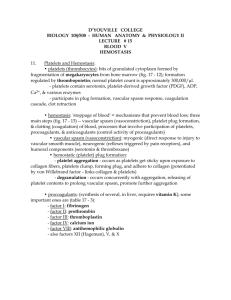
Wounds, Bleeding, and Healing
advertisement

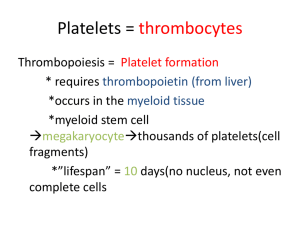
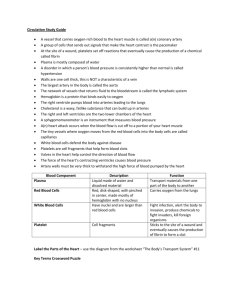
Wounds & Hemostasis By C. Kohn, Waterford WI Normal Blood Flow To have normal blood flow, blood must be kept at an exact viscosity (thickness) Too thin, and the smallest cuts would cause a pet to bleed to death Too thick, and the blood would not flow Anticoagulants keep the blood thin and allow it flow under normal circumstances Injury changes the situation Blood must not be allowed to flow freely everywhere or the wound would never heal 4 Types of Open Wound Abrasions-injuries destroying only surface layers of the skin. Incisions- wounds produced by sharp instruments these types of cuts usually have smooth edges. Puncture Wounds- penetrations of the superficial (surface- layer) tissue. Lacerations- cuts with irregularly torn edges. o Slide courtesy of Texas A&M Hemostasis The series of chemical reactions needed to stop bleeding is called hemostasis Hemostasis has three steps Step 0: Injury Step 1: Vasoconstriction – blood vessels constrict (or “shrink”) to slow blood flow at the site of injury Step 2: Platelet Plug formation – the wound is “corked”, or covered with sticky platelets Step 3: Formation of a fibrin blood clot – a more sturdy solution is created Step 1: Vasoconstriction In vasoconstriction, the walls of the blood vessels “shrink” to reduce the size of the area that blood can flow through. The muscles surrounding the vessel will contract, shrinking the vessel Step 2. Platelet Plug Formation At the site of injury, collagen will help platelets to stick to the site of the injury Collagen is sort of like branches that the platelets can grab onto as they pass in the bloodstream Platelets Platelets are formed in the bone marrow and live in your body’s circulatory system for roughly a week Platelets aren’t really cells – they do not have a nucleus and cannot divide Platelets do have a coat made of a particular protein that prevents a platelet from sticking to anything other than injured tissue Platelets contain contractile proteins (like those in your muscle cells) These proteins enable a platelet to expand and contract Inside the platelet are special chemicals that aid in the formation of the platelet plug (explanation on next slide). Clot Contraction & Repair About 30-60 minutes after a blood clot has formed, the platelets within the clot contract Like muscle cells, platelet cells can shrink due to actin and myosin contractile proteins This contraction pulls on the wound from the inside; bringing the edges of the wound closer together The blood clot is temporary – at the same time of contraction, the tissue surrounding the damaged site begin to divide and repair via mitosis. WBC RBC Platelet Degranulation: A Feed Forward Mechanism The platelets release granules that enable more platelets to get stuck. The more platelets that get stuck, the more granules are released the promote more platelets to get stuck. This is a “feed-forward” mechanism…the process becomes stronger as it happens more. Step 3: Coagulation The platelet plug will become reinforced with a fibrin “mesh net” This fibrin net also traps red and white blood cells in order to from a blood clot over the site of the injury The red blood cells will form a solid “plug” The white blood cells will aid in fighting infectious agents that are able to make it inside the body. Review: 3 Steps of Hemostasis 1. Vasoconstriction – the muscles of the damaged blood vessel contract to reduce the amount of blood flowing through it by reducing the size of the blood vessel 2. Platelet Plug Formation – collagen fibers protruding from the site of the injury ‘catch’ platelets and form a plug. Platelets contract and “shrink” the wound 3. Formation of a Blood Clot – a fibrin “mesh” catches red and white blood cells to form a clot and prevent infection. o http://www.mhhe.com/biosci/esp/2002_general/Esp/folder_structu re/tr/m1/s7/trm1s7_3.htm Prevention of Infection Once bleeding has been controlled, the next step is stopping infection The blood vessels that were constricted now dilate (open up) to bring white blood cells rushing to the scene. The process in which the wound swells and becomes inflamed is called inflammation. White Blood Cells White blood cells engulf and destroy any germs that may have gotten into the body through the open wound. This process of destroying germs creates heat This causes the trademark symptoms of serious wounds – swelling, redness, tenderness, and heat. The worse the infection, the greater the inflammation and heat. Fibrinolysis 2 days after clotting the fibrin mesh that holds the clot together is dissolved This process is called Fibrinolysis Source: thrombosisadviser.com Stuff You Should Know: Warfarin Warfarin (or Coumadin) is a blood thinner. It was originally a rat poison, and is still widely used for this method Rats that eat food laced with Warfarin die from blood loss because their blood is unable to coagulate Warfarin, in much lower doses is one of the most widely prescribed medications in the world. Warfarin can help dangerous clots from forming in heart attack and stroke victims Warfarin is named for WARF, or the Wisconsin Alumni Research Foundation. This is the agency that funds all research at the University of Wisconsin. Review What is necessary for normal blood flow? What is an anticoagulant? What are the four types of open wounds? What is hemostasis? What are the 3 steps of hemostasis? What is vasoconstriction and how does it happen? What is a platelet and how does it help a wound heal? How do they know where to go when there is an injury? How is a platelet different from other kinds of cells? What is a fibrin blood clot made from? (i.e. what is a scab?) How does it form? How does an open wound close? Why do open wounds sometimes swell, become hot, and look red? What is fibrinolysis? How does a wound “know” how to heal? What is Warfarin and what does it do?