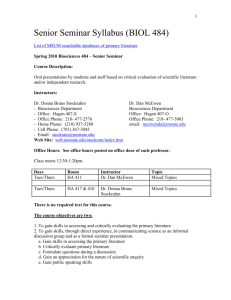
BIOL10004-23-2015-gs
advertisement

• https://www.youtube.com/watch?v=kkG eOWYOFoA BioSciences Q. If it takes only one sperm to fertilise an egg, why do we need millions of sperm in an ejaculate ? A. The sperm won’t stop to ask for directions. BioSciences Is it much further to the Fallopian tube? I think it may be – We’ve only just passed the tonsils. BioSciences Reproductive systems and hormones Professor Geoff Shaw Department of Zoology g.shaw@zoology.unimelb.edu.au • KLES5: Chapter 20; Chapter 28 esp gonads and HPG axis section pp 693-695, fig 28.11 • KLES4: Chapter 19; Chap 27, esp p 647-648, Fig 27.10 BioSciences Copyright Notice BioSciences The Sexual Life Cycle Fertilization diploid- 2n one cell zygote haploid- 1n 2n n n fertilization All other cells of the body: Somatic cells 2n Germ cell development individual germ stem cells 2n male 2n sperm n n n n n n female egg n n meiosis BioSciences see KLES4 Fig 19.4 mouse testis stained to show tubules inside BioSciences What are the main functions of the testis? Testes • sperm production – occurs in seminiferous tubules – controlled by Sertoli cells – spermatogenesis • hormone production – testosterone • steroid • androgen – made by Leydig cells between tubules Testosterone BioSciences Seminiferous tubule LUMEN sperm spermatid secondary spermatocyte primary spermatocyte Sertoli cell spermatogonium peritubular myoid cells BioSciences Sperm BioSciences KLES4 Fig 19.22a Ovaries egg (oocyte) • egg production – oogenesis – occurs in follicle – controlled by granulosa cells • hormone production – oestradiol • steroid - oestrogen • made by granulosa cells in follicle follicle CL – Progesterone • steroid - progestin • made by corpus luteum after ovulation oestradiol progesterone CL Mouse female reproductive tract: microscope slide • note the thick secretory lining of the uterus (endometrium), regulated by oestradiol and progesterone • multiple corpora lutea (CL) in this species (why?) BioSciences CL CL uterus ovary CL oviduct CL CL this section enlarged on previous slide Testis hormones - Testosterone • Testosterone – acts via androgen receptor in cells – stimulates accessory sex organs (eg prostate and seminal vesicles) – modulates male-type behaviour oestradiol Testosterone dihydro-testosterone (DHT) BioSciences Ovary hormones - oestradiol • Oestradiol – acts via oestrogen receptors in cells – controls oviduct, uterus, cervix, vagina and other sex organs – promotes oestrus behaviour (mating) Oestradiol BioSciences Ovary hormones - progesterone • Progesterone – acts via progestin receptors in cells – controls oviduct, uterus, cervix, vagina and other sex organs – modulates effects of oestradiol Progesterone BioSciences Control of testis other brain centres • hypothalamo-pituitary-gonadal axis • gonadotrophin releasing hormone hypothalamus (GnRH) from hypothalamus brain GnRH stimulates release of LH and FSH pituitary (the gonadotrophins) from the pituitary LH FSH • LH stimulates Testosterone testosterone production by testis • FSH stimulates spermatogenesis • testosterone inhibits GnRH accessory sex organs and secretion (negative feedback) secondary sex characters relatively constant T homeostatic control Control of ovary (follicle growth) other brain centres • hypothalamo-pituitary-gonadal axis • gonadotrophin releasing hormone hypothalamus (GnRH) from hypothalamus brain GnRH stimulates LH and FSH (the pituitary gonadotrophins) release from the pituitary LH FSH • FSH stimulates oestradiol – follicle growth/oogenesis growing follicles – oestradiol production • oestradiol regulates GnRH reproductive tract (negative feedback) Control of ovary (ovulation) • Large follicles HIGH oestradiol • HIGH E2 (+)ve feedback • Surge of LH causes ovulation + hypothalamus GnRH LH brain pituitary FSH oestradiol mature follicles/ ovulation reproductive tract preparation oestrous behaviour Control of ovary (after ovulation) other brain centres • ovulated follicle transforms to corpus luteum (corpora lutea) hypothalamus • oestradiol production falls brain GnRH • porgesterone production increases pituitary • progesterone negative feedback on FSH preventing follicle growth LH FSH • after about 2 weeks (human) CL progesterone regresses allowing increased FSH corpora lutea and follicle growth Uterus (preparation for pregnancy) menstrual cycle hormones (uterine lining) switch to positive feedback BioSciences see KLES5:Fig 28.11 http://upload.wikimedia.org/wikipedia/commons/c/cd/MenstrualCycle2.png Contraception • Combined oral contraceptive pill – progestin plus oestrogen – suppresses GnRH ↓ FSH and LH – prevents follicle growth and ovulation Progestin/ oestrogen - hypothalamus GnRH LH brain pituitary FSH oestradiol reproductive tract BioSciences A male contraceptive pill? BioSciences see KLES4 Box 19.2 Methods of Contraception Vasectomy Tubal Ligation From: Life, Purves et al., 6th Ed BioSciences Ch.42 Animal Reproduction Contraceptive effectiveness % of women getting pregnant within 1 year Typical use Perfect use 85 85 29 18 “rhythm method” abstinence near time of ovulation 35 15 condom (male) 15 2 8 0.3 0.05 0.05 0.2-0.8 0.2-0.6 Method Mechanism No method Spermicides kill sperm prevents sperm entering vagina contraceptive pill prevent ovulation implanon prevents ovulation IUD prevents embryo implantation vasectomy prevents release of sperm 0.15 0-0.1 tubal ligation prevents egg from entering uterus 0-0.5 0-0.5 http://www.contraceptivetechnology.org/table.html ZOOLOGY: Further Studies Physiological Aspects 2nd Year Animal structure and function Comparative Animal Physiology 3rd Year Reproduction Research Project Concepts in Cell & Devel Biology Developmental Sex: Science Biology and Society (University breadth) BioSciences http://www.lectureroftheyear.com.au/ BioSciences Next Lectures… Developmental Biology, Digestion, Feeding and Nutrition Dr Stephen Frankenberg BioSciences What do I expect you to learn from this lecture? • • • • meiosis and the alternation of haloid and diploid generations structure and functions of the testis – sperm and testosterone stages of spermatogenesis and structure of mature sperm structure and function of the ovary – eggs, follicles (oestradiol), CL (progesterone) • hypothalamo-pituitary control of testis and ovary • hormonal control and the menstrual cycle • contraceptives – mechanisms and efficiency BioSciences BioSciences HYPOTHALAMUS hypothalamus pituitary hypothalamus pituitary PITUITARY GONADS