Lipid Metabolism
advertisement

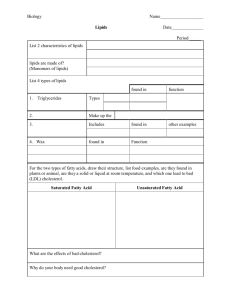
Lipid Metabolism Digestion and Absorption of Dietary Lipids • Lipids are taken in the diet mainly as triacylglycerol •. In addition, small amounts of phospholipids, cholesterol, carotenoids and fat-soluble vitamins are taken in diet. I- Digestion of Triacylglycerol • 1- Lingual lipase • 2- Gastric lipase • 3- Pancreatic lipase, is the main digestive lipase. Emulsification of lipids is important for the action of pancreatic lipase. Emulsification involves mixing in the duodenum with bile salts, phospholipids and lysophospholipids in addition to monoacylglycerol. This leads to breaking of lipid droplets into smallersized structures, which increases their surface area exposed to enzyme. I- Digestion of Triacylglycerol • The products of digestion by pancreatic lipase are: • 72% as 2-monoacylglycerol (MAG) • 22% as glycerol and free fatty acids • 6% as 1-monacylglycerol • 4- Intestinal lipase: This intracellular enzyme hydrolyzes 1-monoacylglycerol to glycerol and free fatty acid. II- Digestion of Phospholipids III-Cholesterol esters • II- Digestion of Phospholipids • Phospholipids may be absorbed without digestion. Also they may be hydrolyzed by pancreatic phospholipase A2 to lysophospholipids. The resulting lysophospholipids act as emulsifying agents. • III- Digestion of cholesteryl ester • Cholesteryl ester is hydrolyzed by pancreatic cholesterol esterase (cholesteryl ester hydrolase) into cholesterol and fatty acid. Digestion of Dietary Lipids FA1 H2O FA1 FA3 FA2 FA2 FA2 FA3 Pancreatic lipase Pancreatic lipase OH OH 2- MAG (72%) 1,2- DAG TAG OH FA1 H2O Isomerase FA1 H2O OH HO HO Pancreatic lipase OH Glycerol (22%) FA1 H2O FA2 FA1 HO FA2 Pancreatic Phospholipase A2 P – Base P – Base Lysophospholipids Phospholipids H2O FA1 FFA Cholesterol Cholesteryl esters Cholesterol esterase OH 1- MAG (6%) Absorption of Dietary Lipids • Bile salts together with products of digestion form micelles. These micelles are soluble thus allowing the products of digestion, together with fat-soluble vitamins to be transported to the brush border of the mucosal cells to be taken to the inside of the epithelial cells. Bile salts pass to the ileum, where most are reabsorbed into the enterohepatic circulation. Diagram for Digestion and Absorption of Lipids Intestinal Lumen Mucosal Cells TAG Chylomicrons Pancreatic lipase Lacteals FFA Phospholipids Free cholesterol Cholesterol-esters ApoA, B-48 DAG Pancreatic lipase FFA FFA 2-MAG TAG 2-MAG Thiokinase Acyl- CoA CoA , ATP Isomerase Glycerol kinase FFA 1-MAG 1-MAG ATP Intestinal lipase Pancreatic lipase Glycerol 3-P Glycerol Glycolysis FFA Glycerol Glucose DHAP Glycerol Portal blood Chylomicron Structure A Apo A Free cholesterol Cholesteryl-ester Phospholipids B-48 TAG Apo B-48 The formed triacylglycerol with cholesteryl ester (hydrophobic core) are surrounded by a single layer of phospholipid and cholesterol together with proteins (apo A and apo B-48) to form minute particles < 1μm called chylomicrons within the mucosal cells which are transported to the lymphatics (lacteals). Fate of Absorbed Lipids • I- Uptake by tissues • About 90% of triacylglycerol in the chylomicrons are hydrolyzed by the enzyme lipoprotein lipase This enzyme is present in the endothelial cells of extrahepatic tissue (muscle and adipose tissue). Its synthesis is increased by insulin. • Heparin stimulates the release of lipoprotein lipase thus clearing plasma turbidity due to the absorbed chylomicrons, thus heparin is called a clearing factor. • Hydrolysis of the triacylglycerol yields free fatty acids (FFAs) and glycerol. Most of the FFAs are taken by the extrahepatic tissue. • The released glycerol is taken by the liver and the kidney where it can be utilized by the glycerol kinase in these tissues. Fate of Absorbed Lipids • II-Utilization by tissues • 1- Oxidation: Fatty acids are mostly oxidized by β-oxidation. Glycerol is oxidized by joining the glycolysis pathway. • 2- Conversion to glucose: glycerol (10% of fats) can be converted to glucose. The last 3 carbons of odd chain fatty acids (which are rare in natural fat) may also be converted to glucose. • 3- Formation of tissue fat. • III-Storage • This occurs mainly in the adipose tissue as triacylglycerol (DEPOT FAT). • IV-Excretion • Fats may be secreted in sebaceous glands and also by mammary gland in milk. Compare between: • Tissue fat: • Depot fat: • Constant element (not • Variable element affected by diet) (affected by diet) • Consists mainly of : Phospholipids, glycolipids. • Consists mainly of TAG • Site: cell membrane, mitochondrial membrane and nervous tissue. • • • • • Functions: 1- membrane permeability 2- ETC 3- Nerve impulse transmission 4- tissue support and protection • Site: Adipose tissue • Function: Source of energy Oxidation of Fatty Acids • Free fatty acids are taken by most of the tissues. Oxidation of the fatty acids is principally by β- oxidation in the mitochondrial matrix (adjacent to the TCA cycle and the respiratory chain). • In the mitochondria, fatty acids are oxidized to acetyl-CoA. Acetyl-CoA may be further oxidized completely in the TCA cycle. Activation of the fatty acid • is catalyzed by acyl-CoA synthetase (key enzyme). This step requires ATP and so it is irreversible Acyl- CoA synthetase R – CO ~ S – CoA R – COOH FFA Acyl- CoA CoA-SH ATP PPi + AMP 2Pi Transport of acylCoA into the mitochondria • Long chain fatty acyl-CoA : They are transported to the mitochondrial matrix by carnitine shuttle Transport of Acyl-CoA into Mitochondria (Carnitine Shuttle) FFA Cytosol Outer membrane CoA-SH Acyl-CoA CoA-SH ATP Carnitine-palmitoyl transferase I Acyl-CoA synthetase Inter-membrane space Carnitine Acyl-carnitine Carnitine Acyl-carnitine translocase Inner membrane Carnitine-palmitoyl transferase II Mitochondrial matrix Carnitine Acyl-CoA CoA-SH Acyl-carnitine -oxidation of Acyl-CoA O R – CH2 CH2 – C ~ S – Co A Acyl-CoA ( Cn ) Acyl- CoA dehydrogenase ETC 2 ADP + 2 Pi [O] + FADH2 O R – CH 2 ATP H2O + FAD CH – C ~ S – Co A 2– Trans- enoyl-CoA Repeat The Cycle H2O 2– Trans-enoyl-CoA hydratase OH R – CH O CH2 – C ~ S – Co A L,3- Hydroxyacyl-CoA H2O + NAD+ L,3- Hydroxyacyl-CoA dehydrogenase NADH,H+ O 3 ATP ETC [O] + 3 ADP + 3 Pi O R – C ~ CH2 – C ~ S – Co A 3- Ketoacyl-CoA CoA-SH -Ketothiolase O O R– C ~ S – CoA Acyl- CoA (Cn-2 ) CH3– C ~ S – CoA Acetyl- CoA Citric Acid Cycle & ETC 2CO2 + 12 ATP Energy yield • Energy yield: Oxidation of palmitic acid (C16) results in the formation of 8 molecules of acetyl-CoA through passing through 7 cycles. • Each cycle yields one molecule of NADH and one molecule of FADH2.These reduced coenzymes will yield 5 ATPs via the respiratory chain. So in 7 cycles: 7 X5 =35 ATPs are produced. The 8 molecules of acetyl CoA will produce 8 X 12=96 ATPs by oxidation in Krebs’ cycle and ETC. • Thus a total of 35 + 96 = 131 ATPs are produced from complete oxidation of one molecule of palmitic acid. Since 2 high energy phosphates are used in the activation of the fatty acid, so the net gain is 131-2= 129 ATPs • ATP Produced by Oxidation of Palmitic Acid CH3(CH2)14-CO ~ S –CoA Palmitoyl-CoA 7 Cycles of β-oxidation 7 FADH2 + 7 NADH,H+ + 8 Active acetate ETC TCA cycle & ETC ETC 16 CO2 14 ATP + 21 ATP + 96 ATP = 131 - 2 for activation = 129 ATP N.B : Oxidation of odd chain fatty acids leaves the last 3 carbons as propionyl-CoA. Propionyl-CoA is carboxylated to methylmalonyl-CoA which is isomerized to succinyl-CoA which enters Krebs’ cycle. • Regulation of β-Oxidation • It depends upon the availability of fatty acids and the consumption of ATP. • 1-Availability of fatty acids: Carbohydrate feeding leads to release of insulin. Insulin stimulates lipogenesis and inhibits lipolysis thus decreasing FFA. • Also during carbohydrate feeding, synthesis of fatty acids is stimulated and so, excess malonyl-CoA is formed. MalonylCoA inhibits CPT-I thus inhibiting the uptake and oxidation of the fatty acids. Thus the 2 processes, synthesis and oxidation do not go together. • 2- β-oxidation in a cell depends upon its consumption of ATP. High ATP (and low ADP& Pi) inhibits the respiratory chain, thus β- oxidation becomes inhibited. Regulation of Fatty Acid β-Oxidation Fatty acids ATP/ADP _ Fatty acyl-CoA Electron transport chain CPT I _ Fatty acyl-carnitine NADH & FADH2 _ β-Oxidation Acetyl-CoA Malonyl-CoA Acetyl-CoA Carboxylase + Insulin Acetyl-CoA Compound Lipids Phospholipids Glycerophospholipids - Phosphatidic acid - Phosphatidylcholine (lecithin) - Phsphatudylethanolamine -Phosphatidylinositol Sphingolipids Sphingophospholipids - Sphingomyelin Glycolipids - Cerebrosides - Sulfatides - Globosides - Gangliosides Metabolism of Ketone Bodies • Ketogenesis • Ketone bodies are acetoacetate, βhydroxybutyrate and acetone. Synthesis of ketone bodies occurs in the mitochondria of the liver. This is because of the presence of HMG-CoA synthase and HMG-CoA lyase chiefly in the liver. The building unit of ketone bodies is acetyl-CoA derived mainly from oxidation of fatty acids. Diagram for Ketogenesis CH3- CO ~ S – CoA Acetyl-CoA Acyl- CoA -Oxidation -Oxidation Last C4 Ketogenic Amino acids Ketothiolase CoA-SH Acetoacetyl-CoA HMG-CoA Synthase H2O (Liver mitochondria) Acetyl-CoA CoA-SH 3-Hydroxy-3-methyl glutaryl-CoA (HMG-CoA) HMG-CoA Lyase (Liver mitochondria) CH3- CO ~ S – CoA Acetyl-CoA Acetoacetate Spontaneous (Lungs & Kidneys) CO2 Acetone (Expired air & Urine) NADH,H+ 3- hydroxybutyrate Dehydrogenase NAD+ 3- Hydroxybutyrate • Importance of Ketogenesis • Ketogenesis is of great importance during starvation when fats represents the main source of energy. Although most tissues can utilize fatty acids, they can utilize ketone bodies more easily. During prolonged fasting, the brain adapt to utilize ketone bodies as it cannot utilize fatty acids (fatty acids are bound to plasma albumin and cannot pass the blood brain barrier). Thus ketogenesis is a preparatory step by the liver to facilitate the oxidation of fatty acids during starvation and to provide energy for extrahepatic tissues including the brain. Ketolysis • It is the complete oxidation of ketone bodies in the mitochondria of extrahepatic tissue. This is due to the high activity of thiophorase (succinyl-CoA:acetoacetate CoA transferase) in the extrahepatic tissue and its deficiency in the liver. β–hydroxybutyrate is converted to acetoacetate, which gives two molecules of acetyl-CoA. Acetyl-CoA is utilized by Krebs’ cycle for complete oxidation. • Ketolysis is dependent on activity of citric acid cycle as succinyl-CoA needed for the thiophorase reaction is supplied from citric acid cycle and acetyl-CoA enters the cycle for complete oxidation. Diagram for Ketolysis CH3-CHOH-CH2-COOH 3- hydroxybutyrate NAD+ 3- hydroxybutyrate Dehydrogenase NADH,H+ Succinyl-CoA CH3-CO~CH2-COOH Acetoacetate CoA Transferase Mitochondria of extrahepatic tissues Citric acid cycle Acetoacetyl-CoA CH3-CO~CH2-CO ~ S - CoA Citrate Succinate Ketothiolase CoA-SH Oxaloacetate 2 CH3-CO ~ S - CoA Acetyl-CoA Ketosis • This is a condition characterized by increased ketone bodies in the blood (ketonemia) and in the urine (ketonuria). • Normally ketone bodies in blood ranges from 0.5-3mg/dL. In urine, it is less than 15mg/day. • Causes of Ketosis • Ketosis occurs in conditions where the rate of ketogenesis exceeds the rate of ketolysis i.e. in conditions where there is marked stimulation of ketogenesis, as in the following: • -Starvation, low carbohydrates and high fat in diet • -Severe diabetes mellitus • -Prolonged administration of anti-insulin hormones • -Prolonged and severe muscular exercise • Effects of ketosis • The increased production and loss of βhydroxybutyrate and acetoacetate leads to excessive loss of buffer cations Na+, K+ and NH4+ in urine associated with decreased bicarbonate in the blood, which causes acidosis and may lead to coma and death. • Ketogenic substances include fatty acids, ketogenic amino acids and anti-insulin hormones • Anti-ketogenic substances include carbohydrates, glucogenic amino acids, glycerol and insulin. • Diagram for Metabolic Changes Adipose Tissue During Ketosis TAG Increased of Antiinsulin / Insulin ratio in Blood Activation of Lipolysis Brain Oxidation for energy production Glycerol FFA Glucose Glucose Glucose BLOOD Glycerol Ketone bodies Oxidation for energy production FFA Gluconeogenesis Ketogenesis - Pyruvate - Lactate Ketone bodies - Oxaloacetate - Glucogenic amino acids Liver Ketogenic Amino acids Acetyl-CoA ketolysis Ketone bodies In Urine (ketonuria) Ketone bodies Extrahepatic Tissues (muscles) Metabolism of Cholesterol • Biosynthesis of Cholesterol • It is synthesized in the cytosol and endoplasmic reticulum in all nucleated cells. Plasma cholesterol is made in the liver and intestine. Acetyl-CoA is the source of all cholesterol carbons. • Cholesterol synthesis starts by the formation of HMGCoA in the same way as in ketogenesis except that it is in the cytosol (ketogenesis occurs in mitochondria). • HMG-CoA is reduced to mevalonate in a reaction catalyzed by HMG-CoA reductase (Key enzyme) and requiring two NADPH. Importance of Cholesterol • 1-Formation of lipoproteins: Cholesterol regulates membrane fluidity. • 2-Synthesis of vitamin D3: Cholesterol is dehydrogenated, forming 7dehydrocholesterol. The latter is converted into vitamin D3 under the skin by ultra-violet rays. • 3-Formation of steroid hormones: Cholesterol is the precursor of all steroid hormones, androgens, estrogens, progesterone, and corticoids. Importance of Cholesterol • 4-Formation of bile acids and salts: Primary bile acids, are synthesized from cholesterol in the liver. Subsequently; these acids are conjugated with glycine or taurine to form (bile salts) • Bile salts are important for emulsification of fats, thus important for digestion and absorption of fats. • Intestinal bacteria deconjugate and dehydroxylate the primary bile acids converting them into secondary bile acid. • Excretion of Cholesterol • About 50% of cholesterol is excreted in feces as bile acids; the remaining 50% are excreted also in stools as neutral sterol (coprostanol). • Plasma Cholesterol • The total plasma cholesterol level ranges from 120-240 mg/dL (recommended level is less than 200 mg/dL). About two thirds are present as cholesteryl ester and one third is present as free cholesterol. Hypercholesterolemia • Hypercholesterolemia means a plasma cholesterol level higher than 240 mg/dL. There are some factors which may lead to it, these include: • 1-Dietary causes: Diet rich in saturated fat, carbohydrates and cholesterol. • 2- Obesity • 3-Diabetes mellitus • 4-Hypothyroidism: as thyroid hormone stimulates the oxidation of cholesterol and its conversion to bile acids. • 5-Obstructive jaundice: This blocks the pathway for excretion of cholesterol and bile acids. • 6-Nephrosis: • 7-Familial hyperliopoproteinemias Plasma Lipids and Lipoproteins • Lipids are transported as lipoproteins with special arrangement, so that the most hydrophobic one is present in the core (triacylglycerol and cholesterol-esters).These are surrounded by the amphipathic lipids (phospholipids and cholesterol) and apolipoproteins. • Types of plasma lipoproteins: • 1- Chylomicrons: Synthesized in intestinal cells and consist mainly of TAG. • 2- Very Low Density Lipoprotein (VLDL): synthesized in liver and consist mainly of TAG. • 3- Low Density Lipoprotein (LDL): synthesized in liver and consist mainly of cholesterol. LDLs are important source of cholesterol to extrahepatic tissues. High levels of LDLcholesterol increase the risk of atherosclerosis. • 4- High Density Lipoprotein (HDL): synthesized in extrahepatic tissues and consist mainly of phospholipids HDLs are important for removal of cholesterol from the tissues to the liver (reverse cholesterol transport) and high levels of HDL protect against atherosclerosis.