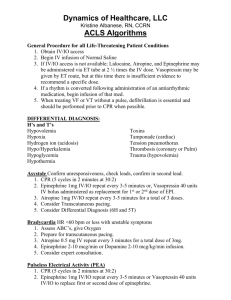
ACLS Case Scenarios: Emergency Medical Response & Algorithms
advertisement

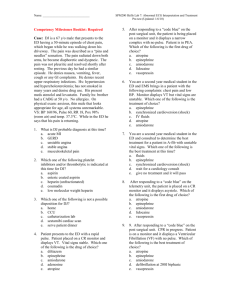
ACLS 2010 Case Scenarios 1 • A 40 year old man arrives at the ER accompanied by his family. He is complaining of palpitations after working outside for several hours. • The assessment is as follows: – SKIN: Hydrated, pale, warm and dry – CVS: Strong peripheral pulses and a BP of 125/80 – CNS: Fully intact – RESP: RR is 22, no resp. difficulties, lungs CTA • The monitor shows narrow complex SVT with a HR of 180 1. You place o2 at 2L by NC on the patient and start an IV. The monitor continues to show a narrow complex SVT 1. What is your next intervention? – Give adenosine 6mg rapid IV push – Attempt vagal maneuvers – Perform immediate synchronized cardioversion – Give epinephrine 1mg IV push 2. You have performed vagal maneuvers and there is no change in the patients heart rate and rhythm. What is your next step? – Give adenosine 6mg rapid IV push. If no conversion, give 12mg rapid IV push – Give adenosine 12mg rapid IV push. If no conversion, give another 12mg rapid IV push – Give Amiodarone 150mg over 10 minutes. May repeat as needed – Continue to attempt vagal manuvers until the patient converts to a regular sinus rhythm 3. You give 6mg Adenosine rapid IV push with no effect. 12mg Adenosine rapid IV push is then given. The patient develops severe chest pain and his vital signs are: HR 220, BP (not obtainable), and weak pulse. Your next step should be. – Perform immediate defibrillation – Give 2nd dose of 12mg adenosine rapid IV push – Perform immediate synchronized cardioversion – Perform precordial thump • 4. After synchronized cardioversion is unsuccessful, the pt. continues to deteriorate. The patient is now unconscious with pusleless ventricular tachycardia. Below is what you see on the monitor: What is your first intervention? – Begin CPR and give 5 cycles before shocking – Give Epinephrine 1mg IV push (repeat every 3-5 minutes) – Give one unsynchronized shock (120-200 J) – Place an advanced airway • 5. The patient does not respond to the defibrillation with 120 J. He remains unconscious in ventricular tachycardia. What is your next intervention? – Deliver a second shock (120-200 J) – Give 1mg Epinephrine IV push (repeat the epinephrine every 3-5 minutes) – Give 5 cycles of CPR – Check the rhythm and the pulse • 6. After completing 5 cycles of CPR, your rhythm check indicates a second shock. You shock a second time with 160 J, and the patient's rhythm does not change. You resume CPR. While completing the cycle of CPR what else should be done? – A. Give Epinephrine 1 mg IV push (repeat every 3-5 minutes) – B. Vasopressin 40 U IV push to replace the 1st or 2nd dose of epinephrine – C. Give Epinephrine 0.5mg IV push (repeat every 35 minutes) – D. Either A or B is correct 7. You have given the epinephrine or vasopressin and completed the 5 cycles of CPR. A rhythm check reveals no change. You attempt at third defibrillation. What will be your defibrillator setting? – 300 Joules – 200 Joules – 160 Joules – 400 Joules 8. The third shock does not change the rhythm and you restart CPR (5 cycles). You have shocked, you have given vasopressors (epinephrine and/or vasopressin), you have continued with effective CPR. What medication should be considered at this point? – Amiodarone – Lopressor – Atropine – Dopamine 9. What is the correct dosing for amiodarone in the Pulseless Arrest Algorithm? – 150mg IV once. If this in not effective give 300mg IV once. – 200mg IV once. – 300mg IV once. Then consider an additional 150mg IV once. – Give IV infusion of 300mg per hour 10. Lidocaine can be used instead of amiodarone as an antiarrhythmic for pulseless arrest. What is the proper dosing of lidocaine? – 1.5 mg IV first dose, then 0.75 mg IV – 3 mg/kg rapid IV push – 0.5 to 0.75 mg/kg IV, if no affect 1 to 1.5 mg/kg IV – 1 to 1.5 mg/kg first dose, then 0.5 to 0.75 mg/kg IV 11. You give amiodarone 300 mg first dose and the patient converts to a Normal Sinus Rhythm. You are instructed to start an amiodarone drip for the post resuscitation maintenance therapy. What is maximum cumulative dose for amiodarone in a 24 hour period? – 2.2 grams – 3.2 grams – 1.5 grams – 5.6 grams 12. Great Job! You saved the patient He has been stabilized and intubated, but does not respond to verbal commands. He is transported to the hospital's ICU. Since the patient is not responsive what would be the most important intervention in the post-cardiac arrest phase. – Monitor waveform capnography – Obtain an arterial blood gas – Induce therapeutic hypothermia – Monitor oxygen saturation 2 • You are caring for a 50 year old female. She is 2 days post-op. from a total hip replacement. 6L/min by nasal cannula. When you enter the patient’s room, she appears to be unconscious and you note that her nasal cannula is laying beside her bed. • Your initial assessment reveals: – SKIN: ashen, diaphoretic, warm – CVS: Carotid pulse only, HR 25, unable to obtain blood pressure – RESP: sporadic and shallow – CNS: Unresponsive – Monitor: Significant bradycardia; HR 25 1. You have called for help. Being an in hospital setting emergency, your first priority is to: – Give epinephrine – Begin chest compressions – Secure the airway and ventilate with BVM (bag valve mask) – Establish IV access 2. Which is the correct order for treatment in this scenario? – Assist breathing and give oxygen, monitor ECG & VS, establish IV access – Give oxygen, monitor ECG & VS, establish IV access, assist breathing – Monitor ECG & VS, assist breathing and give oxygen, establish IV access – Establish IV access, Give oxygen, monitor ECG & VS, assist breathing 3. The patient is showing clear signs of poor perfusion, you should: – Observe and monitor – Give adenosine 6mg rapid IV push – Give atropine 0.5mg IV – Begin CPR 4. You give atropine 0.5mg IV push. There is no change in the patients rhythm/rate. What will be your next intervention? – Attempt transcutaneous pacing – Increase atropine to 1mg IVP – Adenosine 1mg IVP – Norepinephrine 1mg IVP 5. Transcutaneous pacing is attempted. You set the pacing rate for 60/min and attempt capture. After trying for about 30-40 seconds, you are unable to achieve capture. What other medication may now be considered for use in the bradycardia algorithm? – Epinephrine – Dopamine – Amiodarone – Both epinephrine or dopamine – Both dopamine or amiodarone 6. Which is the correct dosing for an epinephrine infusion in the bradycardia algorithm? – 1 mg/min – 2-10 mcg/kg/min – 2-10 mcg/min – 0.5mg/min 7. As you prepare for an epinephrine infusion and consider transvenous pacing, the patients rhythm suddenly changes. This is what you see on the monitor. What should be checked to ensure that this is true asystole? – Loose leads or leads not connected to the patient – Signal gain – Ensure that the patient is pulseless – All of the above 8. You confirm that this is true asystole and that the patient has no pulse. You begin the pulseless arrest algorithm. Your first step is to: – Give 1 shock (120-200 J) – Give epinephrine 1 mg – Begin CPR immediately – Continue transcutaneous pacing 9. As you begin CPR, you recall the number of CPR cycles that are to be delivered between other interventions is ________ and you also recall that the correct compression-toventilation ratio is __________. – 5, 30:2 – 10, 10:2 – 2, 30:2 – 15, 10:1 10. After you begin CPR what is your next step? – Give atropine 1 mg IV/IO – Continue CPR, nothing else can be done – Give 1 shock – Give epinephrine 1 mg IV/IO 11. As you finish up with the first cycle of CPR and give the first dose of epinephrine (1mg IVP), the rhythm changes. The rhythm below is what you now see on the monitor. The patient remains unresponsive. What is this rhythm? – Artifact – Ventricular tachycardia – Atrial fibrillation – Ventricular fibrillation 12. You determine that this rhythm is ventricular fibrillation, and you begin the pulseless arrest algorithm. What is your first intervention? – Give 1 shock (120-200 J) – Give 3 stacked shocks – Continue CPR – Give epinephrine 1mg IV/IO 13. You shock the patient with 120 J and continue CPR immediately. After 5 cycles of CPR, your rhythm check reveals no pulse and continued ventricular fibrillation. What is your next step? – Give epinephrine 1mg IV/IO – Check to see that your leads are still connected – Give 1 shock – Give atropine 0.5mg IV/IO 14. A second shock is delivered at 200 J, and it does not change the rhythm. Your next intervention is to: – Seek expert consultation – Consider giving antiarrhythmics – Check a pulse for no more than 10 seconds – Give 1 mg epinephrine while continuing CPR 15. The epinephrine is given, and after the cycle of CPR ventricular fibrillation continues. You give a third shock (200 J) without effect and resume CPR. What is your next intervention? – Give lidocaine 2 to 2.5 mg/kg IV/IO – Give magnesium 2 to 4 grams IV/IO – Give atropine 1mg IV/IO – Give amiodarone 300mg IV/IO 16. You give the amiodarone 300 mg IV and after 5 more cycles of CPR you check the rhythm which remains in ventricular fibrillation. What is your next step? – a. consider additional dose of amiodarone 150 mg IV – b. consider giving atropine 0.5mg IV – c. shock (200 J) – d. both A and C 17. You shock the patient and after shocking you see the following rhythm on the monitor. The patient has a palpable pulse. VS are: HR 60; BP 105/65; RR 5-8 You have corrected the ventricular fibrillation and the patient is stabilizing. You now consider maintenance antiarrhythmic therapy. Which is the best drug of choice in this scenario? – – – – Amiodarone Lidocaine Epinephrine Magnesium sulfate 3 מקרה • A 65 year old male collapses as he is out for his morning walk. A bystander witnesses the collapse, activates EMS, and begins CPR. The EMS team arrives shortly, takes over CPR, and attaches a defibrillator. The assessment is as follows: • Skin: cold/clammy/cyanotic Cardiovascular: no pulse Respiratory: no respirations CNS: no response Monitor: rhythm strip below • 1. What ACLS algorithm are you going to begin this scenario with ? – Pulseless Arrest (VT/VF branch) – Bradycardia (unstable branch) – Pulseless Arrest (Asystole/PEA branch) – Unstable Tachycardia • 2. As an EMS provider in the out of hospital setting, your first step is to: – Give epinephrine 1mg IV/IO – Give CPR for 5 cycles – Give atropine 1mg IV/IO – Give 1 unsynchronized shock (120-200 J) • 3. While you are giving 5 cycles of CPR you can also carry out what other activities? – secure the airway – start an IV – provide the patient with oxygen – all of the above • 4. After your IV is secure, your next step involves giving a medication. What medication should be used? – epinephrine 0.5mg IV – atropine 1mg IV – vasopressin 20 U IV – epinephrine 1mg IV • 5. What medication can replace the first or second dose of epinephrine? – atropine 1 mg IV – adenosine 6mg IV – vasopressin 40 U IV – atropine 0.5 mg IV • 6. Epinephrine should be repeated at what frequency in this algorithm? – every 3-6 minutes – every 3-5 minutes – only 3 times – after each cycle of CPR • 7. After giving the first dose of epinephrine you finish the cycle of CPR. A rhythm check shows that the patient's rhythm changed from asystole to the rhythm below. He also remains pulseless. Your first action is to: – give 5 cycles of CPR – give another dose of epinephrine 1mg IV – give 1 unsynchronized shock (120-200 J) – give amiodarone 300mg IV x 1 • 8. You deliver 1 shock of 120J. After the shock what is the your next step? – deliver a second shock – check a pulse – resume CPR (5 cycles) – give epinephrine 1mg IV • 9. You have resumed CPR. Your next intervention after 5 cycles of CPR is to: – perform a rhythm check – assess breathing – shock before any other intervention – give vasopressin • 10. Your rhythm check reveals continued pulseless VT. What are your next 2 steps? – 1 shock, check rhythm – 1 shock 150 Joules, epinephrine 1mg IV – 5 cycles CPR, epinephrine 1mg IV – 1 shock 150 Joules, 5 cycles CPR • 11. You give a second shock and perform 5 cycles of CPR. What medication should you give after the second shock during CPR ? – Epinephrine – Amiodarone – Atropine – Lidocaine • 12. You give epinephrine 1 mg IV and finish the cycle of CPR. What is your next intervention ? – give amiodarone 300 mg IV – give epinephrine 1 mg IV – shock 120-200 J – rhythm check • 13. The rhythm check reveals no change in the rhythm. You shock with 200 J and start another cycle of CPR. What medication are you going to give at this time ? – give lidocaine 1-1.5 mg IV – epinephrine 1 mg IV – amiodarone 300 mg IV – vasopressin 40 U IV • 14. You give amiodarone 300 mg IV and finish the cycle of CPR, your rhythm check reveals continued pulseless VT, continuing on, you shock the patient again. What is your intervention at this time. – complete 5 cycles of CPR – check a pulse – start amiodarone drip – give epinephrine 1 mg IV • 15. After completing 5 cycles of CPR a rhythm check reveals the following: • Your pulse check reveals a faint palpable pulse. VS are: HR 30; BP 78/58; and the patient does not have spontaneous breathing. What is the next step? – continue CPR – give atropine 1 mg IV – perform intubation – initiate transcutaneous pacing • 16. You recognize this rhythm because there is no apparent relationship between the Pwaves and the QRS complexes. What is the rhythm ? – sinus bradycardia – sinus rhythm – third-degree heart block – second-degree block • 17. After you initiate TCP the patient continues to stabilize. VS are: HR 70; BP 105/75; RR 5; You continue to support ventilation with the bag valve mask, and TCP continues. If transcutaneous pacing was not available, what medication can be considered as an alternative. – – – – – – a. atropine b. dopamine c. epinephrine d. vasopressin e. none of the above f. either b or c 4 מקרה • Scenario data: 50 year old man brought to the ER by his son. He complains of occasional dizziness and lightheadedness for about 12 hours. He says that he is also occasionally short of air. The assessment is as follows: • Skin: Warm/Dry Cardiovascular: Pulse palpable (strong), BP 96/68, HR 140′s; no chest pain Respiratory: Lungs CTA bilaterally, no respiratory distress; RR 22 • 1. You identify the patient’s condition as: – stable tachycardia – unstable tachycardia – ventricular fibrillation – unstable supraventricular tachycardia • 2. Since the patient's rhythm is stable at this time, what are some things that you should do to begin? – establish IV access – give supplemental oxygen – search for reversible causes – all of the above • 3. The QRS is obviously wide (>.12 sec), stable, and monomorphic. In light of the new 2010 guidelines, you are going to prepare to give which medication? – adenosine 6 mg rapid IV push – atropine 0.5 mg IV push – epinephrine 1 mg IV push – amiodarone 540 mg IV push • 4. There is no response to adenosine 6mg rapid IV push, and a second dose 12mg dose fails to convert the patient as well. What is another medication that you could consider using in the tachycardia algorithm ? – lidocaine 2mg/kg – atropine 1mg IV – amiodarone 150mg IV over 10 minutes – epinephrine 1mg IV • 5. The patient has opted for elective cardioversion, as you prepare for the elective synchronized cardioversion, your patient begins to experience severe chest pain and becomes short of air. His vital signs also change (BP 70/?; HR 160; RR 28). The patients rhythm on the monitor now looks like this : • The patient still has a pulse. What should be your intervention at this time? – Give adenosine 6mg IV push – Perform immediate synchronized cardioversion – Give epinephrine 1mg IV/IO – Begin CPR • 6. The patient remains conscious so you sedate with versed and perform synchronized cardioversion. When the cardioversion is performed, the defibrillator is placed in the sync mode. When during the QRS complex, is the sync mode designed to deliver energy (shock)? – just before the R wave – just after the S wave – just before the Q wave – at the peak of the R Wave • 7. After synchronized cardioversion, the pt. deteriorates further and loses consciousness. His rhythm changes and the patient has no pulse. This is what you see on the monitor: • Identify the pictured rhythm? – ventricular tachycardia – atrial flutter – ventricular fibrillation – atrial fibrillation • 8. You identify this as ventricular fibrillation. What is your first intervention? – give epinephrine 1mg IV push – begin CPR – give 1 unsynchronized shock – give 1 mg atropine IV push • 9. You defibrillate the patient with 120 Joules and begin 5 cycles of CPR. After 5 cycles, your rhythm check reveals the following rhythm: • With this new change in rhythm what is next intervention? – give vasopressin 4 U IV – resume CPR for 5 cycles – give atropine 1 mg IV/IO – give 1 unsynchronized shock • 10. You resume CPR and give 5 cycles. While you are giving CPR, what are 2 medications that you can consider using? – epinephrine, lidocaine – atropine, adenosine – amiodarone, atropine – epinephrine and vasopressin • 12. You have given vasopressin 40 U IV x 1 and completed a cycle of CPR. A rhythm check shows that asystole continues and the patient remains unresponsive. You should do what at this point? – continue CPR – give epinephrine 1mg IV – give adenosine 6mg IV – give atropine 1mg IV • 13. You continue CPR giving 5 cycles CPR along with epinephrine every 3-5 minutes. You have used your one time dose of vasopressin. What is the maximum number of doses of epinephrine that can be given? – 10 –3 –6 – No limit • 14. You have continued CPR and medications per ACLS asystole algorithm for 20 minutes. The patient remains in asystole. There has been no response to epinephrine, or vasopressin, and atropine is no longer recommended according to the new 2010 ACLS guidelines. What is your next intervention? – attempt transcutaneous pacing at 60 beats per minute – consider termination of CPR/ACLS – give one unsynchronized shock – all of the above • 15. (True or False) On average, 20-25% of patients who have witnessed (in-hospital) cardiac arrest with ACLS treatment survive. – True – False