HPI
advertisement

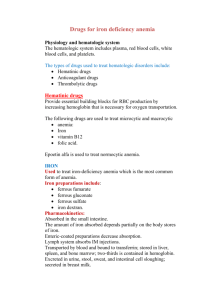
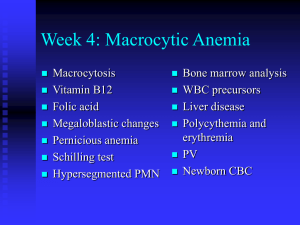
HPI •58 year old African American female presents to your clinic with one month history of fatigue and shortness of breath. •What else would you like to know? HPI continued • Patient states that the shortness of breath usually occurs when she is climbing stairs or walking down the long hallway in her house. • She says for the past month she has not had much of an appetite, and she has been experiencing diarrhea. • She reports numbness and tingling in her fingers and toes. Medical History • Past medical history: Hashimoto’s thyroiditis • Past surgical history: Hysterectomy at age 45 • Medications: Synthroid (synthetic thyroid hormone) • Social History: Single. Retired administrative assistant. Denies smoking, alcohol, illicit drugs. • What is on our differential diagnosis? Differential Diagnosis • Hypothyroidism • Malignancy • Malabsorption syndrome (ie Zollinger-Ellison syndrome) • Infection (ie D. latum tapeworm) • Anemia – Aplastic anemia – Hemolytic anemia – Pernicious anemia • Depression What would you like to do next?? Physical Exam • Vitals: Temp 98.6F, Pulse 110, Resp 20, BP 130/85 • General: Well-nourished African American female. No acute distress. • HEENT: Pale conjunctiva, angular cheilitis, glossitis. • Cardio: Mildly tachycardic. Regular rhythym. No murmurs, rubs, or gallops. • Resp: Breath sounds clear bilaterally to auscultation. Non-labored breathing while sitting. • Neuro: -Diminished sensation to vibration bilaterally in upper and lower extremities. Intact proprioception. Mild ataxia during heel-toe walking. Romberg test positive. What tests should we order? Laboratory Tests • WBC 45000 (normal) , Hgb 9.0 (low) , Hematocrit 27.0 (low) , • MCV 115 (increased) • B12 level: 100 pg/ml (low) • Folate level: 10 ng/ml (normal) • Methylmalonic acid: 0.6 umol/L (elevated) • Homocysteine: 15 mcmol/L (elevated) • Serum intrinsic factor blocking antibody: present • Gastrin: 300 pg/ml (elevated) Peripheral smear • Findings: -Hypersegmented neutrophil (seven lobes) -Macroovalocytes • In light of the lab results and peripheral smear, what is your diagnosis? Resolution • Patient was diagnosed with pernicious anemia. •Patient was begun on lifelong B12 replacement therapy. Pernicious Anemia • Pernicious anemia is a classification of B12 deficiency which is caused by a lack of intrinsic factor from the stomach’s parietal cells. • B12 gets absorbed in the terminal ileum only when bound to intrinsic factor. Without the intrinsic factor, the body will not be able to absorb B12. • Two common causes of pernicious anemia: – Antibody to IF (in the case of our patient) – Atrophic gastritis (IF is not being produced properly) Clinical Presentation Patients with pernicious anemia can present with a variety of issues including: • • • • • • • • • • Weakness Fatigue Shortness of breath Ataxia Loss of proprioception Peripheral neuropathy Poor coordination Personality changes Glossitis (tongue inflammation) Angular chelitis (inflammation/cracking in the corners of the mouth) • Changes in bowel habits (constipation or diarrhea) Evaluating MMA and Homocysteine Patient Condition Healthy Vitamin B-12 deficiency Folate deficiency MethylmalonicAcid Normal Elevated Normal Homocysteine Normal Elevated Elevated This diagram reminds us about the metabolism of MMA and homocysteine. Diagnosis • Once it is found that the patient has a macrocytic anemia (low hemoglobin with elevated MCV), evaluation of the MMA and homocysteine levels can then help confirm the etiology. • The Schilling Test can also be employed, in which B12 and intrinsic factor are given in different monitored stages to determine the etiology of the B12 deficiency. • Usually a bone marrow biopsy is not needed for diagnosis. Below is a picture of a normal bone marrow biopsy on the left, and a biopsy of a patient with pernicious anemia on the right. Megaloblastic erythropoeisis is seen in both B12 and folate deficiency bone marrow samples. Treatment • Lifelong B12 replacement therapy is ordinarily required for a patient with pernicious anemia. • The regimen begins with 1000 mcg injection daily for a week, then 1 mg weekly for a month, then usually 1 mg every month for the remainder of the patient’s life. • It takes time for the neurological symptoms to improve (numbness and tingling, with our patient). Between 6 months and a year after beginning treatment, usually a patient’s neurological symptoms are the most improved they will ever be. If the anemia has been going on for an extended time before treatment, some symptoms may never fully improve.