than in the outside world. Although nearly everyone experiences mild tinnitus momentarily and intermittently, continuous tinnitus is abnormal, but not unusual . The prevalence of tinnitus increases with age up until 70 years and declines thereafter . This symptom is more common in people with otologic problems, although tinnitus also can occur in patients with normal hearing. 36 DDx: Rushing of blood through the cranial arteries (certain changes in the vascular walls : atherosclerosis ) Pressing on various blood vessels in the neck occasionally stops this type of tinnitus . Noises made by muscles in the head during chewing Changes in temporal bone structure 37 Tinnitus also may serve as an early sign of auditory injury.(high-pitched ringing or hissing may be the first indication of impending cochlear damage from ototoxic drugs). Aspirin , Quinine( large dose ) Diuretics Aminoglycoside antibiotics Chemotherapy drugs These drugs should be used with extreme caution, especially when kidney function is deficient. 38 Tinnitus: Subjective (audible only to the patient) More common Unfortunately, it cannot be confirmed with current methods of tinnitus detection. Usually difficult to document its presence and quantify its severity . Objective (audible to the examiner ) comparatively easy to detect and localize because it can be heard by the examiner using a stethoscope or other listening device. Glomus tumors, AV-malformations, Palatal myoclonus 39 DESCRIPTION OF TINNITUS: Ringing of bells Roar of the ocean Running motor Buzzing Machine shop noises Hissing of steam Localization: In the ears In the center head Not in the ears at all but inside the head Patients sometimes say that the ear noises are so loud that they are unable to hear what is going on around them. Tinnitus rarely is louder than a very soft whisper (5–10 dB above hearing threshold) . 40 Although the character of tinnitus is rarely diagnostic, certain qualities are suggestive of specific problems : Seashell-like tinnitus(ocean-roaring type): Meniere’s syndrome (endolymphatic hydrops & swelling of the inner ear membranes & ear fullness & fluctuating hearing loss unassociated with straining or forceful nose blowing ) Syphilitic labyrinthitis Trauma Unilateral ringing tinnitus: Acoustic neuroma Trauma Perilymph fistula (ringing tinnitus & fluctuating ear fullness & hearing loss during straining ) 41 Pulsatile tinnitus: A-V malformations Glomus jugulare tumors low-pitched type: Otosclerosis Other forms of conductive hearing loss Ringing & Hissing: Sensorineural hearing loss 42 When evaluating the history of a tinnitus (ear noise) problem, the following questions should be asked: 43 44 45 46 PHYSICAL EXAMINATION AND TESTING History physical examination: Complete head and neck assessments Examination of the cranial nerves Audiogram Routine audiogram Assessment of hearing at frequencies not tested routinely Brainstem evoked-response audiogram (BERA) Balance tests: Electronystagmogram (ENG) Computerized dynamic posturography (CDP) Otoacoustic emission (OAE) testing 47 PHYSICAL EXAMINATION AND TESTING . . . Imaging studies: MRI CT Single photon emission computed tomography (SPECT) Positron emission tomography (PET) Blood tests: Diabetes Hypoglycemia Hyperlipoproteinemia Lyme disease Syphilitic labyrinthitis Thyroid dysfunction Collagen vascular disease Autoimmune inner-ear disease 48 AUDIOMETRY IN THE PRESENCE OF TINNITUS May be the patient complains of inability to detect the tone produced by the audiometer because of the tinnitus. It is best to present quickly interrupted or warbled tones so that the patient can distinguish the discontinuous audiometer tone from the constant tinnitus. 49 TINNITUS WITH A NORMAL AUDIOGRAM Perform an audiogram on every patient who complains of tinnitus. If the otoscopic findings are normal, and the audiogram shows normal hearing from the lowest frequencies to 8000 Hz, and yet the patient complains of tinnitus, several causes should be considered : (1) Hearing defects > 8000 Hz or at “in-between” frequencies not tested during routine audiogram (2) Vascular and neurologic disorders (3) Functional causes (4) Retrocochlear disease such as an acoustic neuroma (5) Temporomandibular joint (TMJ) abnormality 50 TINNITUS WITH HIDDEN HIGH-FREQUENCY HEARING LOSSES Many patients who complain of ringing or hissing tinnitus may have perfectly normal hearing in the routine frequencies (250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz). when the hearing is tested at higher frequencies up to 20,000 Hz, it is not uncommon to find a hearing deficit. The hearing damage may well be at a point intermediate between these routinely tested frequencies ( 40 dB loss at 3500 Hz ) 51 *History: a 38-year-old woman with fullness in her right ear and high-pitched constant tinnitus for several months. *Otologic: Normal *Audiologic: Normal hearing with high-tone hearing loss > 8000 Hz *Classification: High-tone sensory hearing loss *Diagnosis: After further questioning the patient subsequently associated the onset of tinnitus with a bad cold *Hearing loss and subsequent tinnitus probably due to a viral cochleitis 52 TINNITUS AND OTOSCLEROSIS Low-pitched Buzzing , roaring sound or pulsing noise timed to heartbeat In some patients with otosclerosis, the tinnitus is even more disturbing than the hearing loss. Not all patients with otosclerosis have tinnitus In most instances, tinnitus will disappear or diminish during the course of many years of hearing impairment. The fixation of the stapedial footplate may be eliminate the tinnitus or may not . 53 TINNITUS IN MENIERE’S DISEASE Ocean roar or a hollow seashell sound In the early stages of Meniere’s disease, tinnitus often persists all the time and becomes the most disturbing symptom of the disease. Many patients would even sacrifice their hearing to get rid of the tinnitus. 54 TINNITUS AFTER HEAD TRAUMA, EXPOSURE TO NOISE Ringing tinnitus After a blow to the external ear Close exposure to a sudden very loud noise ( explosion of a firecracker or the firing of a gun ). Tinnitus is accompanied by a high-frequency hearing loss: If the hearing loss is temporary, the tinnitus usually subsides in a few hours or days. If the hearing loss is permanent , the ringing tinnitus may persist for many years or permanently. 55 ACOUSTIC NEURITIS Acoustic nerve inflammation High-tone deafness High-pitched tinnitus Hepatitis , influenza, other viral diseases Infection of the middle ear. 56 ACOUSTIC NEUROMA Benign tumor of the cerebellopontine angle Unilateral tinnitus ( often is the first symptom ) Tinnitus may be caused by: Other Cerebellopontine angle neoplasms( meningioma, cholesteatoma, vascular malformation) Anterior–inferior cerebellar artery(loop of blood vessel ) Brainstem tumors MRI should be considered especially in any patient with unilateral tinnitus. 57 TM JOINT PROBLEMS Malocclusion or other TMJ disparity Tinnitus has resolved with adequate TMJ treatment Placing a plastic prosthesis (bite block) over the lower molars at night 58 FUNCTIONAL CAUSES Diagnosis of functional or psychological tinnitus should be made with great caution. Malingering:when the patient does not perceive an abnormal noise and is aware of the fact, usually for secondary gain(lawsuit). True functional or “hysterical” tinnitus is psychiatric in etiology and disappears following effective psychotherapy. 59 MANAGING THE PATIENT WITH TINNITUS Tinnitus is usually not curable Unless a correctable, structural, or metabolic cause is found. In managing the patient with tinnitus, it is advisable to have a forthright talk with the patient and to explain the most likely cause of the tinnitus and the fact that as yet there is no specific cure for it. Tinnitus maskers a re recommended by some physicians but their value is also limited. Temporary method for relief from tinnitus They introduce a noise into the ear that the patient is able to control. Hearing aid-like instrument that produces a narrow band noise centered around the pitch of the patient’s tinnitus. The level of masking noise is above the patient’s tinnitus. 60 MANAGING THE PATIENT WITH TINNITUS . . . Habituators is a device somewhat similar to a tinnitus masker. Primarily used to treat patients with hyperacusis (hypersensitivity to noise) External masking with a radio, fan, music, vaporizer is helpful, especially at night if the tinnitus interferes with their ability to fall asleep. Tranquilizers : otosclerosis and Meniere’s disease Medical attention to related vascular abnormalities: Hypertension Buerger’s disease Atherosclerosis 61 MANAGING THE PATIENT WITH TINNITUS . . . Hypnosis Psychotherapy SURGERY: Eighth nerve section Vascular loop (malpositioned blood vessel) compressing the eighth nerve, microvascular decompression can be performed through the posterior fossa. THE END 62 63