RTOG 0813
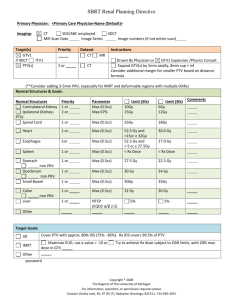
advertisement

RTOG 0813 Seamless Phase I/II Study of Stereotactic Lung Radiotherapy (SBRT) For Early Stage, Centrally Located, Non-Small Cell Lung Cancer (NSCLC) In Medically Inoperable Patients Seth R. Duffy, BSPH Image Source: http://www.ikwilstoppenmetroken.nu/aantal-doden-longkanker-omlaag-door-screening/ Radiation Therapy Oncology Group (RTOG) RTOG 0813 saw its inception and activation in February of 2009 Served as one of the forerunners in the emergence of SBRT treatment techniques SBRT is unique in that it delivers hypofractionated treatments of high-doses Clinical locations (209) approved through a rigorous approval process by the RTOG headquarters Epidemiology: Lung Cancer The Leading Cause of Cancer-Related Deaths in the United States and Globally. Most Common Cancer World-Wide Since 1985. (Incidence and Mortality) 5-Year Survival Rate of 15.6%. Median Age of Diagnosis is 71 Years of Age. Adenocarcinoma has replaced squamous cell as the most prevalent type of NSCLC (2013). Citation [5] Inclusion Criteria for Potential Participants Eligible (Accepted) Pathologically Proven Diagnosis of NSCLC Staging of T1-2, N0, M0 Non-Small Cell Lung Cancer Tumor Size ≤ 5cm Not A Candidate for Surgical Resection Deemed Medically Inoperable By An Experienced Thoracic Surgeon Exclusion (Denied) Measurable Disease Patient Provision of Informed Consent At Least 9 Forms of Consent Also Continued Consent Throughout The Trial Zubrod Performance Status Outside 0-2 Range 4 Weeks Prior to Registration Excess Pleural Effusion Pregnant or Positive Serum Tumor Within The Zone of The Proximal Bronchial Tree Not 18 Years Of Age Prior Invasive Malignancy Within The Past 2 Years Within 72 Hours of Registration Other Than Melanomatous Skin Cancer Previously Irradiated Region of Study (Causing Overlap) Excessive Comorbidities No Concurrent therapy Including Standard Fractionated RT or Surgery or Systemic Chemotherapy Protocol Objectives In RTOG 0813 What does this clinical trial hope to accomplish? Phase I Portion: Phase II Portion: Secondary Objectives: Tertiary Objectives: To determine the maximal tolerated dose (MTD) of SBRT for centrallylocated NSCLC and the efficacy of that dose in patients who are not operative candidates. (8/20/10) To estimate the primary tumor control rate at the MTD of SBRT. To estimate rates of ≥ grade 3 CTCAE, v. 4 adverse events other than a dose-limiting toxicity (DLT) which is possibly, probably, or definitely related to treatment and which occurs within 1 year from the start of SBRT. To estimate rates of late adverse events (> 1 year from starting SBRT) To estimate primary tumor control and progression-free and overall survival rates for patients treated with this regimen. See Reference Section 2.0 in RTOG 0813 Protocol Section 6.1 Stereotactic Dose Fractionation Patients are to be treated with 5 fractions of radiation, on an every other day basis (2-3 treatments per week with a minimum of 40 hours between treatments). The [red box] indicates the protocol starting dose, “Level 5”, from which dose escalation in future patients (or dose-limiting) will occur. Pre-Treatment Planning Preparation Protocol Section 6.2-6.3 Technical Factors -Only X-ray photon beams of energies 4-10 MV -Minimum field dimensions of 3.5 cm is required to account for uncertainties in beam commissioning -Heterogeneity corrections must be utilized when planning with IMRT -Reliable abdominal compression, accelerator beam gating, tumor tracking, and active breath-holding techniques may all be utilized once approved by the PI and Study Co-Chairs Simulation Localization -Achieving the most comfortable, stable patient positioning possible is important -Isocenter, or reference point, port localization images must be taken at each treatment on the specific linac to deliver treatment -Stereotactic body frames, with large rigid pillows, may be used ~AP and Lateral -GTV volume must not deviate beyond the confines of the PTV as defined by the physician -Verification CT scans and portal films may be taken at the discretion of the institution / physician -CT simulation should be the primary imaging modality and should be performed with IV contrast -The 3-D fixed coordinate system should be defined by reliable fiducial markers. -≤ 3.00 mm scan slice thickness -Helical and 4DCT are both acceptable imaging methods ~Radiopaque markers, rods, or even metallic seeds placed within the tumor itself Dosimetry & Treatment Planning Protocol Section 6.4-6.5 Critical Structures Esophagus Spinal Cord The esophagus is a hollow transporting structure that assists in the digestion of solids and liquids. Measures 25-30cm in length. This structure is contoured to include the fatty surrounding tissues as well. Spanning between the foramen magnum to the L1-L2 interspace, the spinal cord is one of the most essential structures within the human body. This protocol outlines that this structure be contoured to the bony limits of the spinal canal. Great Vessels Heart / Pericardium Five great vessels enter and leave the heart: the superior and inferior vena cava, the pulmonary artery, the pulmonary vein and the aorta. The primary function of which are to circulate blood (oxygenated and deoxygenated). The human heart is comprised of four chambers: the right atrium and ventricle and the left atrium and ventricle. The pericardium is a fluid filled sac that Surrounds the heart and the proximal ends of the aorta, vena cava, and pulmonary artery. 2cm Margin The Proximal Bronchial Tree Defined as: The distal trachea (2cm following the proximal trachea), the carina, and the two major mainstem bronchi, portions of the upper lobe bronchi, the intermedius bronchus, the right middle lobe bronchus, the linguar bronchus, and the right and left lower lobe bronchus. Although this structure is not extensively evaluated upon dose received, it plays an important role in delineation of who is eligible for this protocol versus who is not eligible. Critical Structures Skin While often overlooked, the skin is essential to the human body because it not only protects the underlying tissues and organs but also assists in the body’s regulation of temperature as well as giving sensations of touch, hot, and cold. Non-Adjacent Wall The Non-Adjacent Wall structure is something specific to this protocol that accounts for dose-spillage past the midline of the body and into the half where the disease does not exist. Trachea Whole Lung Approximately 11.5cm in length and 2.5 cm in diameter. The trachea provides a path for respiration to occur. This function is further assisted (and strengthened) by tracheal cartilages. The whole lung encompasses both right and left lungs, per protocol request. This also includes collapsed lungs. All GTV must be removed from this structure’s contour. The Lungs are essential to respiration and must be correctly contoured and monitored. Image From: http://www.nlm.nih.gov/medlineplus/ency/imagepages/9129.htm The Brachial Plexus The brachial plexus has been described as: A beautiful, intricate, and complex structure that comprises the connections of the spinal nerves to their terminal branches in the upper extremity.”[8] Clinically divided into five unique zones but not within this protocol Emerges from the posterior triangle of the neck, bordering the sternocleidomastoid Delineation of Target Volumes RTOG 0831 Section 6.4 and ICRU-62 GTV CTV Gross Tumor Volume Defined As: The Visible, Palpable, Known Disease Region as Determined by an Experienced Oncologist. Contoured As: Gross Disease Clinical Target Volume Planning Target Volume Defined As: A Tissue Volume of the GTV and any Suspected Microscopic Disease Defined As: The Geometrical Concept that Encompasses the Previous Structures with Treatment Planning in Mind. Contoured As: GTV+Microscopic Contoured As: GTV (or ITV) + 0.5cm in the axial plane & 1.0cm in the longitudinal plane ITV Internal Target Volume ITV PTV PTV Defined As: The Expansion of the CTV to account for internal movement. (ex. Respiration) Contoured As: GTV+CTV+Motion Non-Coplanar Beam Arrangement Beams Eye View 3D Conformal Treatment Planning Section 6.4.2.1 3-Dimensional beam arrangements, both co-planar and non-coplanar, can be used. This protocol specifies that 10 or more static, non-opposing, beams should be utilized. The field size and shape should correspond identically to the PTV within the BEV. All normalization is done to the center of the PTV and all hotspots must remain inside it. Image From: www.IMRTCenter.com IMRT Treatment Planning Section 6.4.2.2 IMRT should only be chosen when 3D conformal planning does not adequately address target coverage, OAR dose limits, or dose spillage concerns. The protocol recommends about two to three segments per beam to avoid complex beam fluence issues. Dose spillage directly relates to the dose gradients observed at/past the PTV edges. Plan Evaluation Participant Safety and Wellbeing Remains Constant Throughout This Protocol: Plan evaluation can be performed by referencing the strict guidelines set forth by the RTOG. Tables throughout section 6.5 highlight the specific PTV dose coverage needs, the hot spot restrictions, as well as recommendations for dose gradients near organs at risk. Necessitating Thorough Plan Evaluation Figure From RTOG 0813 Sect. 6.5 Conformality & Dose Tolerance Section 6.5 Exceeding a max dose point is a protocol violation, however the other doses are suggested limits supported by current (2010) research. -PTV coverage tables indicate specific tolerable deviations based on PTV size (cc). [Table 1] Deviation from the specified PTV limits is against protocol standards. Tables Directly From RTOG Protocol 0813 In The End, Who Will Benefit From This Clinical Trial? Patients The Field of Radiation Oncology Participating Institutions Image From: www.themedicalbag.com Patients - Patients in RTOG Clinical Protocol 0813 receive SBRT treatments that deliver highly conformal, effective doses of radiation that can contribute to a longer, disease free, life. - SBRT is still used in 2015 and has contributed to some of the best clinical outcomes in patients with NSCLC, increased 5-year survival and local control improvements. [6] Image From: http://www.radonc.com/wp-content/uploads/2011/08/Patient-Linear-Accelerator1.jpg The Field of Radiation Oncology -Clinical trials contribute the the field of radiation oncology as a whole because they provide detailed information on current treatment options, emerging techniques, as well as in-depth comparisons that are only possible through these types of studies. -Without clinical trials such as RTOG 0813, the field would not evolve at such a rapid pace, further exemplifying the necessity these trials pose to the field. Participating Institutions - Every participating institution has gone through a rigorous registration and approval process that not only demonstrates they are capable of carrying out the procedure but also that they are capable of delivering a high-quality procedure consistently. - This prestige is something that attracts new staff, patients, and potential trial participants to the facility. THANK YOU FOR WATCHING! REFERENCES: 1. Bailey R. Anatomy of the heart: pericardium. About:Biology. http://biology.about.com/od/anatomy/a/aa050407a.htm. 2015. Accessed June, 2015. 2. Boundless. Anatomy and physiology: great vessels of the heart. https://www.boundless.com/physiology/textbooks/boundless-anatomy-andphysiology-textbook/the-cardiovascular-system-18/the-heart-172/great-vessels-of-the-heart-866-9331/. June, 2015. Accessed June, 2015. 3. Healthline Medical Team. Healthline body maps: esophagus. http://www.healthline.com/human-body-maps/esophagus. February, 2015. Accessed June, 2015. 4. Nachum N. The university of Texas Medical School E-Textbook for neurosciences - Chapter 3: anatomy of the spinal cord. http://neuroscience.uth.tmc.edu/s2/chapter03.html. 2015. Accessed June, 2015. 5. Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epideminology, etiology, and prevention. Clin Chest Med 2013;32:605-644. http://dx.doi.org/10.1016/j.ccm.2011.09.001 6. Allibhai Z,Taremi M, Bezjak A, Brade A, et al. The impact of tumor size on outcomes after stereotactic body radiation therapy for medically inoperable early-stage non-small cell lung cancer. Int J Rad Onc, Bio, Phys 2013;87:1064-1070. http://dx.doi.org/10.1016/j.ijrobp.2013.08.020 7. RTOG 0813: Seamless phase I/II study of stereotactic lung radiotherapy (SBRT) for early stage, centrally location, non-small cell lung cancer (NSCLC) in medically inoperable patients. (Last Update: 6/8/15) PI: Bezjak A. Princess Margaret Hospital / University of Toronto 8. Chung KC, Yang LJ, Mcgillicuddy JE. Practical management of pediatric and adult brachial plexus palsies. New York, NY: Edinburgh Publishing;2012. ISBN-13: 9781437705751.