Foot & Ankle - 02 - National MSK & Ortho
advertisement

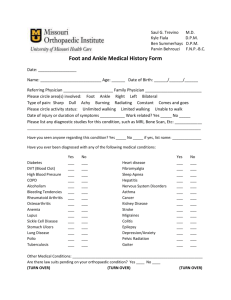
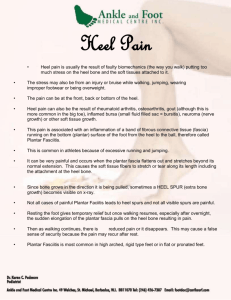
National Foot & Ankle Event June 2015 Kate James – MSK & Orthopaedic Quality Drive - National Lead National Support • • • • • MSK & Orthopaedic Quality Drive – Year Two Dashboard & Indicators Peer Review National Foot & Ankle Pathway - Draft Available Intelligence: – Activity Data – Audit Results ghdfjhsdgfjh Ghdfjhsdgfjh Ghdfjhsdgfjh ghdfjhsdgfjh Peer Review • Chief Exec Letter – Next week • Visit to each hospital – Supported by Indictor Summary – Sept to Dec 2015 • Senior Scottish & Senior English Ortho Surgeon, myself and two ‘peers’ • ‘Pool of Peers’ – Clinicians & Managers from around Scotland each contributing at 2-3 reviews • Attendees: Senior Managers, Senior Clinicians, Workstrand Leads • Pump-Prime Funding (non-recurring) – Funding Request via Board Exec Leads - make a difference to achieving sustainable change in priority focus areas Peer Review • Chief Exec Letter – The focus of the Trauma & Orthopaedic ACCESS programme is on: • embedding the gains for patients of the four ‘pathway’ workstrands in the MSK and Orthopaedic Quality Drive. Progress in AHP MSK Redesign, Non-operative Fracture Redesign, Elective Enhanced Recovery and the Hip Fracture Care Pathway can be evidenced via the clinical quality and efficiency indicators in the 'Rolling Audit'. • maintaining the significant momentum of change, evidenced by the strength of multidisciplinary clinical and managerial teams at the majority of Scottish hospitals and demonstrable gains from the Quality Drive. • optimising use of existing trauma and elective capacity – workforce, beds, and theatres. • demand and capacity planning and management to understand which elements of each Board/Hospital’s service are in balance and which are out of balance. Musculoskeletal – Foot and Ankle - Management and Referral Pathway – July 2013 Patient Presentation Hallux Valgus & Rigidus (Bunions) • Swelling or deformity at 1st MTP joint • Hallux Rigidus due to OA – swelling due to osteophytes. Reduced range of movement and pain on activity • Hallux Valgus due to lateral deviation of hallus – Pain over medial prominence, exacerbated by tight shoes. May develop secondary callous, corns, ulcers or toe deformities Mortons Neuroma / Metatarsalgia • Pain under lesser metatarsal heads or in webspaces • Painful paraesthesia or plantar callosites • Pain on activity Midfoot Arthritis / Tibialis Posterior Rupture • Pain and stiffness • Local tenderness • Loss of medial longitudinal arch GP/AHP Assessment Provide advice on – • footwear (e.g. extra width and low heals) • rest of feet after periods of standing/walking • exercise for ankles and stretch of Achilles Tendon if appropriate • weight-loss if appropriate • analgesia & NSAIDS as appropriate • Consider Podiatry/ Orthotic referral • Website for selfhelp – http://www.nhsinf orm.co.uk/MSK/lo werbody Remember Diabetic Foot and refer early to avoid amputation (to specialist clinic where service exists) Any further guidance from BOFAS to include? Primary Care • Any indications for diagnostic tests from Primary care? How do we make it clear who should be referred to Podiatry / orthotics? • Podiatry and Orthotics • • • • Advice re footwear Provide specialist footwear, insoles, orthotics Care of secondary lesions Intra-articular steroid injections • • If No Improvement after 3 months provide information sheet on surgical options and discuss. Do we have this? If patient considering surgery, refer to secondary care Orthopaedic Foot & Ankle Clinic Include information on conservative treatment tried (any to rheumatology?) Produced by Scottish Orthopaedic Services Development Group With advice from primary and secondary care clinicians Secondary Care Indications for surgery Failure of conservative treatment for at least 3 Months. Hallux Valgus and Rigidus Pain should be primary indication for Surgery. Recurrent ulcers and Infection. Metatarsalgia Fixed toe Deformities. Morton’s Neuroma Not responded to steroid injections. Refer for ultrasound examination Midfoot Arthritis Tibialis Posterior Rupture Consider surgical fusion Page 1 of 3 Any further guidance from BOFAS to include? Musculoskeletal – Foot and Ankle - Management & Referral Pathway – June• 2013 • Patient Presentation Posterior Heel Pain Pump bumps • GP/AHP Assessment • • • Tenderness and swelling proximal to insertion of tendon to posterior calcaneum Plantar Heel Pain Plantar Pad • • • Fat pad atrophy with non-specific pain under heel • Plantar Heel Pain Plantar Fasciitis • • • Primary Care • Prominent posterior aspect of calcaneum Posterior Heel Pain Achilles Tendonosis • Simple padding and footwear advice Pain is worse on taking first steps in the morning Tenderness at attachment of Plantar Fascia to medical calcaneal tubercle (illustrated) Spurs are not significant • • If No Improvement after 3 months provide information sheet on surgical options and discuss. Do we have this? Advise a 1cm heel raise Reduce mileage and frequency of exercise Consider Physio referral • • Include information on conservative treatment tried Consider Podiatry/Orthotics referral for Orthoses • (any to rheumatology?) Regular calf/ plantar fascia stretching Consider Podiatry/Orthotics referral for Orthoses, Steroid injection, Night splints As spurs are not significant X-Rays are not indicated Remember Diabetic Foot and refer early to avoid amputation (to specialist clinic where service exists) Indications for diagnostic tests from Primary care? If patient considering surgery, refer to secondary care Orthopaedic Foot & Ankle Clinic General advice • Advise analgesia and NSAIDs as appropriate • Advise patient that weight loss can reduce heel pain • Minimise impact on feet by wearing footwear with padding or shock absorbing material • Website for self-help http://www.nhsinfor m.co.uk/MSK/lower body Secondary Care Indications for Surgery Failure of conservative treatment for at least 3 Months. Posterior Heel Pain Pump bumps • possible surgical excision of bursa Posterior Heel Pain - Achilles Tendonosis • Possible decompression of Achilles tendon Plantar Heel Pain - Plantar Pad • Surgery rarely indicated Plantar Heel Pain - Plantar Fasciitis • 80% resolve within 12-18 months • Surgery is rarely indicated Produced by Scottish Orthopaedic Services Development Group With advice from primary and secondary care clinicians Page 2 of 3 Musculoskeletal – Foot and Ankle - Management and Referral Pathway – July 2013 Patient Presentation GP / AHP Assessment • Lateral ankle sprains Lateral ankle pain, swelling and giving way • • Ankle and hindfoot disorders Pain stiffness or deformity in hindfoot. Can be caused by arthiritis, tendon rupture, neurological imbalance, diabetic neuroarthropathy • • • • • Cavus feet? Flat feet? Ingrowing toenail? Secondary Care Indications for surgery Acute injury – protection, rest, ice, compression, elevation (PRICE) X-ray if fracture suspected Consider referral for Physiotherapy Advise that weight loss can reduce pain Standing x-rays of ankle and foot: If normal (no deformity/minimal arthritis) consider referral to Podiatry/Orthotics If severe OA or deformity, refer to Orthopaedics If Rheumatoid arthritis refer to Rheumatology Remember Diabetic Foot and refer early to avoid amputation (to specialist clinic where service exists) Primary Care • If No Improvement after 3 months provide information sheet on surgical options and discuss. Do we have this? • If patient considering surgery, refer to secondary care Orthopaedic Foot & Ankle Clinic • Include information on conservative treatment tried Lateral ankle sprains • No indication for surgery after acute ligament injuries • Chronic pain and instability need further imaging and may require surgical reconstruction Ankle and hindfoot disorders • Consider surgery if… General advice • Analgesia and NSAIDs as appropriate • High heel shoes can cause strain on ankles and Achilles tendon • Advise to wear ankle supports when playing sport • Website for self-help http://www.nhsinfor m.co.uk/MSK/lower body Produced by Scottish Orthopaedic Services Development Group With advice from primary and secondary care clinicians Page 3 of 3 Activity Data Audit Slides




![[ ] RESEARCH REPORT](http://s2.studylib.net/store/data/010810863_1-203ff63daf5df20f3208187cecba39c6-300x300.png)