PTSD & Mental Health Across the Lifespan Working with Veterans
advertisement

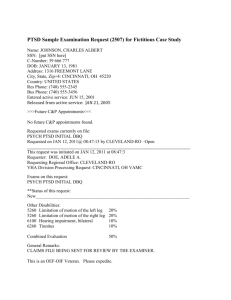
PTSD & Mental Health Across the Lifespan Working with Veterans affected by combat & trauma experiences Edgardo Padin-Rivera, Ph.D. Chief, Psychology Services February 26, 2015 VETERANS AND WARS • There are approximately 20 million veterans alive today. • 1.6 million (~8%) are women • 9.3 million (~ 47%) are over 65 • Most veterans served during wartime (>60%). • Approximately 30-40% were exposed to combat. • The Vietnam era veteran, ~7.2 million living, is the largest segment of the veteran population. *Source: US Census Bureau, 2013 AGE DISTRIBUTION OF U.S. VETERANS IN 2010 Data source: VettPop2011 VETERANS AND WARS WWII (1941-1945) Veterans (16 million) • Less than 1 million living today; Median age = 90 • Over 450 die daily • More than 30% in combat. • Approx. 25% have had PTSD symptoms. • Stoic, resigned to suffering combat memories. • Relatively uninformed on MH issues. VETERANS AND WARS Korean War (1950-1953) Veterans • Over 2 million war era veterans living; Median Age: 85 • ~ 850,000 living who served in combat. • Very patriotic; but mixed feelings about “forgotten” status. • Stoic, resigned to painful memories, similar values to WWII generation. VETERANS AND WARS Vietnam War (1960-1975) Veteran Generation • 9.1 million served on active duty; 6.9 million living. • 2.5 million served in South Vietnam. • 1.5 million (60%) in combat or exposed to direct combat. • Avg. age=67; youngest is 55. • First historical group to be labeled with PTSD. • PTSD estimates at between 7-28% depending on study. VETERANS AND WARS Vietnam War (1960-1975) Veteran Generation • First veteran group to demand individual recognition • • • • • for pain & suffering from war. Many are bitter, disillusioned, conflicted about the war. Many felt blamed, disparaged for participating in war. Carry feelings of betrayal by society. Aware of PTSD, but tend to mythologize. More likely to talk about experiences (but not all). COMING HOME: FALLING OUT Veterans Seeking Mental Health Services • < 40% have been in combat zone. • > 70% have been exposed to traumatic event. • < 25% diagnosed with PTSD. • > 45% suffer from multiple mental health issues. • > 50% have substance abuse problems. • Most have relationship problems at home or work. COMING HOME: FALLING OUT The Not-PTSD Syndrome • Memories may generate conflict, pain, fear, disgust & may be difficult to integrate into self-concept. • Self-blame, guilt, or shame for actions of war or failure to act. • Disillusionment with previous social & spiritual life. • Challenging core beliefs about self and intentions of others. • Experiences of death & loss lead to fear of intimate relationships. Post-Traumatic Stress Disorder PTSD is caused by exposure to such extreme stress that it changes the way a person thinks, copes and behaves in response to other stressful situations. • The event involves the actuality or threat of serious harm or death to self or others. • Reaction to the event is ongoing distress and inability to manage associated memories or emotions. • Diagnostic criteria consists of multiple symptoms a person may acquire long term (> 6 mos.) after exposure to an intensely stressful event. Post-Traumatic Stress Disorder Underlying Problems in PTSD • Inability to process an event into a memory – Overwhelmed by emotions – Unable to gain insight or place experience in history. • Alienation from self & social connections – Lost capacity for joy, pain, self-reflection – Lost capacity to fully trust others emotionally – Lost capacity to trust self-control • Involuntary changes in physical reactions & brain activations. • Highly reactive to environmental demands • physiological reactivity (GSR, HR difficult to control). Post-Traumatic Stress Disorder PTSD is manifested through a constellation of 20 different symptoms that may occur in someone after exposure to extremely stressful (trauma) events. Major symptom categories are: B. C. D. E. Intrusive Re-experiencing events Avoiding reminders of the events Negative Mood & Cognitions Constant or chronic physical arousal Post-Traumatic Stress Disorder Associated Symptoms & Disorders • Major Depression (MDD). • Alcohol & Drug Abuse/Addictions. • Phobias (crowds, enclosed places). • Panic Disorders (Rain; Overpass). • Stress-related Medical Disorders. • Social & functional impairment: work disruptions, marital, family or relationship problems. COMING HOME: FALLING OUT Alcohol and Drug Abuse often associated with PTSD • Work as way to dull post-trauma memories. • Quick way to alleviate anxiety and painful emotions. • Allows social interaction without emotion inhibitions. • Creates fast moving, transient emotional states. • Helps maintain status quo. • Helps develop and reinforce “safe” social alienation. Post-Traumatic Stress Disorder Stages of Coping Across the Lifespan • Turmoil – disabling symptoms, inconsistent life progress. • Repression – subconscious denial of symptoms or memories. • Suppression – Consciously denying any effects. “White knuckle syndrome”. • Vulnerability – adequate functioning with limited capacity for stress. • Integration – successful resolution and enhanced functioning. Traumatic Memories & Vulnerability • Post-traumatic anxiety may resurface or surface for first time in later life or end of life. • Deteriorating cognitive controls may make it more difficult to suppress or repress memories. • Losses of supportive relationships may be source of re-activation. Traumatic Memories & Vulnerability Understanding the Emotions of Vulnerability Turmoil at this stage of life include fears of • Aging body and deterioration of hearing, vision, taste, smell, touch/pain. • Failing kidney/prostate, ability to walk, deterioration of heart & lungs function. • Brain Aging: Difficulties in memory, new learning, language and speech, decision-making and planning capacities. • Pre-existing medical or other mental Illnesses may result in declines in reality testing or disorganized thoughts. • Veteran may be aware but may need (want) to be in denial. Traumatic Memories & Vulnerability Understanding the Emotions of Vulnerability • Threat to life inherent in surgery or terminal illness may elicit emotions of original trauma, triggering memories & symptoms. • Those who coped by suppression, repression, or avoidance may be especially vulnerable to overwhelming anxiety if memories reactivated. • Life review, normally a healing process, can lead to intense anxiety, sadness, guilt, or anger when trauma experiences need integrating. • Veteran with history of social isolation and avoidance may find self without supportive relationships or caregivers. Traumatic Stress Assessment Engagement questions for Veterans: • If veteran status known, ask, ‘What branch of service were you in?’ • Then, if not known, ask “Where did you serve in the military?” • Acknowledging that aspect of their lives increases chances of establishing a connection. • You may then ask: “Did you experience combat?” • Then, “Do any of your experiences or memories from the military or combat upset or bother you?” • You decide when to move on. Listen. Be non-judgmental. INTERVENTION CHALLENGES Myths that hinder caregiver–patient communication • • • • Myth that once a person has PTSD they will always have it. Myth of PTSD veteran as angry, vocal, asocial, crybaby. Myth that every combat veteran suffered terrible trauma. Myth that painful, bittersweet, or conflictual memories are PTSD. • Myth that person HAS to talk about their trauma to feel better or come to peace about their life. • Myth that suppression of feelings or memories is a bad way of coping. INTERVENTION STRATEGIES Basic Needs a Patients: • Clean & Safe Environment • Engaging, not intrusive, not patronizing staff • Consistency & control, e.g., knowing what comes next. • Inpatients: mild stimulation on a regular basis. INTERVENTION STRATEGIES If PTSD is suspected or evident, consider the following: 1. Engage (listen) quietly, being witness to veteran experience can sometimes be enough. 2. Do not push to process traumatic material. 3. Normalize & educate on PTS. 4. Emphasize patient’s control over medical decisions. 5. Link patients in support. 6. If Sx. are severe, ask for PTSD consultation. INTERVENTION STRATEGIES Normalize & Educate • Basic Tenet #1: PTS is normal human reaction to extremely stressful events. • Basic Tenet #2: Symptoms are manageable. • Basic Tenet #3: Confusing and conflicting emotions are to be expected. • Basic Tenet #4: Talking is difficult, but connection with others can help. INTERVENTION STRATEGIES Link patients in Support • Find ways for patients to provide support to each other through groups (story telling, readings, sharing pictures). • Link patients: Look for role models of integration. • Develop activities that fill need to address memories (prayer, writing letters to buddies, verbal journals) fill need to create legacy. STAFF & CAREGIVER CHALLENGES Challenges from caregiver and staff reactions: • May experience strong negative emotional reactions to PTS symptoms, especially with patients who are suspicious, resistant, confrontational, or highly distressed. • May over-identify with patient resulting in excessive sympathy for their suffering, anger at military, society, patient, even self. • May have difficulty engaging emotionally at any level, leaving patient to feel caregiver is cold, uncaring, stiff, or hostile. STAFF & CAREGIVER CHALLENGES Staff & Caregiver Education when a veteran has symptoms: • Inform caregivers of manifest PTSD difficulties or symptoms. • Provide information on how these can interfere with care. • Provide reassurance to staff who have strong emotional reactions to patient (e.g., sympathy, anger, guilt). • Develop a set of PTSD resources (see resources guide). • Locate consultants with PTSD expertise. STAFF & CAREGIVER CHALLENGES Collaboration Enhances Caring • All disciplines need to understand how PTS may affect veterans' physical, emotional, and spiritual care. • Caregivers and family members may need to practice patience & serene “quiet engagement” to deal with agitation and restlessness. • Principal interventions are expressing honor, dignity and gratitude for service. STAFF & CAREGIVER CHALLENGES Immediate goal is to provide comfort & manage symptoms. Approaching the Paradox of PTSD Symptoms • Physical vs. Emotional pain. • Recall vs. Re-experience. • Insight vs. Spiritual Peace • Guilt or Shame vs. Pride RESILIENCY RESOURCES: COMMUNITY SUPPORT Ve t e ra n p e rc ep t i o n o f p o s i t i ve c o m mu n i t y support, whether or not it is used, is one of t h e b e st k n o w n a n t id o t e s t o ch ro n ic m e n t a l h e a lt h p ro ble m s a f t e r a t ra u m at ic eve n t . If you see a returning service member this month, just say thank you.