CONSERVATIVE TREATMENT OF FRACTURE AND CAST
advertisement

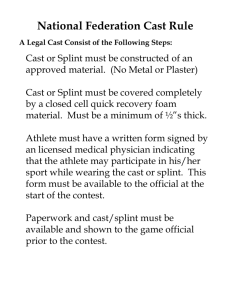
CONSERVATIVE TREATMENT OF FRACTURES Dr. Muhammad ASIF Orthopedic Surgeon Department of Orthopaedics College of Medicine King Khalid University Hospital Fracture management The ideal goal of fracture management is anatomical reduction and function restoration compatible with the severity of injury, age, occupation and activity of daily living of injured patient. Either Operative Non operative (Conservative) Traction Splint (Cast / Slab) Traction Traction is the application of a pulling force to a part of the body Purpose: to reduce, align, and immobilize fractures; • Unstable and unfixable When reduction and/or proper length cannot be maintained by static immobilization to minimize muscle spasm to prevent or reduce skeletal deformities or muscle contractures. Classification of Traction Skin Traction : is maintained by direct application of a pulling force on the patient’s skin . Generally temporary measure. To reduce muscle spasms To maintain immobilization before surgery In children Skeletal Traction : applied to bone by means of a pin or wire surgically inserted into the bone, providing a strong steady, continuous pull, and can be used for prolonged periods . Complications of traction Neurovascular compromise. Inadequate fracture alignment.. Skin breakdown . Soft tissue injury Pin tract infection . Osteomyelitis can occur with skeletal traction. Complications of traction complications from immobility especially with long term traction and in elder pt. Pressure ulcer Pneumonia Constipation Anorexia Urinary stasis and infection Venous stasis with DVT General Indications for CAST 1. Most fractures in children: a. Tremendous capacity of remodeling. b. Non union and stiffness is unlikely. 2. Undisplaced fracture 3. Poor bone Quality: Osteoporosis. 4. Unfixable fracture e.g. severe comminuted. 5. Systemic contraindication. 6. Local contraindication. 7. Psychosocial problem. Splint / Cast Principle: To stabilize joint above and joint below the site of injury whenever and wherever is possible Objectives: To hold broken bone anatomically to prevent malunion. To reduce excessive movements to prevent non union. To get early function How to Preserve Function? Immobilize only joint necessary, Range of motion of uninvolved joints. Isometric exercise. Physiotherapy after cast removal. Weight bearing whenever possible in case of lower limb fracture. What are casts made of ? The outside, or hard part of the cast, two different kinds of casting materials. Plaster (POP) - white in color. hemihydrated calcium sulphate. On adding water it solidifies by an exothermic reaction into hydrated calcium sulphate fiberglass - variety of colors, patterns, and designs. inside of the cast Cotton and other synthetic materials are used to line the inside of the cast to make it soft and to provide padding around bony areas. Plaster is usually used in the early stages of treatment, Displaced Fracture that need manipulation can be molded more precisely. heavy must remain dry, water will distort the cast Fiberglass Can be used in Undisplaced Fx if swelling not expected healing process has already started. lighter weight, durable, require less maintenance. Different types of casts Type of Cast/Slab Location Uses Short arm Applied below the elbow to the hand. Distal Forearm or wrist Fx. Also used to hold the forearm or wrist muscles and tendons in place after surgery. Long arm Applied from the upper arm to the hand. Distal humerus, elbow, or proximal forearm fractures. Also used to hold the arm or elbow muscles and tendons in place after surgery. Scaphoid cast/ thumb spica Below elbow to hand including thumb Scaphoid Fx, thumb FX U slab From shoulder to elbow and then to armpit Humerus shaft fx Type of Cast / Slab Location Uses Short leg cast: Applied to the area below Distal T/F Fx, the knee to the foot. ankle Fx, severe ankle sprains/strains. Long leg cast From above knee to foot Proximal T/F Fx, trauma around knee Hip spica From lower chest to one or both feet Femur fracture in children PTB cast From knee to foot For weight bearing in healing Fx T/F Closed Reduction Method Closed Reduction Method Adequate analgesia / anaesthesia Traction – countertraction Increase the deformity if needed, to reduce / lock on fragments Correct rotational deformity as well. Remove any rings from fingers or affected limbs All acute injuries (<48 hours post injury) fully padded well molded plaster, full casts may be splittted. After Closed Reduction and Casting must have circulation check Plaster takes 48 hours to become fully dry and harden so take care. Weekly radiographs for 3 weeks to confirm acceptable reduction. Can re-manipulate within 3 weeks after injury if displaced. Excellent Reduction with Well Molded Cast Colles’ Fracture Displaced dorsolaterrally Treatment: Cast +/- surgery, depending on shortening and displacement Scaphoid Bone FX Retrograde blood supply Total healing time of 10-12 weeks or more Boxer’s Fracture Classically neck of the fifth metacarpal bump over the back of palm just below the small finger knuckle Treatment: casting or surgery (pins) Patellar Fracture Fall onto kneecap or when quadriceps is contracting Attempt “straight leg raise” If Extensor mechanism intact / undisplaced Fx Cast / Slab Fracture of 5th Metatarsal Avulsion base of 5th metatarsal from pull of attached tendon; heal well in cast Jones Fracture Fracture Transverse fracture through base of 5th metatarsal, about 1-2 cm from tip; cast for 6-8 wks if undisplaced Fracture of 5th Metatarsal Avulsion Fx Jones’ fracture 30 year old patient Torus Fracture “Buckle fracture” mostly in children; metaphysis cast for 2-4 weeks Type 1 S/C Fx humerus: non-displaced conservative Note the nondisplaced fracture (Red Arrow) Note the posterior fat pad (Yellow Arrows) Type 2: Angulated/displaced fracture with intact posterior cortex; close reduction and K-wires fixation Type 3: Complete displacement, with no contact between fragments; close / open reduction and K-Wire fixation UNDISPLACED FRCTURE LATERAL CONDYLE Fracture surgical neck humerus, 10 year old Post Cast instructions Keep your limb elevated to prevent swelling. Apply an ice bag to injured area. Keep the cast clean and dry. Check for cracks or breaks in the cast. Rough edges should be padded to protect the skin from scratches. Do not scratch the skin under the cast by inserting sticks. Encourage patient to move his/her fingers or toes to promote circulation Contd Prevent small toys or objects from being put inside the cast. Do not put powders or lotion inside the cast. Cover the cast while your child is eating to prevent food spills and crumbs from entering the cast. Do not use the abduction bar on the cast to lift or carry the child. Use a diaper or sanitary napkin around the genital area to prevent leakage or splashing of urine. How To Know if Something Is Wrong With Your Cast Pain that is not adequately controlled with medication prescribed by your doctor. Increasing swelling Numbness or tingling in the extremity (hand or foot). Inability to move your fingers or toes beyond the cast. Circulation problems in your hand or foot. Loosening, splitting or breaking of the cast. Unusual odors, sensations, or wounds beneath the cast. If you develop a fever or generalized illness Complications of cast Compartment syndrome, tight cast that restricts swelling. Impaired distal neurovascular. most serious is deep venous thrombosis leading to pulmonary embolism----calf pain. Re displacement of fracture. stiff joints, muscle wasting. Plaster Sores. Malunion, Nonunion, Delayed union Cast Burns- can occur during cast removal if blade dull or improper technique used. Fracture distal Radius & ulna Close reduction and casting Fracture Healed Fx distal Radius ulna in a Child After Close reduction and casting One week follow up; Angulated Surgery; close reduction and fixation Healed 21 year old patient THANKS