Powerpoint 26 Reproduction
advertisement

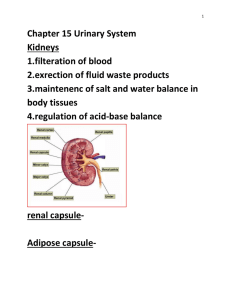
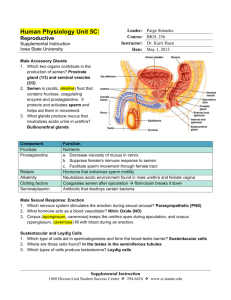
The Reproductive Systems A. Male reproductive system 1. Scrotum 2. Testes a. Spermatogenesis b. Spermatozoa c. Hormones of the braintesticular axis 3. Ducts a. Ducts of the testis b. Epididymis c. Ductus (vas) deferens d. Ejaculatory ducts e. Urethra 4. Accessory sex glands 5. Semen 6. Penis B. Female reproductive system 1. Ovaries a. Oogenesis 2. Uterine (fallopian) tubes 3. Uterus 4. Vagina 5. Vulva 6. Perineum 7. Mammary glands C. Female reproductive cycle 1. Hormonal regulation 2. Phases of the female reproductive cycle a. Menstrual phase (menstruation) b. Preovulatory phase c. Ovulation d. Postovulatory phase D. Physiology of sexual intercourse What is reproduction? What is the essential difference between mitosis and meiosis? How are the organs of reproduction grouped according to function? 1. gonads 2. ducts 3. accessory glands Male Reproductive System Scrotum 1. 2. 3. 4. Dartos' fascia cremaster muscle temperature regulation cremaster reflex Other Male Structures 1. 2. 3. 4. 5. descent of the testes spermatic cord inguinal canal deep inguinal ring superficial inguinal ring Testes 1. inguinal canals 2. tunica vaginalis 3. tunica albuginea 4. 200 - 300 lobules 5. seminiferous tubules _______________________ spermatogenesis Spermatogenesis 1. spermatogonium (2n) a. mitosis b. meiosis 2. 1° spermatocyte (2n4c) 3. 2 2° spermatocytes (1n2c) 4. 4 spermatids (1n1c) spermatogonia 1o spermatocyte 2o spermatocyte spermatids spermatozoa Spermatozoa 1. spermiogenesis (Sertoli cell) a. nourishment b. protection c. anatomical maturation (head, midpiece, tail) 2. 300 million/day 3. life expectancy =72 hrs (up to 6 days) Male Sex Hormones 1. Gn-RF 2. FSH and LH 3. Sertoli cells =inhibin 4. interstitial endocrinocytes (Leydig cells) = testosterone Hormonal Control of Male Reproduction hypothalamic Gn-RF negative feedback anterior pituitary gland follicle-stimulating hormone luteinizing hormone negative feedback testes sustentacular cells prepares for spermiogenesis spermatogonia enter spermatogenesis interstitial cells testosterone secretion inhibin secretion development of primary male sex characteristics (before birth) development of secondary male sex characteristics (beginning at puberty) 1.enlargement of sex organs 2.activation of accessory organs 3.beginning of sexual behavior 4.increased protein anabolism 5.required for spermatogenesis and spermiogenesis Male Ducts 1. straight tubules --> rete testis --> efferent ductules --> 2. ductus epididymis a. functional maturation b. storage (40-60 days) c. resorption 3. ductus (vas) deferens a. path in the body b. ampulla of the vas Male Ducts, Con’t 4. ejaculatory ducts 5. urethra a. prostatic b. membranous c. penile Accessory Sex Glands 1. seminal vesicles 2. prostate gland 3. bulbourethral glands Accessory Gland Fluid Components 1. seminal vesicle fluid (60% of semen) a. Fructose, citrate b. prostaglandins c. proseminogelin 2. prostatic fluid (30% of semen) a. Calcium, citrate, phosphate b. clotting enzymes c. Serine protease (PSA) 3. bulbourethral fluid (trace) a. mucous b. buffers Semen (seminal fluid) = sperm + accessory gland secretions Semen (sperm + seminal fluid) Sperm (10%) + accessory gland secretions (90%) 2 – 5 ml per ejaculate with 50 – 120 million sperm per ml What happens at ejaculation? 1. Prostatic fluid and seminal vesicle fluids mixed at emission proseminogelin seminogelin by prostatic clotting enzymes semen becomes sticky entangles sperm, sticks semen to vaginal and cervical surfaces prevents semen from draining out of vagina 2. Prostatic serine protease breaks down seminogelin after 20-30 min semen liquifies sperm become very active prostaglandins help to thin cervical mucus plug and may stimulate uterine contractions, helping sperm into uterine cavity 3. Two requirements for sperm motility are met vaginal pH (3.5 – 4.0) brought to 7.5 fructose and other sugars provide substrate for sperm ATP production Penis 1. root (bulb and crura) 2. body (a) corpora cavernosa (b) corpus spongiosum 3. glans (prepuce) _______________________ erection Female Reproductive System Organs include: 2 ovaries 2 uterine tubes (oviducts/Fallopian tubes) 1 uterus 1 vagina external genitalia ________________________ mammary glands Ovaries 1. 2. 3. 4. 5. 6. development location germinal epithelium tunica albuginea stroma follicles Oogenesis 1. mitosis in fetal life 2. arrested meiosis 3. 7 million at 5th month --> 2 million at birth --> 40,000 at puberty (~480 ovulations = ~13/yr = ~37 yr) 4. Gn-RF 5. FSH 6. LH 7. estrogen Arrested in prophase I 2n4c Arrested in metaphase II 1n2c Ovarian Follicles ( immature oocyte + follicular cells) Ovarian cycle (6 Stages) 1. primordial follicle- primary oocyte arrested in prophase I, thin layer of follicular cells 2. primary follicle- meiosis resumes, consists of primary oocyte and one to several layers of follicular cells 3. secondary follicle- consists of secondary oocyte arrested in meiosis II. (metaphase II) Contains antrum- fluid filled pools or small cavity 4. tertiary follicle- consists of secondary oocyte with very large antrum. (mature graafian follicle) 5. corpus luteum- remants of follicle after ovulation 6. corpus albicans- scarred over follicle Ovarian Cycle 1. Primordial follicle 2. Primary follicle 3. Secondary follicle 4. Tertiary follicle 5. Corpus Luteum 6. Corpus Albicans Uterine Tubes 1. location 2. sections a. fimbriae b. infundibulum c. ampulla d. isthmus 3. histology Ciliated simple columnar Uterus 1. location 2. sections a. fundus b. corpus (body) c. cervix (mucous plug) 3. anteverted Uterus Continued 4. rectouterine pouch vesicouterine pouch 5. blood supply a. uterine arteries b. spiral arterioles Uterus Histology 6. histology a. perimetrium b. myometrium c. endometrium (1) stratum basalis (2) stratum functionalis Vagina 1. 2. 3. 4. 5. 6. anatomy fornix rugae introitus hymen mucosa a. glycogen b. no glands Vulva 1. 2. 3. 4. 5. mons pubis labia majora labia minora clitoris (prepuce) vestibule a. urethral orifice b. vaginal introitus c. vestibular glands 6. bulb of the vestibule Perineum -urogenital triangle -anal triangle Mammary Glands 1. 2. 3. 4. 5. 6. 7. location 15 - 20 lobes ducts nipple areola development lactation Female Reproductive Cycle 1. ovarian cycle 2. uterine (menstrual) cycle Hormonal Regulation hypothalamic Gn-RF 1. 2. 3. 4. 5. 6. 7. Gn-RF FSH LH estrogen progesterone inhibin relaxin anterior pituitary gland FSH LH ovaries follicle development ovulation corpus luteum estrogen relaxin inhibin progesterone estrogen relaxin -- relaxes pubic symphysis/cervical dilation inhibin -- inhibits Gn-RF and FSH progesterone -- stimulates secretory endometrium prepares mammary glands for milk synthesis estrogen -- primary sex characteristics (before birth) secondary sex characteristics (at puberty) enlargement of sex organs female sexual behavior (with testosterone) endometrial proliferation increased proteins anabolism aids in fluid and electrolyte balance Control of Ovulation by Hormones of the Pituitary-Ovarian Axis Estrogen (EST) secretion and its control 1. EST is secreted by follicular cells prior to ovulation and by the corpus luteum after ovulation. 2. Moderate levels of EST inhibit Gn-RF secretion and thus inhibit secretion of FSH and LH. 3. Low levels of EST allow Gn-RF secretion and prime the anterior pituitary gland to secrete FSH, which stimulates follicular development at the beginning of a new cycle. 4. High levels of EST allow Gn-RF secretion and prime the anterior pituitary gland to secrete LH, which stimulates ovulation and formation of the corpus luteum. Female Cycle Phases 1. menses (days 1 - 5) 2. preovulatory (days 6 - 13) 3. ovulation (day 14) 4. postovulatory (days 15 - 26) 5. ischemic (days 26-28) Ovarian cycle: pink Uterine cycle: green ovulation | | | 1 5 14 26 28 <--------> <---------------> <---------------> <--------> menses proliferative secretory ischemic <---------------------------> <----------------------------> preovulatory postovulatory (follicular) (luteal) Female Cycle Phase Descriptions 1. menses (days 1 - 5) greatly diminished blood estrogen and progesterone levels; stratum functionalis dead and shedding; low estrogen stimulates Gn-RF + FSH 2. preovulatory(days 6 - 13) new follicles developing and secreting estrogen; rising blood estrogen causes mitosis of stratum basalis and rebuilding of stratum functionalis 3. ovulation (day 14) high estrogen stimulates Gn-RF + LH, thus stimulating ovulation; as a result corpus luteum is formed 4. postovulatory (days 15 - 26) corpus luteum produces estrogen + progesterone; stratum functionalis becomes secretory: 1. retains water 2. uterine glands secrete glycogen 3. spiral arterioles rapidly develop 5. ischemic (days 26-28) corpus luteum dying; blood estrogen and progesterone levels dropping; spiral arterioles vasoconstrict for 6 hours at a time; stratum functionalis begins to die The Female Reproductive Cycle Endometrial Changes through the Menstrual Cycle Sexual Responses Male Female 1. excitement -- erection -- lubrication 2. orgasm -- emission orgasm -- expulsion (both) 3. resolution -- detumescence -- refractory period 1. excitement and plateau -- vaginal transudate -- lubrication from glands -- orgasmic platform -- tenting effect 2. orgasm 3. resolution -- detumescence parasympathetic/sympathetic Stages of Male Sexual Response Stages of Female Sexual Response