Preparing for Compliance Monitoring Reviews
advertisement

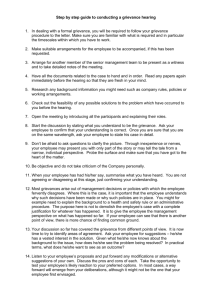
Preparing for Compliance Monitoring Reviews Understanding CMS Protocols Used by Review Organizations January 14, 2009 Presented by: Margaret deHesse, RN, BSN Executive Director, State & Corporate Services Health Services Advisory Group, Inc. Overview of CMS Protocols • Two main sources of information – Document review Assess compliance with regulatory provisions Identify issues that will be pursued during interviews – Interviews Interview participants provide clarification and confirm that documented practices are being followed Data gathered from interviews should supplement and verify what is learned during document review Overview of CMS Protocols Protocol activities 1. 2. 3. 4. 5. 6. 7. Planning for compliance monitoring activities Obtaining background information from the State Medicaid agency (review organization’s responsibility) Document review Conducting interviews Collecting any other accessory information (e.g., from site visits) Analyzing and compiling findings (review organization’s responsibility) Reporting results to the State Medicaid agency (review organization’s responsibility) Activity 1: Planning for Compliance Monitoring Activities • Establishing an agenda for the visit − In conjunction with the review organization. − An agenda will help the review organization to perform an efficient and effective on-site evaluation. − An agenda will help the MCO/PIHP to: Plan for staff participation. Gather documentation. Address logistical issues, such as arranging locations for reviewers to conduct document review, system demonstrations, observations, and interviews. Activity 1: Planning for Compliance Monitoring Activities (cont.) • Establishing an agenda for the visit (cont.) − An agenda sets the tone, as well as the expectations, for the on-site visit so that both the MCO/PIHP and the reviewers understand the objectives and time frames for the review. − Review the agenda at the end of each review day to verify follow-up items and the next day’s events. Activity 1: Planning for Compliance Monitoring Activities (cont.) • Preparation instructions and guidance are provided to the MCO/PIHP by the review organization – An on-site evaluation process requires the cooperation of the MCO/PIHP being evaluated. – If the MCO/PIHP is prepared for the on-site visit, reviewers can remain focused on conducting and completing the evaluation in the allotted time frame. Activity 1: Planning for Compliance Monitoring Activities (cont.) • Preparation instructions and guidance are provided to the MCO/PIHP by the review organization (cont.) – Review organization instructions may include the following: Providing the health plan with the on-site review tool, which describes the scope of the evaluation to be performed Describing how the evaluation will be conducted, including instructions Providing a list of documents that should be available Activity 1: Planning for Compliance Monitoring Activities (cont.) • Preparation instructions and guidance are provided to the MCO/PIHP by the review organization (cont.) – Health plan responsibilities may include the following: Preparing a roadmap (description of how documents, systems, and processes meet the standard). Organizing the files to be reviewed. Verifying that the correct files are prepared (compare to sample list, check names, documents in files, mock file review). Activity 1: Planning for Compliance Monitoring Activities (cont.) • Preparation instructions and guidance are provided to the MCO/PIHP by the review organization (cont.) – Health plan responsibilities may include the following: Completing any forms or other data-gathering instruments (e.g., an Information Systems Capability Assessment). Arranging expected participant interviews. Making administrative arrangements. Confirming other expectations or responsibilities. Examples of Successful Preparation Activities • Create a work team with significant involvement of operational areas being reviewed – Member services, information services, quality, compliance, utilization management, case management, provider relations, etc. • Create a formal work plan based on the review schedule established in conjunction with the State • Conduct a mock review using the review tool to identify gaps prior to the on-site review • Prepare information files or binders coinciding with each area under review Activity 2: Document Review • Consider all sources of compliance requirements – Assessment of compliance with regulatory provisions Medicaid regulatory provisions (BBA) State contract requirements Internal policies and procedures Activity 2: Document Review (cont.) • Consider all sources of compliance requirements (cont.) – Identified issues that will be pursued during interviews Disagreement between internal policies and procedures and State and federal requirements Activity 3: Interviews • Consider the topic and policy/procedure when scheduling participants – Data gathered from interviews should supplement and verify what is learned during document review. – Interview participants provide clarification and confirm that documented practices are being followed. Interviews should be conducted with groups. Rarely is one individual solely responsible for a particular function. Cross-functional/service/department interviews are beneficial. What one area does not know, another may, and the interview then becomes a learning opportunity for the MCO’s/PIHP’s staff as well. Example: Grievance Process Review Activity 1: Planning • Review organization instructions may include the following: – The scope of the evaluation to be performed All grievances in a time frame (between 1/1/2008 and 12/31/2008) – How the evaluation may be conducted Review of documentation and reports (pre-on-site and on-site) System demonstration o Databases—including codes/types of grievances o Manual—paper-based system Interviews o Staff members who are interviewed should be prepared to describe their role in the grievance process, including intake, routing, and oversight. Observations File review of selected sample of grievances Example: Grievance Process Review Activity 2: Document review • Review organization instructions may include the following: − Documents that may be requested for review prior to onsite review or while on-site Grievance and appeals policies and procedures Internal monitoring reports o Reports used to monitor timeliness o Reports used to trend types and subtypes of grievances External regulatory reports Sample acknowledgement letters Sample resolution letters Example: Grievance Process Review Activity 2: Document review (cont.) • Review organization instructions may include the following: – Grievance file review by review organization Random sample of grievance files to review Size of sample determined by review organization The health plan will then compile documentation with each grievance in a separate labeled file folder – Completion of any forms or other data-gathering instruments Health plan description of the system used to handle grievances Systems may include database and manual/paper process. How information is provided to other departments or committees Example: Grievance Process Review Activity 3: Interviews • Review organization instructions may include the following: − Administrative arrangements Need for review team meeting room including interviews − Expected interview participants Supervisory staff members responsible for oversight of staff handling incoming grievances Member services observation Quality or compliance staff members responsible for oversight of process Example: Grievance Process Review (cont.) Activity 3: Interviews (cont.) • Sample interview questions – Which staff members are responsible for helping Medicaid members use the organization’s complaint or grievance system, including completing forms, or taking other steps to resolve an appeal or grievance? – What kind of assistance is made available to Medicaid members? – Describe your role in the process, including documentation you prepare. – Who is responsible for routing grievances to the appropriate department or staff member for resolution? Example: Grievance Process Review Activity 3: Interviews (cont.) • Sample interview questions – Do you get feedback regarding ways you could improve your process? – Is there a process in place to monitor either the appeal and grievance process or the areas of concern identified by member appeals and grievances? – Describe reports used for monitoring. Example: Grievance Process Review Activity 4: Collecting any other accessory information (e.g., from site visits) • Other expectations or responsibilities – Additional information may need to be copied to validate health plan activities – Observations and walk-through for key operations areas such as member services call center Wrap Up • Questions?