Chapter 26: The Urinary
System
Copyright 2009, John Wiley & Sons, Inc.
Overview of kidney functions
Regulation of blood ionic composition
Regulation of blood pH
Regulation of blood volume
Regulation of blood pressure
Maintenance of blood osmolarity
Production of hormones (calcitrol and erythropoitin)
Regulation of blood glucose level
Excretion of wastes from metabolic reactions and
foreign substances (drugs or toxins)
Copyright 2009, John Wiley & Sons, Inc.
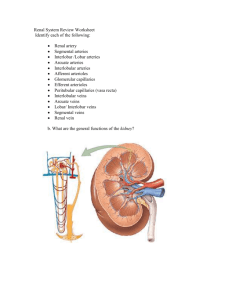
Anatomy and histology of the kidneys
External anatomy
Renal hilium – indent where ureter emerges along
with blood vessels, lymphatic vessels and nerves
3 layers of tissue
Renal capsule – deep layer – continuous with outer coat
of ureter, barrier against trauma, maintains kidney shape
Adipose capsule – mass of fatty tissue that protects
kidney from trauma and holds it in place
Renal fascia – superficial layer – thin layer of connective
tissue that anchors kidney to surrounding structures and
abdominal wall
Copyright 2009, John Wiley & Sons, Inc.
Organs of the urinary system in a female
Copyright 2009, John Wiley & Sons, Inc.
Position and coverings of the kidneys
Copyright 2009, John Wiley & Sons, Inc.
Internal anatomy
Renal cortex – superficial
Renal medulla – inner region
Outer cortical zone
Inner juxtamedullary zone
Renal columns – portions of cortex that extend between
renal pyramids
Several cone shaped renal pyramids – base faces cortex
and renal papilla points toward hilium
Renal lobe – renal pyramid, overlying cortex area,
and ½ of each adjacent renal column
Copyright 2009, John Wiley & Sons, Inc.
Anatomy of the kidneys
Parenchyma (functional portion) of kidney
Renal cortex and renal pyramids of medulla
Nephron – microscopic functional units of kidney
Urine formed by nephron drains into
Papillary ducts
Minor and major calyces
Renal pelvis
Ureter
Urinary bladder
Copyright 2009, John Wiley & Sons, Inc.
Internal anatomy of the kidneys
Copyright 2009, John Wiley & Sons, Inc.
Blood and nerve supply of the kidneys
Blood supply
Although kidneys constitute less than 0.5% of total body mass,
they receive 20-25% of resting cardiac output
Left and right renal artery enters kidney
Branches into segmental, interlobar, arcuate, interlobular arteries
Each nephron receives one afferent arteriole
Divides into glomerulus – capillary ball
Reunite to form efferent arteriole (unique)
Divide to form peritubular capillaries or some have vasa recta
Peritubular venule, interlobar vein and renal vein exits kidney
Renal nerves are part of the sympathetic autonomic nervous
system
Most are vasomotor nerves regulating blood flow
Copyright 2009, John Wiley & Sons, Inc.
Blood supply of the kidneys
Copyright 2009, John Wiley & Sons, Inc.
The nephron – functional units of
kidney
2 parts
Renal corpuscle – filters blood plasma
Glomerulus – capillary network
Glomerular (Bowman’s) capsule – double-walled
cup surrounding glomerulus
Renal tubule – filtered fluid passes into
Proximal convoluted tubule
Descending and ascending loop of Henle
(nephron loop)
Distal convoluted tubule
Copyright 2009, John Wiley & Sons, Inc.
Nephrons
Renal corpuscle and both convoluted tubules in
cortex, loop of Henle extend into medulla
Distal convoluted tubule of several nephrons
empty into single collecting duct
Cortical nephrons – 80-85% of nephrons
Renal corpuscle in outer portion of cortex and short loops of
Henle extend only into outer region of medulla
Juxtamedullary nephrons – other 25-20%
Renal corpuscle deep in cortex and long loops of Henle
extend deep into medulla
Receive blood from peritubular capillaries and vasa recta
Ascending limb has thick and thin regions
Enable kidney to secrete very dilute or very concentrated urine
Copyright 2009, John Wiley & Sons, Inc.
The structure of nephrons and associated
blood vessels
Copyright 2009, John Wiley & Sons, Inc.
Histology of nephron and collecting duct
Glomerular capsule
Visceral layer has podocytes that wrap projections
around single layer of endothelial cells of glomerular
capillaries and form inner wall of capsule
Parietal layer forms outer wall of capsule
Fluid filtered from glomerular capillaries enters capsular
(Bowman’s) space
Copyright 2009, John Wiley & Sons, Inc.
Histology of a renal corpuscle
Copyright 2009, John Wiley & Sons, Inc.
Renal tubule and collecting duct
Proximal convoluted tubule cells have microvilli with
brush border – increases surface area
Juxtaglomerular appraratus helps regulate blood
pressure in kidney
Macula densa – cells in final part of ascending loop of Henle
Juxtaglomerular cells – cells of afferent and efferent
arterioles contain modified smooth muscle fibers
Last part of distal convoluted tubule and collecting duct
Principal cells – receptors for antidiuretic hormone (ADH)
and aldosterone
Intercalated cells – role in blood pH homeostasis
Copyright 2009, John Wiley & Sons, Inc.
Overview of renal physiology
1.
2.
3.
Glomerular filtration
Water and most solutes in blood plasma move across the wall of
the glomerular capillaries into glomerular capsule and then renal
tubule
Tubular reabsorption
As filtered fluid moves along tubule and through collecting duct,
about 99% of water and many useful solutes reabsorbed –
returned to blood
Tubular secretion
As filtered fluid moves along tubule and through collecting duct,
other material secreted into fluid such as wastes, drugs, and
excess ions – removes substances from blood
Solutes in the fluid that drains into the renal pelvis remain in the
fluid and are excreted
Excretion of any solute = glomerular filtration + secretion - reabsorption
Copyright 2009, John Wiley & Sons, Inc.
Structures and functions of a nephron
Renal tubule and collecting duct
Renal corpuscle
Afferent
arteriole
Glomerular
capsule
Urine
(contains
excreted
substances)
Fluid in
renal tubule
1 Filtration from blood
plasma into nephron
2 Tubular reabsorption
from fluid into blood
Efferent
arteriole
Peritubular capillaries
Copyright 2009, John Wiley & Sons, Inc.
3 Tubular secretion
from blood into fluid
Blood
(contains
reabsorbed
substances)
Glomerular filtration
Glomerular filtrate – fluid that enters capsular space
Daily volume 150-180 liters – more than 99% returned to
blood plasma via tubular reabsorption
Filtration membrane – endothelial cells of glomerular
capillaries and podocytes encircling capillaries
Permits filtration of water and small solutes
Prevents filtration of most plasma proteins, blood cells and
platelets
3 barriers to cross – glomerular endothelial cells
fenestrations, basal lamina between endothelium and
podocytes and pedicels of podocytes create filtration slits
Volume of fluid filtered is large because of large surface
area, thin and porous membrane, and high glomerular
capillary blood pressure
Copyright 2009, John Wiley & Sons, Inc.
The filtration membrane
Copyright 2009, John Wiley & Sons, Inc.
Podocyte of visceral
layer of glomerular
(Bowman’s) capsule
Filtration slit
Pedicel
1
Fenestration (pore) of glomerular
endothelial cell: prevents filtration of
blood cells but allows all components
of blood plasma to pass through
2
Basal lamina of glomerulus:
prevents filtration of larger proteins
3
Slit membrane between pedicels:
prevents filtration of medium-sized
proteins
(a) Details of filtration membrane
Pedicel of podocyte
Filtration slit
Basal lamina
Lumen of glomerulus
Fenestration (pore) of
glomerular endothelial cell
(b) Filtration membrane
TEM 78,000x
Net filtration pressure
Net filtration pressure (NFP) is the total pressure
that promotes filtration
NFP = GBHP – CHP – BCOP
Glomerular blood hydrostatic pressure is the blood
pressure of the glomerular capillaries forcing water and
solutes through filtration slits
Capsular hydrostatic pressure is the hydrostatic pressure
exerted against the filtration membrane by fluid already in
the capsular space and represents “back pressure”
Blood colloid osmotic pressure due to presence of proteins
in blood plasma and also opposes filtration
Copyright 2009, John Wiley & Sons, Inc.
The pressures that drive glomerular
filtration
Copyright 2009, John Wiley & Sons, Inc.
1 GLOMERULAR BLOOD
HYDROSTATIC PRESSURE
(GBHP) = 55 mmHg
2 CAPSULAR HYDROSTATIC
PRESSURE (CHP) = 15 mmHg
3 BLOOD COLLOID
OSMOTIC PRESSURE
(BCOP) = 30 mmHg
Afferent arteriole
Proximal convoluted tubule
Efferent
arteriole
NET FILTRATION PRESSURE (NFP)
=GBHP – CHP – BCOP
= 55 mmHg 15 mmHg 30 mmHg
= 10 mmHg
Glomerular
(Bowman's) Capsular
capsule
space
Glomerular filtration
Glomerular filtration rate – amount of filtrate
formed in all the renal corpuscles of both
kidneys each minute
Homeostasis requires kidneys maintain a
relatively constant GFR
Too high – substances pass too quickly and are not
reabsorbed
Too low – nearly all reabsorbed and some waste
products not adequately excreted
GFR directly related to pressures that determine
net filtration pressure
Copyright 2009, John Wiley & Sons, Inc.
3 Mechanisms regulating GFR
Renal autoregulation
1.
Kidneys themselves maintain constant renal blood flow
and GFR using
Myogenic mechanism – occurs when stretching triggers
contraction of smooth muscle cells in afferent arterioles –
reduces GFR
Tubuloglomerular mechanism – macula densa provides
feedback to glomerulus, inhibits release of NO causing
afferent arterioles to constrict and decreasing GFR
Copyright 2009, John Wiley & Sons, Inc.
Tuboglomerular feedback
Copyright 2009, John Wiley & Sons, Inc.
Mechanisms regulating GFR
Neural regulation
2.
Kidney blood vessels supplied by sympathetic ANS fibers that
release norepinephrine causing vasoconstriction
Moderate stimulation – both afferent and efferent arterioles
constrict to same degree and GFR decreases
Greater stimulation constricts afferent arterioles more and
GFR drops
Hormonal regulation
3.
Angiotensin II reduces GFR – potent vasoconstrictor of both
afferent and efferent arterioles
Atrial natriuretic peptide increases GFR – stretching of atria
causes release, increases capillary surface area for filtration
Copyright 2009, John Wiley & Sons, Inc.
Tubular reabsorption and tubular secretion
Reabsorption – return of most of the filtered
water and many solutes to the bloodstream
About 99% of filtered water reabsorbed
Proximal convoluted tubule cells make largest
contribution
Both active and passive processes
Secretion – transfer of material from blood
into tubular fluid
Helps control blood pH
Helps eliminate substances from the body
Copyright 2009, John Wiley & Sons, Inc.
Reabsorption routes and transport mechanisms
Reabsorption routes
Paracellular reabsorption
Between adjacent tubule cells
Tight junction do not completely seal off interstitial fluid from
tubule fluid
Passive
Transcellular reabsorption – through an individual cell
Transport mechanisms
Reabsorption of Na+ especially important
Primary active transport
Secondary active transport
Symporters, antiporters
Transport maximum (Tm)
Sodium-potassium pumps in basolateral membrane only
Upper limit to how fast it can work
Obligatory vs. facultative water reabsorption
Copyright 2009, John Wiley & Sons, Inc.
Reabsorption routes: paracellular reabsorption and
transcellular reabsorption
Copyright 2009, John Wiley & Sons, Inc.
Reabsorption and secretion in proximal
convoluted tubule (PCT)
Largest amount of solute and water reabsorption
Secretes variable amounts of H+, NH4+ and urea
Most solute reabsorption involves Na+
Solute reabsorption promotes osmosis – creates osmotic gradient
Symporters for glucose, amino acids, lactic acid, water-soluble
vitamins, phosphate and sulfate
Na+ / H+ antiporter causes Na+ to be reabsorbed and H+ to be secreted
Aquaporin-1 in cells lining PCT and descending limb of loop of Henle
As water leaves tubular fluid, solute concentration increases
Urea and ammonia in blood are filtered at glomerulus and secreted
by proximal convoluted tubule cells
Copyright 2009, John Wiley & Sons, Inc.
Reabsorption and secretion in the
proximal convoluted tubule
Copyright 2009, John Wiley & Sons, Inc.
Reabsorption in the loop of Henle
Chemical composition of tubular fluid quite different from
filtrate
Glucose, amino acids and other nutrients reabsorbed
Osmolarity still close to that of blood
Reabsorption of water and solutes balanced
For the first time reabsorption of water is NOT
automatically coupled to reabsorption of solutes
Independent regulation of both volume and osmolarity of
body fluids
Na+-K+-2Cl- symporters function in Na+ and Cl- reabsorption
– promotes reabsorption of cations
Little or no water is reabsorbed in ascending limb –
osmolarity decreases
Copyright 2009, John Wiley & Sons, Inc.
Na+–K+-2Cl- symporter in the thick
ascending limb of the loop of Henle
Copyright 2009, John Wiley & Sons, Inc.
Reabsorption and secretion in the late distale
convoluted tubule and collecting duct
Reabsorption on the early distal convoluted tubule
Na+-Cl- symporters reabsorb Na+ and ClMajor site where parathyroid hormone stimulates
reabsorption of Ca+ depending on body’s needs
Reabsorption and secretion in the late distal
convoluted tubule and collecting duct
90-95% of filtered solutes and fluid have been returned by
now
Principal cells reabsorb Na+ and secrete K+
Intercalated cells reabsorb K+ and HCO3- and secrete H+
Amount of water reabsorption and solute reabsorption and
secretion depends on body’s needs
Copyright 2009, John Wiley & Sons, Inc.
Hormonal regulation of tubular reabsorption
and secretion
Angiotensin II - when blood volume and blood pressure
decrease
Aldosterone - when blood volume and blood pressure
decrease
Decreases GFR, enhances reabsorption of Na+, Cl- and water
in PCT
Stimulates principal cells in collecting duct to reabsorb more
Na+ and Cl- and secrete more K+
Parathyroid hormone
Stimulates cells in DCT to reabsorb more Ca2+
Copyright 2009, John Wiley & Sons, Inc.
Regulation of facultative water reabsorption
by ADH
Antidiuretic hormone (ADH
or vasopressin)
Increases water
permeability of cells by
inserting aquaporin-2 in last
part of DCT and collecting
duct
Atrial natriuretic peptide
(ANP)
Large increase in blood
volume promotes release of
ANP
Decreases blood volume
and pressure by inhibiting
reabsorption of Na+ and
water in PCT and collecting
duct, suppress secretion of
ADH and aldosterone
Copyright 2009, John Wiley & Sons, Inc.
Production of dilute and concentrated
urine
Even though your fluid intake can be highly
variable, total fluid volume in your body
remains stable
Depends in large part on the kidneys to
regulate the rate of water loss in urine
ADH controls whether dilute or concentrated
urine is formed
Absent or low ADH = dilute urine
Higher levels = more concentrated urine through
increased water reabsorption
Copyright 2009, John Wiley & Sons, Inc.
Formation of dilute urine
Glomerular filtrate has same osmolarity as blood
300 mOsm/liter
Fluid leaving PCT is isotonic to plasma
When dilute urine is being formed, the osmolarity
of fluid increases as it goes down the descending
loop of Henle, decreases as it goes up the
ascending limb, and decreases still more as it
flows through the rest of the nephron and
collecting duct
Copyright 2009, John Wiley & Sons, Inc.
Formation of dilute urine
Osmolarity of interstitial fluid of
renal medulla becomes
greater, more water is
reabsorbed from tubular fluid
so fluid become more
concentrated
Water cannot leave in thick
portion of ascending limb but
solutes leave making fluid
more dilute than blood plasma
Additional solutes but not
much water leaves in DCT
Low ADH makes late DCT and
collecting duct have low water
permeability
Copyright 2009, John Wiley & Sons, Inc.
Formation of concentrated urine
Urine can be up to 4 times more concentrated than
blood plasma
Ability of ADH depends on presence of osmotic
gradient in interstitial fluid of renal medulla
3 major solutes contribute – Na+, Cl-, and urea
2 main factors build and maintain gradient
Differences in solute and water permeability in
different sections of loop of Henle and collecting
ducts
Countercurrent flow of fluid though descending and
ascending loop of Henle and blood through
ascending and descending limbs of vasa recta
Copyright 2009, John Wiley & Sons, Inc.
Countercurrent multiplication
Process by which a progressively increasing osmotic gradient is
formed as a result of countercurrent flow
Long loops of Henle of juxtamedullary nephrons function as
countercurrent multiplier
Symporters in thick ascending limb of loop of Henle cause buildup
of Na+ and Cl- in renal medulla, cells impermeable to water
Countercurrent flow establishes gradient as reabsorbed Na+ and
Cl- become increasingly concentrated
Cells in collecting duct reabsorb more water and urea
Urea recycling causes a buildup of urea in the renal medulla
Long loop of Henle establishes gradient by countercurrent
multiplication
Copyright 2009, John Wiley & Sons, Inc.
Countercurrent exchange
Process by which solutes and water are passively
exchanged between blood of the vasa recta and
interstitial fluid of the renal medulla as a result of
countercurrent flow
Vasa recta is a countercurrent exchanger
Osmolarity of blood leaving vasa recta is only
slightly higher than blood entering
Provides oxygen and nutrients to medulla without
washing out or diminishing gradient
Vasa recta maintains gradient by countercurrent
exchange
Copyright 2009, John Wiley & Sons, Inc.
Mechanism of urine concentration in
long-loop juxtamedullary nephrons
Copyright 2009, John Wiley & Sons, Inc.
Vasa
recta
Loop of
Henle
Juxtamedullary nephron
and its blood supply
together
Glomerular (Bowman’s) capsule
H2O
Na+CI–
Blood flow
Glomerulus
Afferent
arteriole
Distal convoluted tubule
Presense of Na+-K+-2CI–
symporters
Interstitial
fluid in
renal cortex
200
HO
H2O 2
Efferent
arteriole
300
300
Collecting
duct
300
300
100
H2O
320
Na+CI–
400
Interstitial fluid
in renal medulla
380
200
H2O
400
3 Principal cells in
Osmotic
gradient
H2O
collecting duct
reabsorb more
water when ADH
is present
Na+CI–
400
500
H2O
600
H2O
580
600
320
300
H2O
Proximal
convoluted
tubule
Flow of tubular fluid
400
H2O
Na+CI–
600
1 Symporters in thick
ascending limb cause
buildup of Na+ and Cl–
800
700
780
600
Urea
H2O
980
1000
H2O
800
800
H2O
800
900
4 Urea recycling
1000
causes buildup
of urea in the
renal medulla
Na+CI–
H2O
1000
1100
H2O
1200
2 Countercurrent flow
through loop of Henle
establishes an osmotic
gradient
1200
Loop of Henle
1200
Papillary
duct
1200
Concentrated urine
(a) Reabsorption of Na+CI– and water in a long-loop juxtamedullary nephron
1200
(b) Recycling of salts and urea in the vasa recta
Summary of filtration, reabsorption, and secretion
in the nephron and collecting duct
Copyright 2009, John Wiley & Sons, Inc.
Evaluation of kidney function
Urinalysis
Analysis of the volume and physical, chemical and
microscopic properties of urine
Water accounts for 95% of total urine volume
Typical solutes are filtered and secreted
substances that are not reabsorbed
If disease alters metabolism or kidney function,
traces if substances normally not present or
normal constituents in abnormal amounts may
appear
Copyright 2009, John Wiley & Sons, Inc.
Evaluation of kidney function
Blood tests
Blood urea nitrogen (BUN) – measures blood nitrogen that
is part of the urea resulting from catabolism and
deamination of amino acids
Plasma creatinine results from catabolism of creatine
phosphate in skeletal muscle – measure of renal function
Renal plasma clearance
More useful in diagnosis of kidney problems than above
Volume of blood cleared of a substance per unit time
High renal plasma clearance indicates efficient excretion of
a substance into urine
PAH administered to measure renal plasma flow
Copyright 2009, John Wiley & Sons, Inc.
Urine transportation, storage, and
elimination
Ureters
Each of 2 ureters transports urine from renal
pelvis of one kidney to the bladder
Peristaltic waves, hydrostatic pressure and gravity
move urine
No anatomical valve at the opening of the ureter
into bladder – when bladder fills it compresses the
opening and prevents backflow
Copyright 2009, John Wiley & Sons, Inc.
Ireters, urinary bladder, and urethra in a
female
Copyright 2009, John Wiley & Sons, Inc.
Urinary bladder and urethra
Urinary bladder
Hollow, distensible muscular organ
Capacity averages 700-800mL
Micturition – discharge of urine from bladder
Combination of voluntary and involuntary muscle contractions
When volume increases stretch receptors send signals to
micturition center in spinal cord triggering spinal reflex –
micturition reflex
In early childhood we learn to initiate and stop it voluntarily
Urethra
Small tube leading from internal urethral orifice in floor of
bladder to exterior of the body
In males discharges semen as well as urine
Copyright 2009, John Wiley & Sons, Inc.
Comparison between female and male
urethras
Copyright 2009, John Wiley & Sons, Inc.
End of Chapter 26
Copyright 2009 John Wiley & Sons, Inc.
All rights reserved. Reproduction or translation of this
work beyond that permitted in section 117 of the 1976
United States Copyright Act without express
permission of the copyright owner is unlawful.
Request for further information should be addressed to
the Permission Department, John Wiley & Sons, Inc.
The purchaser may make back-up copies for his/her
own use only and not for distribution or resale. The
Publishers assumes no responsibility for errors,
omissions, or damages caused by the use of theses
programs or from the use of the information herein.
Copyright 2009, John Wiley & Sons, Inc.