Review Q and A ch 10
advertisement

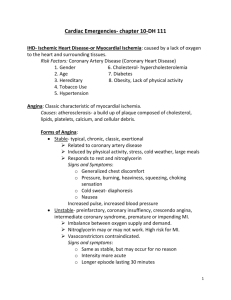
8-13 1. The most common cause of myocardial ischemia is: ◦ ◦ ◦ ◦ A. obesity B. cigarette smoking C. atherosclerosis D. hypertension 8-13 1.The most common cause of myocardial ischemia is: ◦ ◦ ◦ ◦ A. obesity B. cigarette smoking C. atherosclerosis D. hypertension 8-13 2. The age advantage that women have over men in the development of CHD is most likely related to A. better lifestyle habits B. the protective effects of estrogen C. a lower incidence of hypertension D. a lower incidence of diabetes 8-13 2. The age advantage that women have over men in the development of CHD is most likely related to A. better lifestyle habits B. the protective effects of estrogen C. a lower incidence of hypertension D. a lower incidence of diabetes 8-13 3. Cigarette smoking contributes to the development of coronary artery disease in all of the following ways except one. Which one is the exception? ◦ A. Tobacco use accelerates the development of coronary plaques. ◦ B. Tobacco use promotes plaque rupture ◦ C. Tobacco use promotes coronary thrombosis ◦ D. Tobacco use causes vasodilatation and hypotension. 8-13 3. Cigarette smoking contributes to the development of coronary artery disease in all of the following ways except one. Which one is the exception? ◦ A. Tobacco use accelerates the development of coronary plaques. ◦ B. Tobacco use promotes plaque rupture ◦ C. Tobacco use promotes coronary thrombosis ◦ D. Tobacco use causes vasodilatation and hypotension. 8-13 4. In individuals over the age of 50, systolic blood pressure greater than ______ is a more important risk factor than diastolic blood pressure. ◦ ◦ ◦ ◦ A. 150 mmHg B. 130 mmHg C. 140 mmHg D. 125 mmHg 8-13 4. In individuals over the age of 50, systolic blood pressure greater than ______ is a more important risk factor than diastolic blood pressure. ◦ ◦ ◦ ◦ A. 150 mmHg B. 130 mmHg C. 140 mmHg D. 125 mmHg 8-13 5. If a patient with angina has had no changes in the cause, frequency, or duration of anginal symptoms in the previous 60 days, he or she is considered to have ◦ ◦ ◦ ◦ A. unstable angina B. stable angina C. vasoplastic angina D. variant angina 8-13 5. If a patient with angina has had no changes in the cause, frequency, or duration of anginal symptoms in the previous 60 days, he or she is considered to have ◦ ◦ ◦ ◦ A. unstable angina B. stable angina C. vasoplastic angina D. variant angina 8-13 6. A sharp, stabbing chest pain that can be localized and is aggravated by movement or breathing is symptomatic of ◦ ◦ ◦ ◦ A. variant angina B. unstable angina C. non-cardiac related chest pain D. an acute myocardial infarction 8-13 6. A sharp, stabbing chest pain that can be localized and is aggravated by movement or breathing is symptomatic of ◦ ◦ ◦ ◦ A. variant angina B. unstable angina C. non-cardiac related chest pain D. an acute myocardial infarction 8-13 7. Patients who present to the dental office with unstable angina ◦ A. can be treated in the dental office if their vital signs are monitored throughout the appointment ◦ B. can receive emergency dental treatment after consultation with a physician and preferably in a hospital setting ◦ C. can receive a local anesthetic with epinephrine safely ◦ D. can receive a local anesthetic with epinephrine but the maximum dose of the vasoconstrictor should not exceed o.o4 mg. 8-13 7. Patients who present to the dental office with unstable angina ◦ A. can be treated in the dental office if their vital signs are monitored throughout the appointment ◦ B. can receive emergency dental treatment after consultation with a physician and preferably in a hospital setting ◦ C. can receive a local anesthetic with epinephrine safely ◦ D. can receive a local anesthetic with epinephrine but the maximum dose of the vasoconstrictor should not exceed o.o4 mg. 8-13 8. The protocol for management of a patient with no history of angina and who is experiencing anginal-like chest pain includes ◦ A. administering three doses of nitroglycerin over 15 minutes prior to activating the EMS system ◦ B. administering one dose of nitroglycerin and activation of the EMS system if the pain continues for two minutes or longer ◦ C. immediately administering 81 mg of aspirin ◦ D. positioning the patient in a Trandelenburg position because he or she is probably having an anxiety attack. 8-13 8. The protocol for management of a patient with no history of angina and who is experiencing anginal-like chest pain includes ◦ A. administering three doses of nitroglycerin over 15 minutes prior to activating the EMS system ◦ B. administering one dose of nitroglycerin and activation of the EMS system if the pain continues for two minutes or longer ◦ C. immediately administering 81 mg of aspirin ◦ D. positioning the patient in a Trandelenburg position because he or she is probably having an anxiety attack. 8-13 9. During the first one to two hours following the onset of symptoms of an AMI, the greatest risk for death is the development of ◦ ◦ ◦ ◦ A. cardiac dysrhythmias B. dyspnea C. diaphoresis D. pulmonary edema 8-13 9. During the first one to two hours following the onset of symptoms of an AMI, the greatest risk for death is the development of ◦ ◦ ◦ ◦ A. cardiac dysrhythmias B. dyspnea C. diaphoresis D. pulmonary edema 8-13 10. It is recommended that out-of-hospital AMI victims begin fibrinolysis as soon as the symptoms are recognized. The recommended drug is ◦ ◦ ◦ ◦ A. 5 mg of warfarin B. 7 mg of Coumadin C. 162 to 325 mg of acetylsalicylic acid D. 50 mg of aspirin 8-13 10. It is recommended that out-of-hospital AMI victims begin fibrinolysis as soon as the symptoms are recognized. The recommended drug is ◦ ◦ ◦ ◦ A. 5 mg of warfarin B. 7 mg of Coumadin C. 162 to 325 mg of acetylsalicylic acid D. 50 mg of aspirin 8-13 8-13 1. Left ventricular heart failure results in ◦ ◦ ◦ ◦ A. respiratory distress B. peripheral edema C. distended jugular veins while lying or sitting D. nocturia 8-13 1. Left ventricular heart failure results in ◦ ◦ ◦ ◦ A. respiratory distress B. peripheral edema C. distended jugular veins while lying or sitting D. nocturia 8-13 2. All of the following symptoms are observed in late stage heart failure except one. Which symptom is the exception? ◦ ◦ ◦ ◦ A. cyanosis of the lips and/or nail beds B. cardiac cachexia C. mental confusion and anxiety D. stabbing chest pain lasting less than 30 seconds 8-13 2. All of the following symptoms are observed in late stage heart failure except one. Which symptom is the exception? ◦ ◦ ◦ ◦ A. cyanosis of the lips and/or nail beds B. cardiac cachexia C. mental confusion and anxiety D. stabbing chest pain lasting less than 30 seconds 8-13 3. Right ventricular heart failure usually develops before left ventricular heart failure. The major clinical symptom of RV heart failure is pulmonary edema. ◦ ◦ ◦ ◦ A. The 1st statement is true, 2nd is false B. The 1st statement is false, the 2nd true C. Both statements are true D. Both statements are false 8-13 3. Right ventricular heart failure usually develops before left ventricular heart failure. The major clinical symptom of RV heart failure is pulmonary edema. ◦ ◦ ◦ ◦ A. The 1st statement is true, 2nd is false B. The 1st statement is false, the 2nd true C. Both statements are true D. Both statements are false 8-13 4. Symptoms of right heart failure include all of the following except one. Which one is the exception? ◦ ◦ ◦ ◦ A. distended jugular veins B. peripheral edema with pitting C. nocturia D. carpopedal spasms 8-13 4. Symptoms of right heart failure include all of the following except one. Which one is the exception? A. distended jugular veins B. peripheral edema with pitting C. nocturia D. carpopedal spasms 8-13 5. A bloodless phlebotomy ◦ A. should only be performed in a hospital setting on patients suffering from heart failure ◦ B. could be performed in the dental setting to help reduce peripheral edema in heart failure patients ◦ C. could be performed in a dental setting to help manage lung congestion in patients suffering from acute pulmonary edema. ◦ D. is never a treatment option for patients experiencing acute pulmonary edema. 8-13 5. A bloodless phlebotomy ◦ A. should only be performed in a hospital setting on patients suffering from heart failure ◦ B. could be performed in the dental setting to help reduce peripheral edema in heart failure patients ◦ C. could be performed in a dental setting to help manage lung congestion in patients suffering from acute pulmonary edema. ◦ D. is never a treatment option for patients experiencing acute pulmonary edema. 8-13 6. The administration of nitroglycerin is indicated in the management of acute pulmonary edema and heart failure. The administration of nitroglycerin is contraindicated in patients with a systolic pressure lower than 100 mmHg. ◦ ◦ ◦ ◦ A. The 1st statement is true, the 2nd false B. The 1st statement is false, the 2nd true C. Both statements are true D. Both statements are false 8-13 6. The administration of nitroglycerin is indicated in the management of acute pulmonary edema and heart failure. The administration of nitroglycerin is contraindicated in patients with a systolic pressure lower than 100 mmHg. ◦ ◦ ◦ ◦ A. The 1st statement is true, the 2nd false B. The 1st statement is false, the 2nd true C. Both statements are true D. Both statements are false 8-13 7. Prominent jugular veins while seated in an upright position is indicative of ◦ ◦ ◦ ◦ A. left heart failure B. right heart failure C. pulmonary embolism D. acute myocardial infarction 8-13 7. Prominent jugular veins while seated in an upright position is indicative of A. left heart failure B. right heart failure C. pulmonary embolism D. acute myocardial infarction 8-13 8. The most frequent etiology of heart failure is ◦ ◦ ◦ ◦ A. cerebrovascular accident B. diabetes C. myocardial infarction D. cardiac valve abnormalities 8-13 8. The most frequent etiology of heart failure is A. cerebrovascular accident B. diabetes C. myocardial infarction D. cardiac valve abnormalities 8-13 8-13 1. Which of the following should not be used on patients with a pacemaker or ICD? ◦ ◦ ◦ ◦ A. dental handpieces B. composite curing light C. magnetostrictive ultrasonic scaler D. dental radiographs 8-13 1. Which of the following should not be used on patients with a pacemaker or ICD? ◦ ◦ ◦ ◦ A. dental handpieces B. composite curing light C. magnetostrictive ultrasonic scaler D. dental radiographs 8-13 2. The most common use for an implantable cardioverter defibrillator is ◦ ◦ ◦ ◦ A. tachyarrhythmia B. syncope C. severe hypertension D. none of the above 8-13 2. The most common use for an implantable cardioverter defibrillator is ◦ ◦ ◦ ◦ A. tachyarrhythmia B. syncope C. severe hypertension D. none of the above 8-13 3. The portion of the pacemaker that contains the electronic circuitry and powers the device is the ◦ ◦ ◦ ◦ A. lead B. defibrillator C. copper stem D. generator 8-13 3. The portion of the pacemaker that contains the electronic circuitry and powers the device is the ◦ ◦ ◦ ◦ A. lead B. defibrillator C. copper stem D. generator 8-13 4. All of the following are symptoms of an individual suffering from a pacemaker malfunction except one. Which one is the exception? ◦ ◦ ◦ ◦ A. dizziness B. hiccoughing C. swelling of the extremities D. wheezing 8-13 4. All of the following are symptoms of an individual suffering from a pacemaker malfunction except one. Which one is the exception? ◦ ◦ ◦ ◦ A. dizziness B. hiccoughing C. swelling of the extremities D. wheezing 8-13 5. The most important vital sign to monitor on a patient suspected of having a pacemaker malfunction is the ◦ ◦ ◦ ◦ A. pulse B. respiration C. blood pressure D. temperature 8-13 5. The most important vital sign to monitor on a patient suspected of having a pacemaker malfunction is the ◦ ◦ ◦ ◦ A. pulse B. respiration C. blood pressure D. temperature 8-13 6. Local anesthetics with vasoconstrictors should be used with caution on patients with pacemakers and ICDs. ◦ A. True ◦ B. False 8-13 6. Local anesthetics with vasoconstrictors should be used with caution on patients with pacemakers and ICDs. A. True B. False 8-13 7. The factor that causes the greatest risk of malfunction with pacemakers or ICDs is ◦ ◦ ◦ ◦ A. electromagnetic interference B. solar interference C. radiation interference D. sonar interference 8-13 7. The factor that causes the greatest risk of malfunction with pacemakers or ICDs is A. electromagnetic interference B. solar interference C. radiation interference D. sonar interference 8-13 8. The first step in the treatment of suspected pacemaker malfunction is to ◦ ◦ ◦ ◦ A. remove the cause of the interference B. use the AED to regain appropriate heart rate C. administer one table of nitroglycerin sublingually D. contact the manufacturer of the pacemaker for advice. 8-13 8. The first step in the treatment of suspected pacemaker malfunction is to A. remove the cause of the interference B. use the AED to regain appropriate heart rate C. administer one table of nitroglycerin sublingually D. contact the manufacturer of the pacemaker for advice. 8-13