Pediatric Anatomy and Physiology
advertisement

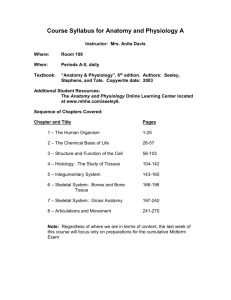
Pediatric Anatomy and Physiology Gerard T. Hogan, Jr., CRNA, MSN Clinical Assistant Professor Anesthesiology Nursing Program Florida International University Pediatric Anatomy/Physiology The physiologic appearance of a newborn contrasts sharply with that of a toddler and even more so with that of a school-age child You must understand these differences and appreciate them to properly assess, plan, and deliver an anesthetic Pediatric Anatomy/Physiology Physical appearance Most dramatic difference is physical size BSA can be computed using nomogram Head is large compared to the adult Often in newborns it exceeds the circumference of the chest Arms and legs are shorted and underdeveloped at birth Midpoint in length on child is umbilicus Midpoint in length on an adult is the symphysis pubis Pediatric Anatomy/Physiology Frequently because there is a large difference in the proportions of body parts, providers use a BSA chart for drug dosages Pediatric Anatomy/Physiology Musculoskeletal system Bone growth occurs at different rates throughout the body This affects anatomical landmarks In the neonate, the imaginary line joining the iliac crests occurs at S1 Sacrum is not fused normally at birth At birth spinal column has only the anterior curvature Cervical and lumbar curvature begin with holding head up and walking Pediatric Anatomy/Physiology Central Nervous System The brain at birth is 1/10 the body weight Only ¼ of the neuronal cells that exist in adults are present in the newborn Neuronal development finishes as age 12 Myelination is not complete until age 3 Primitive reflexes (Moro, grasp) disappear with myelination Pediatric Anatomy/Physiology Central Nervous System Autonomic nervous system is developed at birth, though immature Parasympathetic system is intact and fully functional Lower end of the cord is at L3 at birth Receeds to L1 by 1 year of age Dural sac shortens from S3 to S1 by 1 y/o Pediatric Anatomy/Physiology Cardiovascular System Many profound changes after birth SVR doubles after first breath Pulmonary vasculature dilates, decreasing PVR Foramen ovale closes as left atrial pressure becomes higher than right atrial pressure Flow reverses in the ductus arteriosis, preventing flow between the pulmonary artery and the aorta Pediatric Anatomy/Physiology Cardiovascular system The reason for closure is not fully understood Umbilical vein flow ceases at birth Muscular contraction shuts off the ductus venosus, and portal venous pressure rises, directing flow through the liver Persistent fetal circulation may require surgical intervention Pediatric Anatomy/Physiology Cardiovascular system Persistent fetal circulation Hypercarbia, hypoxia, and acidosis can precipitate pulmonary vasoconstriction If RA pressure exceeds LA pressure, the foramen ovale can open, and exacerbate the shunt If the ductus arteriosus fails to close, a right to left shunt may continue Pediatric Anatomy/Physiology Pediatric Anatomy/Physiology Myocardium Stroke volume of an infant is relatively fixed “they live for (or better yet, by) heart rate” Myocardium is relatively stiff Increasing preload will not increase CO Cardiac reserve is limited Small changes in end diastolic volume yield large changes in end diastolic pressure Pediatric Anatomy/Physiology Myocardium To increase CO, you must increase HR Infants (and prepubescent children, for that matter) are predisposed to bradycardia (“Vagus with legs”) Parasympathetic cardiac innervation is completely developed (and ready for stress) at birth Sympathetic innervation is sparse, but functional Pediatric Anatomy/Physiology Unbalanced parasympathetic tone can manifest in negative inotropy, predisposing them to CHF Heart rate in infants is higher and decreases gradually over the first 5 years of life to near adult levels Pediatric Anatomy/Physiology Pediatric Anatomy/Physiology Respiratory System Pediatric airway Head is large and neck is short Occiput predominates Supine, the chin meets the chest Tongue is large and occupies entire oropharynx Absence of teeth further predisposes the infant to airway obstruction Pediatric Anatomy/Physiology Respiratory System Pediatric airway Obligate nose breathers because of the close proximity of the epiglottis to the soft palate Mouth breathing occurs only during crying Obligate nose breathing is vital for respiration during feeding Pediatric Anatomy/Physiology Respiratory System Pediatric airway The pharynx is almost completely soft tissue It is easily collapsed by posterior displacement of the mandible, or external compression of the hyoid The pharyngeal lumen may collapse with negative pressure generated through inspiratory effort, particularly when the muscles that maintain airway structure are depressed or paralyzed Pediatric Anatomy/Physiology Respiratory System Pediatric airway Larynx Funnel shaped, as opposed to adult cylindrical shape More cephalad in location as compared to an adult In adults, the larynx lies at the level of C 4-6, but in infants, it is 2 vertebral levels higher Cricoid ring is complete, and is the narrowest point of the pediatric airway Pediatric Anatomy/Physiology Respiratory System Pediatric airway Larynx Because the cricoid ring is the narrowest part of the airway, traumatizing it with multiple intubation attempts may lead to swelling and obstruction Epiglottis is short and narrow, and cords are angled Pediatric Anatomy/Physiology Respiratory System Pediatric airway Anatomical differences in the thorax Chest wall is very compliant Ribs are horizontally located, limiting inspiration Diaphragm is deficient in type 1 muscle cells These cells are required for continuous, repeated exercise activities Pediatric Anatomy/Physiology Respiratory System Pediatric airway Lungs Maturation not complete until age 8 Alveoli grow and increase in number to age 8 Surfactant production begins at 20 weeks, but really increases between 30-34 weeks Breathing movements begin in utero, to prepare for the big event Bu 36 weeks, regular breathing movements of 70/min are noted Pediatric Anatomy/Physiology Respiratory System Pediatric airway High metabolic rate necessitates high respiratory rate Pulmonary parameters vastly different Pediatric Anatomy/Physiology Respiratory System Pediatric airway FRC is relatively close to adult No where near as effective based on metabolic rate, O2 consumption, and high degree of alveolar ventilation Infants initially hyperventilate in response to hypoxia, but will not sustain and begin to slow down their breathing Pediatric Anatomy/Physiology Respiratory System Pediatric airway Infants increase their respiratory rate in the presence of hypercarbia Not as much as adults because chemoreceptors are immature Periodic breathing occurs in 78% of infants, usually during quiet sleep Hemoglobin level is around 19g/dl, most is HbF, which has a greater affinity for O2 Pediatric Anatomy/Physiology Respiratory System Pediatric airway Oxygen is bound more tightly to HbF, so cyanosis occurs at a lower PO2 than in the adult O2 tissue delivery is not as good as adult due to HbF’s poor reactivity to 2,3-DPG Normal PO2 in the newborn is 60-90 mmHg HbF rapidly disappears in the first few weeks of life Pediatric Anatomy/Physiology Respiratory System Pediatric airway Physiologic anemia peaks at 3 months of age Hgb remains relatively low until teenage years (10-11g/dl) Children have a lower oxygen affinity for hemoglobin; therefore tissue unloading is higher, that is why they can have lower HGB levels and not be affected Pediatric Anatomy/Physiology Renal System Full term infants have the same number of nephrons as adults Glomeruli are much smaller than in adults GFR in the newborn is 30% that of the adult Tubular immaturity leads to a relative inability to concentrate urine Pediatric Anatomy/Physiology Renal System Fluid turnover is 7 times greater than that of an adult Altered fluid balance can have catastrophic consequences Organ perfusion and metabolism count on adequate hydration Infants and children are at a much higher risk for developing dehydration Pediatric Anatomy/Physiology Hepatic System Neonatal liver is large Enzyme systems exist but have not been sensitized or induced Neonates rely on limited supply of stored fats Gluconeogensis is deficient Plasma proteins are lower, greater levels of free drug exist Pediatric Anatomy/Physiology GI System Gastroesophageal reflux is common until 5 months of age Due to inability to coordinate breathing and swallowing until then Gastric pH and volume are close to adult range by 2nd day of life Gastric pH is alkalotic at delivery Pediatric Anatomy/Physiology Pharmacologic considerations Uptake Route of administration affects uptake IV – fastest Oral and rectal routes slowest Transdermal faster than adults, due to realtively thin skin layers Pathological conditions of the liver and heart can significantly effect uptake Pediatric Anatomy/Physiology Pharmacologic considerations Distribution 55-70% of body weight is water in infants and children Large ECF leads to large Vol. of distribution In adults, ECF accounts for 20% of body weight In children, ECF accounts for up to 40% of body weight The concentration and effects of watersoluble agents are affected greatly by the larger Volume of Distribution Pediatric Anatomy/Physiology Pharmacologic considerations Plasma protein binding Lower levels of serum albumin yield higher levels of free drug Plasma protein levels are even lower in certain disease states, like nephrotic syndrome or malnutrition Endogenous molecules, like bilirubin, can be displaced by protein bound drugs Pediatric Anatomy/Physiology Pharmacologic considerations Metabolism Soundness and maturity of the liver affect metabolism Glucuronidation is underdeveloped in neonates Maternal use of drugs may affect enzyme induction Medications, like phenobarbital, induce enzymes rapidly Pediatric Anatomy/Physiology Pharmacologic considerations Excretion Renal excretion is dependent on glomerular filtration, active tubular secretion, and passive tubular reabsorption Drugs dependent on renal excretion, like Pancuronium and Digoxin, can be markedly affected by immature kidney function Kidneys receive a lower percentage of CO than in adults GFR does not reach adult level until age 3-5 Pediatric Anatomy/Physiology Pharmacologic considerations ONLY body weight or BSA should be used to calculate and determine correct pediatric drug dosages Body weight is used in premature infants As always, titrate to effect Pediatric Anatomy/Physiology Routes of administration Oral Sometimes it is difficult to gain cooperation Liquid forms have greater absorption Place in back corner of mouth in infants Intramuscular Gluteus medius muscle over age 2 Vastus lataralus under 2 Pediatric Anatomy/Physiology Pharmacologic considerations Intravenous Good luck starting it! May necessitate mask induction Use of EMLA or other anesthethetic cream Usually better luck the more peripheral you are Well protected and secured Pediatric Anatomy/Physiology Pharmacologic considerations Intravenous agents Typically pediatric patients require a larger kg dose than adults Example – Thiopental Adult 3-5mg/kg Neonate 3-4mg/kg Infant 5-7mg/kg Children 5-6mg/kg Pediatric Anatomy/Physiology Pharmacologic considerations Pediatric patients can be very sensitive to the repiratory depressant effects of narcotics Careful titration is vital Morphine 0.05-0.2mg/kg up front is commonly used in peds Fentanyl and demerol cause more respiratory depression Pediatric Anatomy/Physiology Pharmacologic considerations Muscle relaxants Increased doses due to increased volume of distribution When using succinylcholine, expect bradycardia if you didn’t pretreat with an anticholinergic agent