The Reproductive System
advertisement

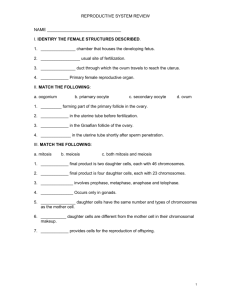
The Reproductive System Function Preview Ensures continuity of the species by producing offspring In sexual reproduction new individuals are produced by the fusion of haploid gametes to form a diploid zygote. Sperm are male gametes, ova (ovum singular) are female gametes. Function Preview Meiosis produces cells that are genetically distinct from each other; fertilization is the fusion of two such distinctive cells that produces a unique new combination of alleles, thus increasing variation on which natural selection can operate. Function Preview Sexual reproduction offers the benefit of generating genetic variation among offspring, which enhances the chances of the population's survival. Anatomy of the Male Reproductive System Common purpose Identify the organs and discuss the general function of each Testes: Exocrine and endocrine functions Anatomy of the Male Reproductive System Composition of semen and the glands that produce it Erection, ejaculation and circumcision Meiosis and spermatogenesis Sperm structure and how it relates to its function Anatomy of the Male Reproductive System FSH and LH: Its effect on testes functioning Anatomy of the Female Reproductive System Identify the organs of the female reproductive system and discuss the general functions Vesicular follicle and corpus luteum of the ovary Endometrium, myometrium and ovulation Anatomy of the Female Reproductive System Locate the female uterus: cervix, fundus and body What is oogeneis What is the influence of FSH and LH on ovarian function Phases and controls of the menstrual cycle Anatomy of the Female Reproductive System Function and structure of the mammary glands Fertilization and zygote Implantation Placenta and its functions Three stages of labor Overview Primary sex organs are the gonads Testes and ovaries Gonads produce sex cells: gametes Accessory reproductive organs The reproductive role of the male is to produce sperm, deliver them to the female Overview Female provide female gametes or ova The joining of a sperm and ova causes a fusion or a fertilized egg which is the first cell of a new individual Overview After fertilization the female uterus provides a protective environment for the embryo, later called the fetus, which develops until birth Overview Human reproduction employs internal fertilization, and depends on the integrated action of hormones,the nervous system, and the reproductive system. Gonads are sex organs that produce gametes. Male gonads are the testes, which produce sperm and male sex hormones. Female gonads are the ovaries, which produce eggs (ova) and female sex hormones. Anatomy of the male Reproductive System Testes are suspended outside the abdominal cavity by the scrotum, a pouch of skin that keeps the testes close or far from the body at an optimal temperature for sperm development. Anatomy of the male Reproductive System Seminiferous tubules are inside each testis, and are where sperm are produced by meiosis. About 250 meters (850 feet) of tubules are packed into each testis. Spermatocytes inside the tubules divide by meiosis to produce spermatids that in turn develop into mature sperm. The male reproductive system. Images from Purves et al., Life: The Science of Biology, 4th Edition, by Sinauer Associates (www.sinauer.com) and WH Freeman (www.whfreeman.com), used with permission. Testes Fibrous connective tissue capsule: Tunica albuginea Septa or extensions form this capsule divides the testes into lobules. Within the lobules are the sperm- forming factories- seminferous tubules Testes The sperm empty into the rete testis and travel to the epididymis Surrounding the seminiferous tubules are interstitial cells, functionally distinct cells that produce androgens- most important is testosterone Testes In the male spermproducing and hormone producing function of the testes are carried out by two completely different cell populations Accessory Organs Epididymis Ductus deferens, vas deferens Urethra Accessory Organs Epididymis Epididymis First part of the male duct system Provides a temporary storage site for immature sperm It takes 20 days to get here and the sperm mature gaining the ability to swim Sexual stimulation causes the walls to contract and expel the sperm into the ductus deferens Ductus Deferens This is a low power image of the Ductus Deferens or Vas Deferens. Notice the Stellate shaped lumen that is a characteristic of the duct (red arrow), along with the very thick smooth muscle walls indicated by the blue arrows. Red arrow - Stellate Shaped Lumen Of Vas Deferens Blue arrow - Thick Muscular wall of Vas Deferens Ductus Deferens Runs upward from the epididymis through the inguinal canal into the pelvic cavity It is enclosed along with blood vessels and nerves in a connective tissue sheath: spermatic cord Ductus Deferens The end of the ductus deferens empties into the ejaculatory duct, which passes through the prostate gland and merges with the urethra Main function is to propel live sperm from the epididymis (storage space) and the distal part of the ductus deferens into the urethra Physical prevention (most effective) include vasectomy. Vasectomy: the vas deferens connecting the testes with the urethra is cut and sealed to prevent the transport of sperm. Urethra Terminal part of the male duct system Three named regions Prostatic urethra- prostrate gland Membranous urethra Spongy urethra- running within the length of the penis Accessory Gland and Semen Paired seminal vesicles Prostrate gland Bulbourethral glands (Cowper’s gland) These glands produce the bulk of the semen Seminal Vesicles Produce about 60% of semen fluid Fructose, Vitamin C. prostoglandins and other substances which nourish and activate the sperm passing through the tract Sperm and seminal fluid enter the urethra together during ejaculation Prostate Gland Produce a milky secretion that plays a role in activating sperm Prostrate cancer is the third most prevalent cancer in men Hypertrophy of the prostrate strangles the urethra: Cystitis and kidney damage Bulbourethral Glands Produce a thick, clear mucus that drains into the penile urethra This secretion is the first to pass down the urethra when a man becomes sexually excited Cleanses traces of acidic urine and serves as a lubricant during intercourse Semen Milky white, sticky mixture of sperm and accessory gland secretions Provides a transport medium Contains nutrients and chemicals that protect the sperm and aid its movement Fructose provides the energy Alkalinity of semen (ph 7.2-7.6) Semen Neutralizes the acid environment of vagina (pH 3.5 - 4) Contains seminal plasmin ( inhibits bacterial multiplication) Hormone relaxin and enzymes that enhance sperm mobility Spermatogenisis Sperm production begins at puberty at continues throughout life, with several hundred million sperm being produced each day. Once sperm form they move into the Human Sperm (SEM x5,785). This image is epididymis, where copyright Dennis Kunkel at www.DennisKunkel.com, they mature and are used with permission. stored. Spermatogenesis Begins in seminiferous tubules: Spermatogonia FSH- at puberty causes the production of stem cell (daughter cell A) and daughter cell B Type B- Primary spermatocyte and undergoes meiosis to form four spermatids (gametes) Spermiogeneis Head contains: DNA Midpiece: Centrioles that form filaments of the tail Tail: Mitochondria are wrapped tightly around filaments to provide ATP The entire process of spermatogenesis takes 64-72 days Male Sex Hormones The anterior pituitary produces folliclestimulating hormone (FSH) and luteinizing hormone (LH) or interstitial cell- stimulating hormone (ICSH). Action of LH is controlled by the gonadotropin-releasing hormone (GnRH). Male Sex Hormones LH stimulates cells in the seminiferous tubules to secrete testosterone, which has a role in sperm production and developing male secondary sex characteristics. FSH acts on cells to help in sperm maturation. Negative feedback by testosterone controls the actions of GnRH. Secondary Sex Characteristics Deepening of the voice due to the enlargement of the larynx Increases hair growth all over the body Enlargement of skeletal muscles to produce heavier muscle mass Increased heaviness of the skeleton due to thickening of the bones Anatomy of the Female Reproductive System More complex Produces female gametes (ova) Nurture and protect the developing fetus Ovaries are the primary reproductive organs Ovaries produce both an exocrine product (ova) and endocrine products ( estrogens and progesterone) www.gynaesurgeon.co.uk/anatomy/anatomy6.htm Ovaries Paired and contain saclike structures called ovarian follicles Each follicle consists of an immature egg (oocyte) surrounded by follicle cells As follicle matures it enlarges and develops a fluid-filled center: antrum Ovaries The follicle is now called a vesicular or Graafian follicle: the developing egg is ready for ovulation After ovulation the ruptured follicle is transformed into the corpus luteum which eventually degenerates Ovulation generally occurs every 28 days Duct System Uterine tubes Uterus Vagina The female reproductive tract Duct System The reproductive system of a women is entirely internal. The vagina is the passage that leads from the outside of the body to the cervix, which is the opening to the uterus. The uterus is the muscular organ where a fertilized egg attaches and develops. It is about the size and shape of a pear, and is lined with a rich and nourishing mucous membrane called the endometrium. Fallopian Tubes Forms the initial part of the duct system Receives the ovulated oocyte Provides a site where fertilization can occur Enclosed and supported by a broad ligament Fallopian Tubes Unlike the male duct system, no actual contact between the uterine tubes and the ovaries Distal end expands into infundibulum which has finger-like projections( fimbriae) Fimbriae create fluid currents to carry the oocyte into the uterine tube Fallopian Tubes Oocyte is carried to the uterus by peristalsis and rhytmic beating of cilia Takes 3-4 days to get to the uterus Oocyte is viable up to 24 hours after ovulation Usual site for fertilization is the uterine tube www.2womenshealth.co.uk/Figure02-01.htm Uterus Womb Located in the pelvis between the urinary bladder and the rectum Receives, retains and nourishes the fertilized egg The major portion is the body Uterus Superior rounded region above the entrance of the uterine tubes is the fundus Narrow outlet that protrudes into the vagina beow is the cervix Duct System From the top of the uterus extend the fallopian tubes, which lead backward and downward to the ovaries. www.afraidtoask.com/STD/stdanatomy.html sprojects.mmi.mcgill.ca/gynecology/anatute.html www.gynaesurgeon.co.uk/anatomy/anatomy6.htm Uterus Three layers Inner layer or mucosa is the endometrium if fertization ocurs, the fertilized egg implants into the endometrium Myometrium is the bulky middle layer Composed of smooth muscle Active role during the delivery of the baby Uterus Three layers Perimetrium or viseceral peritoneum Outer serous layer Menses When not pregnant the endometral lining sloughs off periodically Usually every 28 days Responds to the levels of the ovarian hormones Vagina Birth canal Provides a passageway for the delivery of the baby Provides a oassageway for menstrual flow to leave the body Receives the penis and semen Female organ of copulation Vagina Distal end is partially closed by the hymen Very vascular and tends to bleed if ruptured If too tough it is surgically ruptured to allow for intercourse External Genitalia Called the Vulva collectively Mons pubis Labia Clitoris Urethral and vaginal orifices Greater vestibular glands A: Prepuce (Hood) of Clitoris B: Clitoris C: Opening of Urethra (urinary tract) D: Labia minora E: Labia majora F: Opening of Vagina G: Vestibule H: Hyman tissue (residual) I: Opening of Anus Vulva The MONS, a name that comes from the Latin mons veneris means mound of Venus, the Roman goddess of love, is the area of fatty tissue that forms a soft mound over the pubic bone. The mons is covered by skin and pubic hair. Vulva The LABIA MAJORA, or OUTER LIPS, extend from the mons to the anus. They cover the urinary and vaginal openings and are in turn covered by pubic hair. The LABIA MINORA, or INNER LIPS, are delicate folds of moist skin that lie inside the outer lips, although they can protrude beyond them. They extend from just above the clitoris to below the vaginal opening. They vary in size and form in each woman. Vulva The CLITORIS is an exquisitely sensitive organ that lies just under the mons. It is covered by the inner lips which can be gently pushed back to reveal the tip (the head or glans). The rest of the clitoris can be seen because it extends inside the body. The clitoris is extremely sensitive to stimulation and when stimulated it becomes erect. Although direct stimulation of the tip of the clitoris is pleasurable for some women it is uncomfortable and even painful for others. Vulva The URINARY OPENING is just under the clitoris. It is the outer part of the urethra, the tube from the bladder. The VAGINAL OPENING is located behind the urinary opening. During sexual stimulation erectile tissue on both sides of the vagina become engorged with blood. The whole area becomes moist. The pelvic muscles contract and relax during orgasm. One- to two-thirds of the vaginal opening is covered with the HYMEN until this is broken by intercourse or penetration or another object or even bicycle or horseback riding. Vulva The VAGINA lies between the urethra and the rectum. Unless a woman is sexually stimulated the walls of the vagina touch each other. When a woman is sexually aroused a slippery liquid is produced and the vagina opens, or enlarges. ( Greater Vestibular Glands) The vagina can open as much as to facilitate the passage of a baby, therefore there is no such thing as a penis too large for a woman's vagina . www.2womenshealth.co.uk/Figure02-02.htm Female Reproductive Functions and Cycles Oogenesis: Meiosis to produce female gametes The ovary contains many follicles composed of a developing egg surrounded by an outer layer of follicle cells. Each egg begins oogenesis as a primary oocyte. At birth each female carries a lifetime supply of developing oocytes, each of which is in Prophase I. Female Reproductive Functions and Cycles A developing egg (secondary oocyte) is released each month from puberty until menopause, a total of 400-500 eggs. Oogenesis In the female fetus: oogonia or the female stem cells Rapidly multiply Daughter cells, the primary oocytes, push into the ovary connective tissue Surrounded by a single layer of cells and form the primary follicles Oogenesis By birth the oogenia are no longer exist and a lifetime supply of primary oocytes exists; arrested in prophase I During puberty, the anterior pituitary secretes FSH Stimulates a small number of follicles to grow and mature Ovulation occurs Oogenesis. The above image is from http://www.grad.ttuhsc.edu/courses/histo/notes/female.html. Ovarian Cycle Cyclic changes that occur monthly At puberty, 400,000 oocytes remain Small number activated each month Follicle prodded by FSH grows it accumulates fluid in the center: antrum Primary oocyte undergoes first meiotic division Produces: Ovarian Cycle Secondary oocyte Polar body The vesicular follicle contains a secondary oocyte 14 days Ovualation of secondary oocyte occurs in response to LH Ovulated secondary oocyte still surrounded by capsule now called the corona radiata Ovarian Cycle LH stimulus causes rupture and release of oocyte into peritoneal cavity Vesicular follicles that do not ovulate overripe and deteriorate LH causes the ruptured follicle to change into corpus luteum Secondary oocyte if penetrated by sperm its nucleus undergoes the second meiotic division that produces another polar body and the ovum nucleus Meiosis in females yields only one functional ovum and three tiny polar bodies Ovarian Cycles After puberty the ovary cycles between a follicular phase (maturing follicles) and a luteal phase (presence of the corpus luteum). These cyclic phases are interrupted only by pregnancy and continue until menopause, when reproductive capability ends. Ovarian Cycles During the first phase, the oocyte matures within a follicle. At midpoint of the cycle, the oocyte is released from the ovary in a process known as ovulation. Following ovulation the follicle forms a corpus luteum which synthesizes and prepares hormones to prepare the uterus for pregnancy. Ovarian Cycle If secondary oocyte is not penetrated it deteriorates Ovarian Cycle The ovarian cycle is http://www.emc.maricopa. edu/faculty/farabee/BIOB K/BioBookREPROD.html hormonally regulated in two phases. The follicle secretes estrogen before ovulation The corpus luteum secretes both estrogen and progesterone after ovulation. Ovarian Cycle The ovarian cycle covers events in the ovary The menstrual cycle occurs in the uterus. Menstrual Cycle Menstrual cycles vary from between 15 and 31 days. Menses Days 1-5 The first day of the cycle is the first day of blood flow (day 0) known as menstruation. During menstruation the uterine lining is broken down and shed as menstrual flow. FSH and LH are secreted on day 0, beginning both the menstrual cycle and the ovarian cycle. Menstrual Cycle Menstrual cycles vary from between 15 and 31 days. Menses Days 1-5 Both FSH and LH stimulate the maturation of a single follicle in one of the ovaries and the secretion of estrogen. Menstrual Cycle Menstrual cycles vary from between 15 and 31 days. Proliferative stage Days 6-14 Rising levels of estrogen in the blood trigger secretion of LH Basal layer of endometrium regenerates stimulates follicle maturation and ovulation LH stimulates the remaining follicle cells to form the corpus luteum, which produces both estrogen and progesterone. Menstrual Cycle Menstrual cycles vary from between 15 and 31 days. Secretory stage 15-31 Estrogen and progesterone stimulate the development of the endometrium and preparation of the uterine inner lining for implantation of a zygote. If pregnancy does not occur, the drop in FSH and LH cause the corpus luteum to disintegrate. The drop in hormones also causes the sloughing off of the inner lining of the uterus by a series of muscle contractions of the uterus. Secondary Sex Characteristics Caused by estrogens (estradiol, estrone, estriol) Estradiol is the most abundant and responsible for mediating estrogenic effects Secondary Sex Characteristics Enlargement of accesory organs of the femaale reproductive system Uterine tubes Uterus Vagina vulva Development of the breasts Secondary Sex Characteristics Appearance of axillary and pubic hair Increased deposits of fat beneath the skin Hips Breasts Widening and lightening of the pelvis Onset of the menstrual cycle Mammary Glands Mammary glands develop from distinctive mammary ridges running along both sides of the trunk of a mammalian embryo. Mammary glands are found in both sexes, but cease development in males well before puberty. Mammary Glands Mammary glands are probably highly modified sweat glands. reasonable to suggest that their origin was correlated with the development of milk teeth and the pattern of tooth replacement (diphyodonty) seen in most modern mammals. Milk teeth are probably not as efficient as adult teeth at chewing, due partly to their small size and partly to their ever-changing pattern of occlusion as the young mammal grows. Mammary Glands This lack of efficiency is accommodated by reliance on a food that doesn't need to be chewed, milk. Mammary glands are made up of a system of ducts surrounded by glandular tissue, which secretes milk. Mammary Glands Milk formation is stimulated by the hormones prolactin and growth hormone Secretion of these hormones is in turn stimulated by the act of suckling. Numerous ducts discharge to the surface of a fleshy protuberance called a nipple. Milk contains high percentages of protein, fat, and sugars (especially lactose), and some amount of vitamins and salts. Fertilization transmission of genes from both parents to offspring restoration of the diploid number of chromosomes reduced during meiosis initiation of development in offspring The egg and sperm. Sperm are color enhanced (green) while the egg is color enhanced to gold. The above image is modified from http://130.102.208.100/FMRes/FMPro?db=images.fp3&key=32931&-img. Sperm on the surface of a human egg. This image is from http://130.102.208.100/FMRes/FMPro?db=images.fp3&key=32932&-img. Fertilization Steps Contact between sperm and egg Entry of sperm into the egg Fusion of egg and sperm nuclei Activation of development Embryonic Events Cleavage is the first step in development of multicelled organisms. Cleavage converts a single-celled zygote into a multicelled embryo by mitosis. The blastocyst or chorionic vesicle is produced by mitosis of the zygote, and is a ball of cells surrounding a fluid-filled cavity (the blastocoel). Embryonic Events The decreasing size of cells increases their surface to volume ratio, allowing for more efficient oxygen exchange between cells and their environment. RNA and information carrying molecules are distributed to various parts of the blastula, and this molecular differentiation sets the stage for the layering of the body Embryonic Events Gastrulation involves a series of cell migrations to positions where they will form the three primary cell layers. Ectoderm forms the outer layer. Endoderm forms the inner layer. Mesoderm forms the middle layer. Embryonic Events Mesoderm forms structures associated with movement and support: body muscles, cartilage, bone, blood, and all other connective tissues. Reproductive system organs and kidneys come from mesoderm. Embryonic Events Endoderm forms tissues and organs associated with the digestive and respiratory systems. Many endocrine structures, such as the thyroid and parathyroid glands, are formed by the endoderm. The liver, pancreas, and gall bladder arise from endoderm. Embryonic Events Ectoderm tissues associated with outer layers: skin, hair, sweat glands, epithelium. The brain and nervous system also develop from the ectoderm. Implantation The uterine lining becomes enlarged and prepared for implantation of the embryo in the trophoblast layer. Twelve days after fertilization, the trophoblast has formed a two-layered chorion. Human chorionic gonadotropin (hCG) is secreted by the chorion, and prolongs the life of the corpus luteum until the placenta begins to secrete estrogen and progesterone. Home pregnancy tests work by detecting elevated hCG levels in the woman's urine. Implantation Your Placenta or Mine? Maternal and embryonic structures interlock to form the placenta, the nourishing boundary between the mother's and embryo's systems. The umbilical cord extends from the placenta to the embryo, and transports food to and wastes from the embryo. Changes in the zygote from fertilization to implantation. The above image is from http://www.biosci.uga.edu/almanac/bio_103/notes/apr_15.html. Stages of Development The period of time from fertilization to birth (usually 9 months) is divided into trimesters, each about three months long. During pregnancy the zygote undergoes 40 to 44 rounds of mitosis, producing an infant containing trillions of specialized cells organized into tissues and organs. Stages of Development The First Trimester The three embryonic tissue layers form. Cellular differentiation begins to form organs during the third week. After one month the embryo is 5 mm long and composed mostly of paired somite segments. During the second month most of the major organ systems form, limb buds develop. Stages of Development The First Trimester The embryo becomes a fetus by the seventh week. Beginning the eighth week, the sexually neutral fetus activates gene pathways for sex determination, forming testes in XY fetuses and ovaries in XX fetuses. External genitalia develop. Stages of Development The Second Trimester The fetus increases in size during this trimester, and bony parts of the skeleton begin to form. Fetal movements can be felt by the mother. Stages of Development The Last Trimester During this trimester the fetus increases in size. Circulatory and respiratory systems mature in preparation for air breathing. Fetal growth during this time uses large parts of its mother's protein and calcium intake. Maternal antibodies pass to the fetus during the last month, conferring temporary immunity. Birth Birth is a positive feedback hormonal mechanism. During birth the cervix dilates to allow passage of the fetus. Uterine contractions propel the fetus through the birth canal, usually head first. Hormonal control of the birth process involves the release of oxytocin and prostaglandins, which are stimulated by uterine contractions, which stimulate more hormones that cause more contractions....etc. Birth First Stage: Dilation stage The first stage of birth lasts from beginning of contractions to the full (10 cm) dilation of the cervix. Membranes of the amniotic fluid rupture, lubricating the vagina.( breaking the water) Birth Second Stage: Expulsion stage Strong uterine contractions of a minute in duration separated by two to three minute intervals propel the fetus down the birth canal. Abdominal muscles relax in synchrony with the uterine contractions. Vertex position: head-first Breech: buttocks- first Birth Third Stage: Placental stage After delivery of the baby, the umbilical cord is clipped and cut. The placenta (or afterbirth) in expelled through the vagina. Birth Milk Production Nursing mothers have their hormone levels and uterine size return to normal much faster than non-nursing mothers. Breasts develop the capability for milk secretion about the mid point of pregnancy. Secretion of milk does not occur until delivery, and the action of prolactin. Suckling by the infant causes production of oxytocin to promote release of milk into the ducts emptying into the nipple.