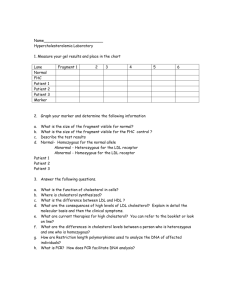
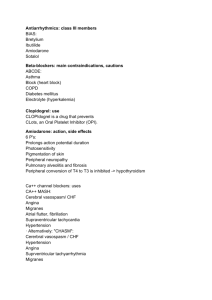
Cardiovascular I
advertisement

Control of Cardiovascular Function, Disorders of Blood Flow and Blood Pressure, Hyperlipidemia, and Artherosclerosis 1 INTRODUCTION 2 Sympathetic Nervous System 3 Location Response to agonist or neurotransmitter Alpha-1 – activated with norepi Arteries and veins Constriction Bladder neck (internal sphincter) Constriction Alpha-2 – activated with norepi Central nervous system Inhibits sympathetic outflow Beta-1 – activated with norepi Heart, SA node Increases heart rate (positive chronotropic effect) Heart, AV node Increases speed of conduction (positive dromotropic effect) Heart, ventricular muscle Increased contractility (positive inotropic effect) Kidney Release of renin - Leads to thicker blood and vasoconstriction (through angiotensin II) - ultimately leads to increased blood pressure - do not need to pee Beta-2 – activated with only epi Arterioles in skeletal muscle beds Dilation to bring more blood to muscles Bronchi Dilation Uterus Relaxation 4 Alpha-1 Receptors 5 Alpha-1 Receptors • Norepinephrine and epinephrine • Vasoconstriction of arterioles and veins • Vasoconstriction of the bladder – Prevents urination 6 Alpha-2 Receptors 7 Alpha-2 Receptors • Norepinephrine and epinephrine • Inhibits sympathetic outflow 8 Beta-1 Receptors 9 Beta-1 Receptors • Norepinephrine and epinephrine • Increases heart rate • Increases speed of conduction • Increases heart contractility • Activates the RAAS to increase blood pressure 10 Beta-2 Receptors 11 Beta-2 Receptors • Epinephrine only • Arterial dilation • Bronchodilation • Relaxation of the uterus 12 Outline of the Lecture 13 Outline of the Lecture • Review of Hemodynamics – Blood vessel structure, function – Regulation of cardiac output – Mechanisms of blood pressure regulation • Disorders of blood pressure – Hypertension – Orthostatic hypotension • Drugs that affect blood pressure • Disorders of arterial circulation – Hyperlipidemia, atherosclerorosis • Drugs that lower LDL cholesterol 14 Pulmonary and Systemic Circulation Description 15 Pulmonary and Systemic Circulation Description • Likes this diagram a lot • Depicts the circulatory system as two systems that are in tandem and are connected to each other in the heart • Left ventricle – aorta – systemic circulation – right atria – right ventricle – pulmonary artery – pulmonary circulation 16 Pulmonary and Systemic Circulation Diagram 17 Pulmonary and Systemic Circulation Diagram 18 Baxter Corp. (1999) Differences in the Pulmonary and the Systemic Systems 19 Differences in the Pulmonary and the Systemic Systems • PULMONARY • Low pressure system (MPAP 12 mmHg) • Good for gas exchange • SYSTEMIC • High pressure system (MAP 90-100 mmHg) • Good for distant transport, against gravity so the pressure needs to be higher 20 How Does Blood Get Back to the Heart? Diagram 21 How Does Blood Get Back to the Heart? 22 Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p 461 How Does Blood Get Back to the Heart? Description 23 How Does Blood Get Back to the Heart? Description • Pressure is high in the aorta, low in the large arteries, even lower in the arterioles, there is a big drop in capillaries, and gets even lower as it returns into the right atria – It is good to have a negative pressure in the right atria because you will be sucking the blood into the heart, which is a good thing 24 Principles of Blood Flow 25 Principles of Blood Flow • Hemodynamics • Heart is an intermittent pump, blood flow is pulsatile – This is not true if the person has a continuous heart pump 26 Factors Governing the Function of the Cardiovascular System 27 Factors Governing the Function of the Cardiovascular System • Volume • Pressure • Resistance • Flow 28 Determinants of Blood Pressure 29 Determinants of Blood Pressure BP = CO X Peripheral vascular resistance CO = SV X HR • What determines peripheral vascular resistance? 30 Resistance of a Tube Description 31 Resistance of a Tube Description • Peripheral vascular resistance – the resistance to flow in the vascular tree • The radius of the tube is a huge factor in delivering flow because it is done to the fourth power!!! – Changing the radius of the tube just a little bit greatly changes the resistance of the flow and thus the flow itself 32 Resistance of a Tube Diagram 33 Resistance of a Tube Diagram Big factor! Porth, Pathophysiology, Concepts of Altered Health States, 7th ed., 2005, Lippincott, p. 452. Also see p 322, point 2 in Porth, Essentials 34 Volume and Pressure Distribution Description 35 Volume and Pressure Distribution Description • When we get to the arterioles, there is a huge drop in pressure – The degree of constriction of the arterioles determines the peripheral vascular resistance, which then makes it important in determining blood pressure • 4% of blood is in the left ventricle, 16% in the arteries, 4% in the capillaries, and 64% in the veins • Veins are capacitance vessels – The veins serve as a storage place for the blood – If we want to increase cardiac output quickly, the veins can constrict and return the blood to the heart, sending a bolus to the heart to increase the stroke volume and thus the cardiac output 36 Volume and Pressure Distribution Diagram 37 Volume and Pressure Distribution Diagram Arteriolar tone determines systemic vascular resistance Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 321. 38 Pulmonary and Circulatory Systems Diagram, Lehne 39 Pulmonary and Circulatory Systems Diagram, Lehne Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p 461 40 Layers of the Blood Vessels 41 Layers of the Blood Vessels • Intima- elastic layer • Media- smooth muscle for diameter control (innervated by the SNS with alpha receptors) – Alpha receptors cause constriction of the vessels – The arteries have more smooth muscle than the veins • Externa- fibrous and connective tissue for support Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 338 42 Resistance Arterioles Maintain Blood Pressure 43 Resistance Arterioles Maintain Blood Pressure • Arteries have abundant smooth muscle. The diameter of the artery/arteriole is determined by the degree of contraction of the smooth muscle, which is mediated by the SNS (alpha receptors). • The SNS maintains tone in the arteries 44 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 338 Blood Vessels and the Peripheral Circulation 45 Blood Vessels and the Peripheral Circulation • Blood vessels are not pipes – Pipes cannot change their diameters, while blood vessels can • Blood vessels are dynamic structures – They constrict and relax to adjust blood flow to meet varying needs of tissues/organs • The heart, brain, liver, and kidney require large continuous flow – There are no alpha receptors on blood vessels going to the brain because we do not want to ever constrict then • Skin and skeletal muscle require varying flow of blood, depending on the situation – Ex. if you just ate, you will need a lot of blood going to your digestive tract 46 Arteries and Arterioles 47 Arteries and Arterioles • Elasticity allows for stretching during systole • Arterioles have abundant smooth muscle • Arterioles are the major resistance vessels for circulatory the system and basically determine the systemic vascular resistance • Sympathetic fibers innervate arterioles cause them to constrict/relax as needed to maintain BP (alpha receptors) 48 Veins and Venules 49 Veins and Venules • Collect blood from capillaries and carry it back to the heart • Enlarge and store large quantities of blood and are then able to return the stored blood to the heart when needed • Contract/expand to accommodate varying amounts • Innervated by SNS (alpha receptors) • Venous constriction can increase the preload to the heart by conducting stored blood into the vena cava – This will increase the cardiac output 50 Veins 51 Veins • Valves prevent retrograde flow – Incompetent valves in venous varicosities – As we age, the valves may become incompetent • Skeletal muscles help compress veins in “milking manner” up to heart • Low pressure system – Pressure in venules is ~10 mm Hg and in the vena cava ~0 mmHg Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 339. 52 Endothelial Cells 53 Endothelial Cells •Endothelial cells line all blood vessels. •They are normally quite smooth and permit laminar (uninterrupted) blood flow. •They also form a tight barrier in larger vessels •Capillaries are more permissive of small molecules exiting and entering the vascular system because they possess fenestrations54 Capillaries 55 Capillaries • Single cell-thick vessels that connect arterial and venous segments • Wall composed of a single layer of endothelial cells surrounded by a basement membrane – Do not have smooth muscle • In most vascular beds, capillaries have fenestrations that allow passage of water and small molecules but not large proteins. • The basement membrane between the endothelial cells and the outside of the capillaries is very important Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 341. 56 Vascular Smooth Muscle and Sympathetic Nervous System 57 Vascular Smooth Muscle and Sympathetic Nervous System • Norepinephrine-activated alpha receptors cause calcium channels in vascular smooth muscle to open, which produces vasoconstriction • In some vascular beds, beta-2 receptors promote vasodilation by decreasing calcium. • Calcium Causes Contraction in vascular smooth muscle – The more calcium that is present inside the cell, the more contraction is present • Calcium channel blockers prevent vasoconstriction – Prevents calcium from going through the calcium channel so the calcium cannot cause contraction 58 Perfusion of Organs 59 Perfusion of Organs • Tissue blood flow to a given organ is regulated on a minute-to-minute basis in relation to tissue needs • Neural mechanisms regulate cardiac output and systemic vascular resistance (BP) to support local mechanisms • Local control includes preferential vasoconstriction or vasodilation mediated by the SNS or by intrinsic mechanisms within the organ. 60 Tissue Factors Contributing to Local Control of Blood Flow 61 Tissue Factors Contributing to Local Control of Blood Flow • Factors are released from an organ when it has too much or too little blood flow. • In order to increase blood flow – Histamine • Would cause dilation of the vessel • Decrease blood flow – Serotonin • Would cause constriction of the vessel • Are these correct?* 62 Endothelial Control of Vascular Smooth Muscle 63 Endothelial Control of Vascular Smooth Muscle • The endothelium produces factors that act on smooth muscle to produce vasoconstriction or vasodilation • Vasodilating substances – Nitric Oxide • Vasoconstricting substances – Angiotensin II, Prostaglandins, Endothelins • The circulatory system is a dynamic structure that works to send blood to different organs that need more or less blood 64 Functional Anatomy of the Heart 65 Functional Anatomy of the Heart Pericardium: •Sac around heart •Normally, has a little bit of fluid in it in order to make movement easier A “virtual space” which can become fluid or blood-filled (pericardial effusion). Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 328. 66 Contraction: Actin and Myosin Binding Description 67 Contraction: Actin and Myosin Binding Description • Actin and myosin overlap and grab onto each other • Calcium is what makes this process work 68 Contraction: Actin and Myosin Binding Diagram 69 Contraction: Actin and Myosin Binding Diagram Spirito et al., NEJM 336, pg 775, 1997 http://www.sci.sdsu.edu/movies/actin_myosin_gif.html 70 Heart Valves Keep Blood Flow Unidirectional Diagram 71 Heart Valves Keep Blood Flow Unidirectional Semilunar valves A-V valves 72 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 329. Function of Heart Valves 73 Function of Heart Valves • Major function of heart valves: Forward direction of blood flow • Open and shut in order to keep blood moving forward in an unidirectional manner 74 Semilunar Valves 75 Semilunar Valves • Control blood flow out of ventricles • Aortic valve • Pulmonic valve 76 Atroventricular Valves 77 Atroventricular Valves • Control blood flow between atria and ventricles • Tricuspid valve • Mitral valve 78 Cardiac Conduction System 79 Cardiac Conduction System • The conduction system stimulates the myocardium to contract and pump blood • The conduction system controls the rhythm of the heart. • Heart has two conduction systems – One controls atrial activity – One that controls ventricular activity – The two systems communicate when the impulse that causes atrial contraction travels to the ventricular system via the A-V node 80 Conduction System Diagram 81 Conduction System Diagram 82 SA Node 83 SA Node • Pacemaker of the heart – Spontaneously depolarizes • Impulses originate here • Located in posterior wall RA • Causes the atria to contract • Fires at 60 -100 bpm if it is not innervated by anything – Can be influenced by the SNS and PNS • Rate is determined by the autonomic nervous system – Increase HR: Sympathetic nervous system---NE---beta-1 receptors – Decrease HR: Parasympathetic nervous system ---acetylcholine--muscarinic receptors 84 AV Node 85 AV Node • Connects the atria and ventricles, provides one way conduction • The speed of conduction of the AV node is much slower than the fibers in the atria or the ventricle • At the AV node, the signal stops – Promotes filling of the ventricles before ejection • Speed of conduction in the AV node is determined by the ANS – – The SNS can speed up conduction and make the pause shorter (beta-1) The PNS can slow conduction down and make the pause longer (muscarinic receptor) • Can assume pacemaker function if SA fails to discharge – Can depolarize on its own and cause the ventricles to contract – Fires at 40 -60 bpm 86 Purkinje Fibers 87 Purkinje Fibers • Supply the ventricles – Spread the impulse throughout the ventricular muscle • Large fibers, rapid conduction for swift and efficient ejection of blood from heart • Assume pacemaker of ventricles if AV fails – Intrinsic rate is 15-40 bpm Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 331. 88 ECG 89 ECG • Electrical events recorded – Transmitted to the skin via conduction • Electrical events precede mechanical events; know what they represent! – P – – – – • Atrial depolarization Pause caused by the AV node QRS • Ventricular depolarization T • Ventricular repolarization U wave • The repolarization of the atria Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p.331 & 333. 90 Cardiac Cycle 91 Cardiac Cycle • Term used to describe the rhythmic pumping action of heart • Cycle divided into 2 parts – Systole: period during which ventricles are contracting – Diastole: period during which ventricles are relaxed, filling with blood • Simultaneous changes occur in pressure (LA,LV, aorta), ventricular volume, ECG, heart sounds during cardiac cycle 92 The Wiggers Diagram 93 The Wiggers Diagram Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 334. 94 The Wiggers Diagram Description of Pressure 95 The Wiggers Diagram Description of Pressure • • • • • • • • • At the beginning of systole, the pressure in the left ventricle is low, starts to contract (at this point, the aortic and the mitral valve are both closed), as the ventricle is contracting, pressure builds in the ventricle (isovolumetric contraction) The dotted line at the beginning is the aortic pressure The pressure in the ventricle and aorta are the same Pressure in the ventricle forces the aorta to open Pressure in the ventricle rises further until it is maximally contracted Pressure in the aortic route and in the ventricle are equal at this time because the pressure is the same When the ventricle pressure is lower than in the aorta, the aortic valve closes As the ventricle is relaxing, pressure in the ventricle drops a lot Isometric relaxation period – Pressure in low • Diastole – The ventricle is relaxed – Ventricle pressure is staying low – Volume is increasing because the ventricle is filling • • Fills passively because the mitral valve opens Pressure between the atria and the ventricle are the same – The atria contracts to force more blood into the ventricle 96 The Wiggers Diagram Other Elements 97 The Wiggers Diagram Other Elements • The electrical stimuli come before the contractions or relaxations because the stimulation causes the contraction • The little increase in atrial volume at the end is called the atrial kick – Contributes very little to the volume in the left ventricle • May be important if the heart rate is really fast so the diastole is slow – May be important to end more to the volume • Important in people with heart rate who need the kick to help the ventricles fill more • At the middle is volume • EKG • Heart sounds 98 Ventricular Systole Diagram 99 Ventricular Systole Diagram 100 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 334. Ventricular Systole Description 101 Ventricular Systole Description • Isovolumic (isometric) contraction • Ejection period. 102 Ventricular Systole Isovolumic (metric) Contraction 103 Ventricular Systole Isovolumic (metric) Contraction • Closure of AV valves (S1), all valves closed. • No change in ventricular volume • Ventricles contract • When ventricular pressures > aortic and pulmonary pressures, semilunar valves open, leading to the ejection period 104 Ventricular Systole Ejection Period 105 Ventricular Systole Ejection Period • Stroke volume ejected. • Ventricles contract, then relax. • Intraventricular pressures and become less than pressures in aorta and pulmonary arteries • Blood from large arteries flows back toward ventricles and aortic/pulmonic valves shut (S2). 106 Ventricular Diastole Diagram 107 Ventricular Diastole Diagram 108 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 334. Ventricular Diastole Description 109 Ventricular Diastole Description • Ventricular relaxation and filling • Isovolumic (isometric) relaxation • Rapid filling period 110 Ventricular Diastole Isovolumic (metric) Relaxation 111 Ventricular Diastole Isovolumic (metric) Relaxation • Semilunar valves closed • Ventricles relaxed • No change in ventricular volume, but ventricular pressure until it is less than atrial pressures. • AV valves open, blood from atria enters ventricles, leading to rapid filling phase 112 Ventricular Diastole Rapid Filling Phase 113 Ventricular Diastole Rapid Filling Phase • Most ventricular filling in first third of diastole (S3) • During the last third, atria contract (atrial kick). 114 Atrial Contraction 115 Atrial Contraction • Last third of ventricular diastole • Gives additional thrust to ventricular filling • Important during tachycardia or when heart disease impairs ventricular filling – May not be important in a person with a normal heart, especially at physiologic heart rates. • Fourth heart sound (S4), when present, occurs when atria contract – Cannot always hear the S4 heart sound 116 Cardiac Output 117 Cardiac Output • Cardiac output (CO) – Amount of blood the heart pumps/minute – 3.5 - 8.0 L/minute • In athletes, this could be much higher • Stroke volume (SV) – Amount of blood the heart pumps each beat – 70 ml/beat • CO = SV x HR • CO varies with body activities. – Ex. sleeping vs. exercise • CO varies by changes in SV and/or HR – SV – when veins contract – HR – more beats lead to more blood being pumped out 118 Heart Rate 119 Heart Rate • Frequency with which blood is ejected from heart – One way to increase the cardiac output • As HR → CO • HR is increased by activation of beta-1 receptors and decreased by activation of muscarinic receptors on the SA node. • BUT as HR → diastolic filling time – This occurs when heartrate increases too fast or too much • diastolic filling time may SV and CO • Tachycardia can be dangerous because the heart may not have time to fill adequately → CO 120 Equation for Cardiac Output 121 122 Stroke Volume Components 123 Stroke Volume Components • Preload – the amount of blood that is returned to the heart from the veins – Ventricular filling (volume) • Afterload – the pressure that the heart must press against in order to get the blood out – Pumping function – Resistance to ejection of blood from heart • Contractility – how hard is the heart contracting – Pumping function of heart 124 Preload (“Volume”) 125 Preload (“Volume”) • Represents the volume of blood the heart must pump with each beat – Ex. if the veins return 100mL to the heart and the heart does not pump out 100mL, the blood must stay in the heart, which is bad • What the veins return to the heart is what the heart must pump out • Largely determined by venous return and stretch of muscle fibers • Venous return – 64% of blood volume in veins – Venous constriction mediated by alpha-1 receptors 126 Preload: Frank-Starling Law of the Heart 127 Preload: Frank-Starling Law of the Heart •Actin, myosin filaments that overlap and create cross bridge attachments, which leads to contraction of cardiac muscle 128 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 336. Preload: Frank-Starling Law of the Heart Description 129 Preload: Frank-Starling Law of the Heart Description • An intrinsic property of the heart • The actin and myosin filaments must overlap in order for the contraction of cardiac muscle – They may overlap a little, optimally, or too much • Law – there is an optimal degree of overlap – This is determined by the end diastolic filling of the heart – If there is a little bit of volume in the heart, there is a lot of overlap and good contractility, but once the filaments slide, they cannot slide any more • This means that there is not a lot of extra space to end into, so filaments cannot contract a lot – Optimal overlap leads to the best contractility – If you overfill the heart and overstretch the filaments, then cardiac output declines because the filaments cannot touch • Not affected by the SNS – Has to do with the filling that the heart gets from the veins • Optimal overlap leads to increased SV beyond what we would expect from the increased filling 130 Implications of the Frank-Starling Law 131 Implications of the Frank-Starling Law • At normal volumes, as preload increases, stretch increases, which increases contractility. – CO goes up both because of the increased volume and increased contractility – The increase in contractility is independent of the SNS – it is an intrinsic property of the heart. • At high volumes, the cardiac muscle is overstretched and contractility decreases. – This is usually seen only in patients with heart failure (covered in CVII) who have fluid overload. 132 Afterload (“Resistance”) 133 Afterload (“Resistance”) • The heart must develop a pressure equal to the aortic pressure in order to open the valve • Afterload - the amount of pressure the heart must develop during the period of isovolumic contraction to open the aortic and pulmonic valves. • Without valve disease, afterload = diastolic pressure 134 Major Sources of Resistance 135 Major Sources of Resistance • Arterial pressures are the major sources of resistance – Right ventricle: • Pulmonary arterial pressure (low) – Left ventricle: • Systemic arterial pressure (high – equal to the diastolic BP in the absence of valve disease) 136 Diseases of the Semilunar Valves 137 Diseases of the Semilunar Valves • Disease of the aortic or pulmonic valves resistance – Stenosis/narrowing of the valve – This means that the heart has to develop an increased pressure to open the diseased valve. • The decrease in the valve will have a big impact on resistance, flow, and afterload because the radius is done to the fourth power – Diastolic hypertension also increases the pressure necessary to open the aortic valve. 138 Effect of Afterload on CO Diagram 139 Effect of Afterload on CO Diagram Guyton, 2006, Textbook of Medical Physiology, 11th ed.,Saunders, p. 114. 140 Effect of Afterload on CO Description 141 Effect of Afterload on CO Description • In normal people without disease, afterload has little impact on cardiac output – The ventricle can develop the pressures – Most important thing in determining CO is the preload • The heart pumps what it receives from the venous system • In a person with impaired contractility, this curve is shifted back to the left – At normal aortic pressures, there may be a decrease in cardiac output – With impaired contractility, afterload becomes important 142 Contractility 143 Contractility • Ability of the heart to change its force of contraction – The heart can contract harder when it is needed • Strongly influenced by number of calcium ions that are available to participate in the contractile process. – Determined by biochemical and biophysical properties that govern actin and myosin interactions in myocardial cells (Frank-Starling mechanism). – Activation of beta-1 receptors in the ventricles by norepinephrine (SNS) increases the availability of calcium ions and increases contractility. • The heart’s contractility can be stimulated by the sympathetic nervous system 144 Determinants of Blood Pressure 145 Determinants of Blood Pressure BP = CO X Peripheral vascular resistance CO = SV X HR 146 Mechanisms of BP Regulation Arterial Pressure 147 Mechanisms of BP Regulation Arterial Pressure • Arterial pressure must remain relatively constant as blood flow shifts from one area of body to another – Feedback mechanisms are short-term and long-term to regulate the blood pressure to remain constant • Method by which arterial pressure is regulated depends on whether short-term or long-term adaptation is needed 148 Mechanisms of BP Regulation ANS, RAAS, Kidneys 149 Mechanisms of BP Regulation ANS, RAAS, Kidneys • Autonomic nervous system – short-term regulation • RAAS (Renin-angiotensin-aldosterone system) – longer term regulation of blood pressure • Kidneys – control blood volume as well as the RAAS – a long-term mechanism of blood pressure control. – The kidneys are very important in long-term regulation of blood pressure 150 The Baroreceptor Reflex Diagram 151 The Baroreceptor Reflex Diagram Baroreceptors in the aortic arch and carotid artery Autonomic centers in the brainstem Cardiac muscle, cardiac conduction system, and vascular smooth muscle. 152 The Baroreceptor Reflex Description 153 The Baroreceptor Reflex Description • Baroreceptors sense pressure in the aortic arch and the carotid artery • Send information to the medulla in the autonomic centers in the brainstem • Send impulses to the heart and vessels to lower the blood pressure (if stimulation is too high) or to raise the blood pressure (if stimulation is too low) 154 The Sensory Components of the Baroreceptor Reflex – Chemo and Stretch Receptors 155 The Sensory Components of the Baroreceptor Reflex – Chemo and Stretch Receptors 156 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 364. ANS Regulation of BP – the Baroreceptor Reflex 157 ANS Regulation of BP – the Baroreceptor Reflex McCance & Heuther, 2002, Pathophysiology: The Biologic Basis for Disease in Adults & Children, Mosby, p.961 *Be sure you know which receptors are where!!! 158 ANS Regulation of BP – the Baroreceptor Reflex Description 159 ANS Regulation of BP – the Baroreceptor Reflex Description • Vagus nerve sends signals to the SA node to slow down the heart • SNS increases CO by increasing HR and contractility • SNS innervates arterioles to cause them to constrict (alpha) to raise blood pressure • SNS innervates veins to cause them to constrict to increase preload to increase CO • Baroreceptor reflex is happening all of the time • If blood pressure is too low, medulla instructs SNS centers in spinal cord to send information to the SA node through beta-1 receptors and the AV node to speed up the heart 160 Neurotransmitters 161 Neurotransmitters Porth, Pathophysiology, Concepts of Altered Health States, 7th ed., 2005, Lippincott, p. 1151. 162 Long-term Regulation of Blood Pressure 163 Long-term Regulation of Blood Pressure • Primarily controlled by kidneys • Neural mechanisms act rapidly, but cannot maintain their effectiveness over time so the kidneys are used • Kidneys’ control in long term is through regulation of Na+ and H20 balance – RAAS – Vasopressin 164 Renin-Angiotensin-Aldosterone System Diagram 165 Humoral Mechanisms: Reninangiotensinaldosterone system MUST KNOW THIS! Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 365. 166 Renin-Angiotensin-Aldosterone System Description 167 Renin-Angiotensin-Aldosterone System Description • When renal blood pressure falls, juxtaglomerular cells of the kidney acts on renin • Renin works on angiotensinogen • Angiotensinogen is converted to angiotensin I • Angiotensin I becomes angiotensin II – Angiotensin II constricts arteries and causes the adrenal cortex to release aldosterone • Aldosterone increases Na reabsorption, which increases water reabsorption 168 Vasopressin (Antidiuretic Hormone (ADH)) Diagram 169 Vasopressin (Antidiuretic Hormone (ADH)) 170 Porth, Pathophysiology, Concepts of Altered Health States, 7th ed., 2005, Lippincott, p. 756. Vasopressin (Antidiuretic Hormone (ADH)) Description 171 Vasopressin (Antidiuretic Hormone (ADH)) Description • ADH is released in result to changes in serum osmolality strength – When dehydrated, the serum osmolalitiy goes up, which stimulates the hypothalamus 172 The ANS and RAAS Systems Work in Concert to Maintain Blood Pressure 173 The ANS and RAAS systems work in concert to maintain blood pressure Porth, Pathophysiology, Concepts of Altered Health States, 7th ed., 2005, Lippincott, p. 756. 174 Which of the following is an important determinant of cardiac output in a normal person? 175 Which of the following is an important determinant of cardiac output in a normal person? 1. Afterload. 2. Heart rate. 3. Venous return (preload) 4. Total peripheral resistance. er ... ... rip h pe ta l To V en ou s H ea re tu rn rt ra te . d. rlo a ft e A - Component of afterload 25% 25% 25% 25% 176 You assess a patient’s pulse to be 40 bpm. He is not an athlete. Given this HR, the electrical impulses in the heart are probably originating from: 177 You assess a patient’s pulse to be 40 bpm. He is not an athlete. Given this HR, the electrical impulses in the heart are probably originating from: 25% 25% 25% 25% 1. 2. SA Node AV Node - Could be originating in the AV node 3. An ectopic atrial focus - This leads lead to increased heartrate r.. . P ur ki nj e ic to p A n ec A Fi be at r.. . od e N V N A - Could be originating from here as well od e Purkinje Fibers S 4. 178 Angiotensin II causes 179 Angiotensin II causes ab te ... ft he ar A ll o se d cr ea In oc as V R el ea se on s of tr ic ti. .. al d. .. 1. Release of aldosterone 2. Vasoconstriction of arterioles 3. Increased arterial blood pressure 4. All of the above o. .. 25% 25% 25% 25% 180 DISORDERS OF BLOOD PRESSURE REGULATION: HYPERTENSION AND ORTHOSTATIC HYPOTENSION 181 Orthostatic Hypotension 182 Orthostatic Hypotension • Abnormal drop in BP on assumption of the standing position – People can actually faint from this • Defined as a drop in systolic pressure > 20 mm Hg or drop in diastolic pressure > 10 mm Hg when going from lying to standing • In absence of normal circulatory reflexes and/or if blood volume is decreased, blood pools in lower part of the body when the standing position is assumed (decreased venous return), CO and blood flow to the brain is inadequate dizziness, syncope (fainting), or both • Occurs when the baroreceptor is not working properly or the person is dehydrated 183 Orthostatic Hypotension Diagram 184 Orthostatic Hypotension Diagram Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 374 185 Compensatory Mechanisms of Orthostatic Hypotension 186 Compensatory Mechanisms of Orthostatic Hypotension • Stand up, drop in blood pressure, compensated by increased venous return and increased heart rate – If you are taking a beta blocker is would prevent the heart rate from increasing – Alpha blocker would prevent the vasoconstriction • Dehydration is a big cause of people fainting 187 Causes of Orthostatic Hypotension 188 Causes of Orthostatic Hypotension • Reduced blood volume (dehydration) (reduced preload) – This is the most common cause of dizziness and fainting, especially in young, health people. • Drug-induced orthostatic hypotension – Impairment of venous return (reduced preload) (Ca2+ channel blockers) – Impairment of the baroreceptor reflex (beta blockers, alpha-1 blockers) – Diuretics (reduced preload) • Aging – sluggish reflexes, including the baroreceptor reflex • Bedrest – deconditioning • Disorders of the autonomic nervous system – Autonomic neuropathy – neuropathy of all of the nerves • The autonomic ones may be affected 189 Treatment of Orthostatic Hypotension 190 Treatment of Orthostatic Hypotension • Address the alleviating cause – Rehydrate, change medications • Help cope with disorder, prevent falls, injury – Gradual ambulation (sit on edge of bed, move legs) – Avoid venodilation (drinking ETOH; exercise in warm environment) – Maintain hydration 191 Hypertension Description 192 Hypertension Description • Common health problem in adults • A leading risk factor for cardiovascular disorders (myocardial infarction, heart failure, stroke, vascular disease) • More common in young men than young women, blacks compared with whites, in persons from lower socioeconomic groups, and with increasing age • Diabetics are more likely to have hypertension and it is more likely to lead to cardiovascular disease than in nondiabetics. 193 Primary Hypertension 194 Primary Hypertension • “Essential hypertension” • Chronic elevation of BP occurs without evidence of other disease • 90-95% of hypertension – Much more common than secondary hypertension 195 Secondary Hypertension 196 Secondary Hypertension • Elevation of BP occurs from some other disorder – Kidney disease – Chronic renal failure • Kidney thinks that it does not have enough blood flow, which activates the RAAS – Disorders of adrenocorticoid hormones (pheochromocytoma) 197 Hypertension Definitions 198 Hypertension Definitions • JNC-VII* (June 2003) – – – – “Prehypertension” (120-139/80-89) Stage I (140-159/90-99) Stage II (160-179/100-109) Stage III (>180/>110) *7th Report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure 199 Constitutional Risk Factors 200 Constitutional Risk Factors • Family history – Hereditary pattern unclear, genes not identified • Age related changes – BP higher with advancing age • Insulin resistance, metabolic syndrome, diabetes (especially type II) • Race – African Americans more prevalent, early onset, more severe; greater renal, CV damage – Less known about other races 201 Lifestyle Risk Factors 202 Lifestyle Risk Factors • Diet high in Na+ and saturated fats • Obesity – When people lose weight, a lot of times it result in their blood pressure decreasing • Physical inactivity • Excessive alcohol consumption • Oral contraceptives in predisposed women 203 Consequences of Hypertension 204 Consequences of Hypertension • Usually related to long term effects of HTN on other organs, “target organ damage”. • HTN seems to accelerate atherosclerotic vascular disease (covered later today) – Heart • Left ventricular hypertrophy (the heart muscle has to increase in size to pump blood against the aortic resistance) • Coronary artery disease (angina, myocardial infarction) • Heart failure – Brain • Stroke or transient ischemic attack – Chronic kidney disease – Peripheral vascular disease – Hypertensive retinopathy • Usually does not have any symptoms 205 Consequences of HTN Heart 206 Consequences of HTN Heart • Heart: LV Hypertrophy – workload of LV ( afterload); LV tries to compensate for workload. – LV hypertrophy is major risk factor for ischemic heart disease (myocardial infarction), dysrhythmias, heart failure, sudden death 207 Consequences of HTN Vascular Damage 208 Consequences of HTN Vascular Damage • Coronary arteries – myocardial infarction (CVII) • Peripheral blood vessels – peripheral vascular disease • Kidney – renal failure • Cerebral blood vessels – stroke 209 Diagnosis of Hypertension 210 Diagnosis of Hypertension • Repeated BP measurements – Average of > 2 readings taken at > 2 visits after an initial screening visit; over several months • Laboratory tests, x-rays looking for target organ damage – There is no specific test for hypertension, but you can look at the target organs – ECG, Urinalysis, Hb (erythropoietin in kidneysanemic due to kidney disease), Hct, Na+, K+, Cr (major indicator of kidney function), glucose, triglycerides (tells about other factors that may influence disease), cholesterol 211 Treatment of Hypertension 212 Treatment of Hypertension • Lifestyle modification is the first line of treatment – Weight reduction, regular physical exercise, DASH eating plan (a lot of fruits and vegetables, very little meat), reduction of dietary sodium intake, moderation of alcohol intake • Pharmacologic treatment • Goal: To achieve and maintain systolic BP below 140 mm Hg and diastolic BP below 90 mm Hg – The better people control their blood pressure, the less likely they are to suffer the negative effects of the hypertension on target organs 213 Sites of Action of Hypertension Diagram 214 215 Lehne, 2009, Pharmacology for Nursing Care, 67h ed., Elsevier, p. 500 Pharmacologic Treatment of Hypertension 216 Pharmacologic Treatment of Hypertension • Diuretics • Sympatholytics • Act on RAAS • Others Adapted from Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, Table 46-5, p. 502 217 Sympatholytics 218 Sympatholytics • Interfere with the sympathetic nervous system • Beta-adrenergic blockers • Alpha-1 adrenergic blockers • Centrally-acting alpha-2 agonists • Drugs that block norepinephrine release 219 Drugs that Act on the RAAS 220 Drugs that Act on the RAAS • Renin inhibitor • ACE inhibitors • Angiotensin II receptor blockers • Aldosterone antagonists 221 Other Drugs 222 Other Drugs • Ca+2 channel blockers • Direct-acting vasodilators 223 Pharmacologic Treatment Compliance 224 Pharmacologic Treatment Compliance • Compliance is a huge issue – Lifetime treatment – Many of the drugs have unpleasant side effects – Many are expensive 225 Algorithm for Treating Hypertension 226 Algorithm for Treating Hypertension Lifestyle modifications - Increase exercise (aerobic, decrease weight) Goal BP not met Stage 1 – thiazide diuretic /consider ACEI, ARB, beta blocker, CCB or combination Stage 2 – 2-drug combo (usually a thiazide + ACEI, ARB, beta blocker or CCB) Goal BP not met Optimize dosage or add a drug from a different class Goal BP not met Continue adding drugs from other classes until goal is achieved Adapted from Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 507 227 Classes of Antihypertensive Drugs Recommended for Initial Therapy in Patients with High-Risk Comorbid Conditions 228 Classes of Antihypertensive Drugs Recommended for Initial Therapy in Patients with High-Risk Comorbid Conditions Condition Heart Failure Drug Classes Recommended for Initial Therapy of HTN Diuretic Beta Blocker ACEI ARB X X X X X X Post MI X X X Diabetes X X X X X X Recurrent Stroke Prevention X Aldosterone Antagonist X X Coronary Artery Disease Risk Chronic Kidney Disease CCB X X X Adapted from Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 508 229 Drugs That Affect BP: Diuretics Diagram 230 Drugs That Affect BP: Diuretics Diagram 231 Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 500 Classification of Diuretics 232 Classification of Diuretics • Thiazide diuretics – Hydrochlorothiazide (HCTZ®) and chlorthalidone – Most common • High-ceiling (loop)– Furosemide (Lasix®) • K+ sparing: – Non-aldosterone antagonists - Triamterene (Dyrenium®) – Aldosterone receptor antagonists – Spironolactone (Aldactone) • Osmotic diuretics – Mannitol • All diuretics indirectly prevent the reabsorption of water in the kidneys!, most of them by preventing the reabsorption of sodium 233 Thiazides 234 Thiazides Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 445 Prevent re-absorption of sodium in the distal tubule. 235 Thiazides Hydrochlorthiazide and Chlorthalidone Uses 236 Thiazides Hydrochlorthiazide and Chlorthalidone Uses Uses: • Essential hypertension – Often first drug used – May be part of multiple-drug therapy • Edema – Preferred drugs for mobilizing edema associated with incompetent, premenstrual fluid retention, or mild, moderate heart failure 237 Thiazide Diuretics Adverse Effects 238 Thiazide Diuretics Adverse Effects • Hypokalemia • Hyponatremia, hypochloremia, dehydration • Orthostatic hypotension due to the dehydration • Avoid in pregnancy if possible – May reduce placental perfusion (not for routine use in pregnancy) • Nocturia if taken at night 239 Thiazide Diuretics Drug Interactions 240 Thiazide Diuretics Drug Interactions • Digoxin→digoxin toxicity (ALL K+-LOSING DIURETICS) • Lithium→lithium toxicity (ALL DIURETICS!!!) – Increase the blood levels of lithium because they rid the body of water – Diuretics are contraindicated for people on lithium • NSAIDS→ Reduced natriuresis/diuresis • Will reduce the diuretics’ ability to cause diuresis 241 Loop Diuretics 242 Loop Diuretics Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 445 Prevent the re-absorption of sodium from the ascending Loop of Henle. 243 Furosemide (Lasix®) 244 Furosemide (Lasix®) • A second-line diuretic for hypertension but has many other uses. • Used primarily for pulmonary edema associated with congestive heart failure • Edema of hepatic, cardiac, or renal origin unresponsive to less efficacious diuretics – Promotes diuresis in renal impairment 245 Loop Diuretics Adverse Effects 246 Loop Diuretics Adverse Effects • • • • • • Hypokalemia Hyponatremia, hypochloremia, dehydration Orthostatic hypotension Ototoxicity, especially in large doses Avoid in pregnancy if possible Nocturia if taken at night 247 Loop Diuretics Drug Interactions 248 Loop Diuretics Drug Interactions • Digoxin – hypokalemia is dangerous with digoxin with potassium levels are very important with the way that digoxin works • Nitrates/other antihypertensives – increased hypotensive effects • Other ototoxic drugs (aminoglycoside antibiotics) • Lithium – lithium toxicity – ALL diuretics are contraindicated for people on lithium • NSAIDS can attenuate the diuretic effect of furosemide 249 Potassium-Sparing Diuretics 250 Potassium-Sparing Diuretics Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 445 Prevent the re-absorption of sodium from the collecting tubule and duct. 251 Spironolactone - Aldactone 252 Spironolactone - Aldactone® • Hypertension • Edema • Commonly used in combination with thiazide or loop diuretics • Effects are delayed – Takes about one day or so to work 253 Spironolactone (Aldactone®) Adverse Effects 254 Spironolactone (Aldactone®) Adverse Effects • Hyperkalemia – Avoid the use of potassium supplements • Avoid salt supplements because they are made of potassium chloride – Synergistic with ACE inhibitors and ARBs • Spironolactone blocks the effects of aldosterone • ACE inhibitors and ARBs block the secretion of aldosterone – Can be extremely dangerous • Can stop your heart!! • Endocrine effects – Spironolactone has a steroid structure and can cause a variety of effects similar to steroid hormones, such as gynecomastia and impotence in men, menstrual irregularities, hirsutism, and deepening of the voice in women 255 Spironolactone (Aldactone®) Drug Interactions 256 Spironolactone (Aldactone®) Drug Interactions • Potassium supplements and salt substitutes are contraindicated • ACE inhibitors or ARBs may exacerbate the tendency to hyperkalemia • Pregnancy category D because of steroidlike effects on the fetus 257 Triamterene 258 Triamterene • Often given in combination with a thiazide – Dyazide = hydrochlorothiazide + triamterene • Hydrochlorothiazide causes hypokalemia and triamterene causes hyperkalemia, so the two drugs kind of balance each other out 259 Triamterene Adverse Effects 260 Triamterene Adverse Effects • Hyperkalemia – AVOID K+ supplements 261 Triamterene Drug Interactions 262 Triamterene Drug Interactions • ACE Inhibitors/ARBs: Hyperkalemia potential • NSAIDS may blunt diuretic effect and indomethacin may precipitate renal failure • Take after meals in AM • Avoid potassium rich diet items -- bananas, orange juice, salt substitutes (which are likely to be KCl) 263 Osmotic Diuretics - Mannitol 264 Osmotic Diuretics - Mannitol Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 445 Prevents re-absorption of water from the proximal tubule. 265 Mannitol 266 Mannitol • Must be given parenterally • Therapeutic uses – Prophylaxis of renal failure – Reduction of intracranial pressure • Draws water out of the brain – Increased intra-ocular pressure • When mannitol is in the bloodstream, before it gets into the renal tubules, it increases the osmotic pressure of the blood and draws edema fluid into the vascular system. • Mannitol is filtered into the glomerulus, drawing the excess water with it and holding it in the renal tubules for excretion. 267 Osmotic Diuretics Adverse Effects 268 Osmotic Diuretics Adverse Effects • Edema (caused by mannitol leaving the circulation and drawing water into the tissues with it) – Administer with extreme caution in heart failure because of its ability to increase vascular volume and overload the heart. • Dehydration • Orthostatic hypotension 269 Osmotic Diuretics Drug Interactions 270 Osmotic Diuretics Drug Interactions • Mannitol is not metabolized, very inert. • It has no significant drug interactions 271 Drugs Acting on RAAS Diagram 272 Drugs Acting on RAAS Diagram Renin inhibitor 273 Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 500 Renin Inhibition Diagram 274 Renin Inhibition Diagram 275 Renin Inhibitor Description 276 Renin Inhibitor Description • Renin inhibition should prevent all activation of the renin-angiotensin aldosterone system. • Only one such drug, aliskiren (Tekturna), is approved for use as monotherapy or in combination with hydrochlorothiazide. • Like other drugs that target the RAAS, aliskiren is pregnancy category D because of evidence of fetal harm. • Not used a lot yet 277 ACE Inhibitors (ACEI) 278 ACE Inhibitors (ACEI) •Introduced in the late 1980s •Angiotensin converting enzyme inhibitors •Work in the lung Captopril, lisinopril, enalapril, and others - All end in -pril Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 365. 279 Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 469 280 Therapeutic Uses of ACEI 281 Therapeutic Uses of ACEI • Hypertension • Heart failure • Protective effects in diabetic nephropathy – Protect the kidneys • Post MI prophylaxis – Prevent a second heart attack in people who have had one heart attack • Prevention of MI, stroke, and death in patients at risk 282 Therapeutic Uses of ACEIs Hypertension 283 Therapeutic Uses of ACEIs Hypertension • Initial responses: reduced formation of angiotensin II • Prolonged therapy: additional reduction in BP due to reduced formation of angiotensin II • REDUCE THE RISK OF CV MORTALITY CAUSED BY HEART FAILURE – People who are having heart failure, should be on an ACE inhibitor or an ARB • REDUCE THE RISK OF RENAL FAILURE IN DIABETICS 284 Things Not Caused by ACE Inhibitors 285 Things Not Caused by ACE Inhibitors • Do not interfere with cardiovascular reflexes – Do not cause orthostatic hypotension because they do not interfere with the baroreceptors • Do not cause hypokalemia but may contribute to the tendency to hyperkalemia if given with potassiumsparing diuretics. • Do not induce lethargy, weakness, sexual dysfunction as other antihypertensives may. 286 ACE Inhibitors Adverse Effects 287 ACE Inhibitors Adverse Effects • Bilateral renal artery stenosis is a contraindication because these drugs can precipitate acute renal failure in these patients – These people need their high blood pressure in order to get the blood past the stenotic valve and into the kidney • Dry cough – an effect of increased bradykinin • First dose hypotension – Most prominent in patients with very high BP or those on diuretics. – Should start with a lower dose • Teratogenic – contraindicated in pregnancy • Angioedema – due to increased bradykinin, may be very serious – Can be very serious if it is present in the mouth of throat 288 Angioedema Diagram 289 A 75-year-old man presented to the emergency department with diffuse swelling of his tongue that had begun a few hours earlier. He had been taking 25 mg of captopril twice daily for the past 3 years because of hypertension. He was treated with epinephrine, corticosteroids, and antihistamines and the swelling resolved over a three-hour period. The angioedema was likely due to the angiotensin-converting enzyme inhibitor. 290 Westra S and de Jager C. N Engl J Med 2006;355:295 ACE Inhibitors Drug Interactions 291 ACE Inhibitors Drug Interactions • Digoxin Increased digoxin levels • Lithium Increased lithium levels/toxicity • K+ sparing diuretics hyperkalemia • Potassium supplements hyperkalemia 292 ACE Inhibitors Additional Information 293 ACE Inhibitors Additional Information • Can be combined with a thiazide diuretic • All are oral except for enalaprilat, which is IV only • Patients with renal impairment may need dosage reduction 294 Angiotensin II Receptor Blockers (ARBs) 295 Angiotensin II Receptor Blockers (ARBs) Losartan, valsartan, candesartan, and others - End in sartan Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 365. 296 ARB Therapeutic Uses 297 ARB Therapeutic Uses • Widely used – Not as widely used as the ACE inhibitors • Hypertension – Reductions in BP = ACEI • Heart failure – prevent the progression and improve outcomes • Diabetic nephropathy – prevents progression • Post-MI prophylaxis • Stroke prevention 298 ARBs Adverse Effects 299 ARBs Adverse Effects • Well tolerated • Do not cause cough • Angioedema – Much more rare than ACE inhibitors • Fetal harm – contraindicated in pregnancy • Renal failure 300 ARBs Drug Interactions 301 ARBs Drug Interactions • Hypotensive effects are additive with other anti-HTN drugs • Do not cause hyperkalemia but may contribute if given with potassium-sparing diuretics 302 Aldosterone Antagonists 303 Aldosterone Antagonists •Spironolactone •Eplerenone (Inspra) •Potassium-sparing diuretics (covered previously as diuretics) •Block the aldosterone receptor •Promote Na+ and H20 excretion in the collecting tubule and duct 304 Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 365. Sympatholytics (Antiadrenergics) Outline 305 Sympatholytics (Antiadrenergics) Outline • • • • • Beta blockers Alpha-1 blockers Alpha/beta blockers Centrally acting alpha-2 agonists Adrenergic neuron blockers (inhibit synthesis or release of norepinephrine) • Ganglionic blockers (not used, we will not cover) 306 Sympatholytics (Antiadrenergics) Diagram 307 Sympatholytics (Antiadrenergics) Diagram Sites of Action 308 Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 500 Beta-Adrenergic Blockers 309 Beta-Adrenergic Blockers • Widely used anti-hypertensive drugs • Actions in hypertension – Blockade of cardiac beta-1 receptors→↓HR and contractility → ↓CO – Suppress reflex tachycardia caused by vasodilators – Blockade of beta-1 receptors in JG cells in kidney → ↓ renin release → ↓ RAAS mediated vasoconstriction (angiotensin II) and volume expansion (aldosterone) – Long-term use peripheral vascular resistance *Recall from Dr McLeskey’s lecture; Lehne Chapter 18 310 Beta-Adrenergic Blockers Affinity for Receptors 311 Beta-Adrenergic Blockers Affinity for Receptors • Some block both beta-1 and beta-2 receptors (nonselective) • Some have greater affinity for beta-1 than beta-2 (“cardioselective”) – but the selectivity is not absolute • Some are partial agonists – they are said to have “intrinsic sympathomimetic activity” or ISA 312 Clinical Pharmacology of Some Beta Blockers 313 Generic/trade name ISA Cardioselective (beta1 > beta2) Acebutolol/Sectal® + Atenolol/Tenormin® 0 Esmolol/Brevibloc® 0 Metolprolol/Lopressor® Slow release/Toprol XL 0 Clinical Pharmacology of Some Beta Blockers Nonselective (beta1 = beta2) Pindolol/Visken® Propranolol/Inderal® Slow release/Inderal LA® +++ 0 Nonselective alpha/beta blockers Carvedilol/Coreg® 0 Labetolol/Normodyne® or Trandate® 0 Adapted from Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 167 314 Therapeutic Uses of BetaAdrenergic Blockers 315 Therapeutic Uses of Beta-Adrenergic Blockers Drug HTN Angina Dysrrhythmias Acebutolol A I A Atenolol A A I I A A I MI Migraine Stage Fright A I I A I Heart Failure Cardioselective Esmolol Metolprolol A A Nonselective Pindolol A I Propranolol A A Carvedilol A I Labetolol A A I A A I Nonselective alpha/beta blockers A – approved; I - investigational A A 316 Adapted from Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p.168 Sympatholytics Alpha-1 Antagonists 317 Sympatholytics Alpha-1 Antagonists Sites of Action Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 500 318 Alpha-1 Antagonists 319 Alpha-1 Antagonists •Doxazosin, terazosin, prazosin and others •End in -azosin •Block alpha-1 receptors on arterioles and veins prevent SNS-mediated vasoconstriction vasodilation peripheral resistance, venous return to heart •Doxazosin, terazosin and tamsulosin (Flomax) used for BPH. •May actually be used more frequently for this than for hypertension 320 Alpha-1 Antagonists Adverse Effects 321 Alpha-1 Antagonists Adverse Effects • Not used as first line therapy for hypertension – Orthostatic hypotension is a big problem – Sexual side effects are big reasons for noncompliance 322 Centrally Acting Alpha-2 Agonists 323 Centrally Acting Alpha-2 Agonists Sites of Action Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 500 324 Centrally Acting Alpha-2 Agonists • Clonidine • Methyldopa (agent of choice for chronic hypertension in pregnancy – not for pre-eclampsia) – The only drug that is approved for hypertension in pregnancy • Act within brainstem (alpha-2 receptors) to suppress sympathetic outflow to the heart and blood vessels → vasodilation, CO BP 325 Centrally Acting Alpha-2 Agonists Adverse Effects 326 Centrally Acting Alpha-2 Agonists Adverse Effects • • • • Dry mouth Sedation Hemolytic anemia Liver disorders • Rebound hypertension if abruptly stopped – Could result in a stroke 327 Calcium Channel Blockers 328 Calcium Channel Blockers • Dihydropyridines • Non-dihydropyridines 329 Calcium Channel Blockers Dihydropyridines 330 Calcium Channel Blockers Dihydropyridines • Nifedipine • Amlodipine (Norvasc) • Used for hypertension – Promote dilation of arterioles, little effect on veins 331 Calcium Channel Blockers Non-dihydropyridines 332 Calcium Channel Blockers Non-dihydropyridines • Verapamil, diltiazem • Can be used for hypertension – Promote dilation of arterioles, little effect on veins • Also act on heart to slow conduction and decrease contractility – May be good or bad 333 Calcium Channels in the Heart Diagram 334 Calcium Channels in the Heart Diagram Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 481 335 Calcium Channels in the Heart Description 336 Calcium Channels in the Heart Description • NE – beta receptor – increased activity at calcium channels – heart – increased HR (SA node), conduction velocity (AV node), and contraction (myocardium) 337 Verapamil 338 Verapamil • Blocks Ca+2 channels in arterioles, heart – Dilation of peripheral vessels BP – Dilation of coronary arteries coronary perfusion – Blockade at SA node HR – Blockade at AV node nodal conduction – Blockade in myocardium contractile force • Indications – Angina pectoris, hypertension, dysrhythmias (Afibrillation, PSVT) 339 Verapamil Adverse Effects 340 Verapamil Adverse Effects • Constipation (why?) – Block calcium channels in the smooth muscle of the GI tract, leading to constipation • Dizziness, facial flushing, headache, edema of ankles, feet (why?) – Because of the effect on veins • Bradycardia, conduction defects (why?) – Due to effects on the heart rate 341 Nifedipine and Amlodipine (Dihydropyridines) 342 Nifedipine and Amlodipine (Dihydropyridines) • Block Ca+2 channels in arterioles – Do not have the effects on the heart that verapamil does – Used mainly for hypertension – Dilation of peripheral vessels → BP – Dilation of coronary arteries → coronary perfusion • Do NOT block cardiac Ca+2 channels at therapeutic doses 343 Nifedipine and Amlodipine Indirect (Reflex) Effects 344 Nifedipine and Amlodipine Indirect (Reflex) Effects • Lowering BP baroreceptor reflex → stimulate the medulla -- firing of SNS to beta receptors in the heart --- increased heart rate and increases contractility – Stimulating the heart may not be desirable in somebody with heart disease – Can use a beta blocker along with this in order to decrease heart rate • But, nifedipine lacks direct cardiosuppressant actions, cardiac stimulation is unopposed → HR, contractility • Net effect is the sum of the direct effect (vasodilation) and the indirect effect (reflex cardiac stimulation) 345 Nifedipine and Amlodipine Uses 346 Nifedipine and Amlodipine Uses • Angina pectoris – Vasospastic angina, angina of effort • Hypertension – Essential hypertension – Nifedipine – only use sustained-release formulation for hypertension • Take whole, do not crush or chew – Amlodipine has a longer half-life than nifedipine and does not have a sustainedrelease formulation 347 Nifedipine and Amlodipine Adverse Effects 348 Nifedipine and Amlodipine Adverse Effects • Flushing, dizziness, headache, edema • Gingival hyperplasia • Constipation – This is a big deal – People have to be on a bowel regimen of stool softeners and fiber • Do not exacerbate conduction abnormalities because they do not affect the conduction system of the heart • Do cause reflex tachycardia → cardiac oxygen demand → angina – Give with a beta blocker to counteract this in patients with angina 349 Nifedipine blocks Ca+2 channels in arterioles. This results in: 350 Nifedipine blocks Ca+2 channels in arterioles. This results in: ... of D ila tio n se D ec re a on s oc as V pe H R in tr ic ti. .. tr ic on s oc as V - Because you are blocking calcium channels, so contraction cannot occur ti. .. 25% 25% 25% 25% 1. Vasoconstriction of peripheral vessels 2. Vasoconstriction of coronary arteries 3. Decrease in HR 4. Dilation of peripheral vessels 351 Hypertensive Emergencies 352 Hypertensive Emergencies • (SBP >200 mm Hg or DBP >120 mm Hg) • Symptoms of actual or impending end-organ damage – Neurological – Cardiovascular – Other 353 Hypertensive Emergencies Neurological Symptoms 354 Hypertensive Emergencies Neurological Symptoms • Hypertensive encephalopathy - the brain does not work well, person is not oriented • Cerebral vascular accident/cerebral infarction – May have an aortic dissection where the lining of the aorta separates from the other layers, preventing the blood from going forward • Subarachnoid hemorrhage • Intracranial hemorrhage 355 Hypertensive Emergencies Cardiological Symptoms 356 Hypertensive Emergencies Cardiological Symptoms • Myocardial ischemia/infarction • Acute left ventricular dysfunction • Acute pulmonary edema • Aortic dissection 357 Hypertensive Emergencies Other Symptoms 358 Hypertensive Emergencies Other Symptoms • Acute renal failure/insufficiency • Retinopathy • Eclampsia • Microangiopathic hemolytic anemia 359 Sodium Nitroprusside-Nitropress 360 Sodium Nitroprusside-Nitropress® • A very powerful arterial vasodilator • No reflex tachycardia • Overshoot hypotension is possible but can be correctly quickly by stopping or slowing the infusion • Titrate to blood pressure – An infusion pump is essential. An arterial line or an automatic blood pressure cuff must be used to check BP continuously. 361 Sodium Nitroprusside-Nitropress Adverse Effects 362 Sodium Nitroprusside-Nitropress Adverse Effects • Cyanide poisoning • Thiocyanate Toxicity Lehne, 2009, Pharmacology for Nursing Care, 7th ed., Elsevier, p. 492 363 Adverse Effects Cyanide Poisoning 364 Adverse Effects Cyanide Poisoning • Likely in patients with liver disease • Avoid prolonged rapid infusion because of the risk of cyanide poisoning 365 Adverse Effects Thiocyanate Toxicity 366 Adverse Effects Thiocyanate Toxicity • Likely when drug given over days • CNS effects (disorientation, delirium) • Avoid infusions > 3 days; monitor plasma thiocyanate 367 IV Calcium Channel Blockers 368 IV Calcium Channel Blockers • Can be used for hypertensive emergencies • Fenoldepam – long half-life • Nicardipine – long half life • Clevidipine – short half-life, easy to titrate • Titrate similarly to sodium nitroprusside • All can cause reflex tachycardia and hypotension. 369 How do diuretics decrease blood pressure? 370 How do diuretics decrease blood pressure? 1. Block beta adrenergic receptors – beta blockers 2. Inhibit angiotensin converting enzyme – ACE inhibitors 3. Act on renal tubules to promote water excretion 4. Act as a vasodilator d. .. t.. . so va as ct A A ct on a ng i In hi b it a ta be k lo c B re na l ot .. ad r. .. . 25% 25% 25% 25% 371 Hyperlipidemia Leading to Atherosclerosis DISORDERS OF ARTERIAL CIRCULATION 372 Types of Biological Lipids 373 Types of Biological Lipids • Triglycerides, phospholipids, cholesterol classified as lipids • Lipids are chemical substances that are insoluble in water but soluble in alcohol. Three types of biological lipids • Triglycerides Used as sources for energy metabolism • Phospholipids Structural components of lipoproteins, clotting components, myelin sheath, cell membranes • Cholesterol Basis of steroid hormones and an important cell membrane component 374 Lipoproteins 375 Lipoproteins • Lipoprotein – a lipid transport particle • Lipids (cholesterol, triglycerides) insoluble in plasma – Must be transported encapsulated in lipid transport particles (lipoproteins) composed of phospholipids and embedded proteins – The outside is made of phospholipids (phosphate group on the outside that are polar and two fatty acid tails on the inside) – Green beans are triglycerides and orange circles are cholesterolproteins • Apoproteins are large proteins contained within the phospholipid coat of the lipoprotein Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 348. – Identify which lipid transport particle it is and help with its docking and release of lipids 376 Types of Lipoproteins Description 377 Types of Lipoproteins Description • Of the five types of lipoproteins, LDLs and HDLs are the most important • As the density of the lipoprotein increases, the proportion of triglycerides decreases and the proportion of cholesterol increases (except LDLs have more cholesterol than HDLs) • Chylomicrons • Come from the GI tract • Dietary lipids • VLDL • Smaller, heavier, more compact, circulate in the blood • LDL • Smaller, more compact, heavier, circulate • HDL • Smaller, most compact and dense 378 Types of Lipoproteins 379 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 348. Lipoprotein Synthesis and Transport Description 380 Lipoprotein Synthesis and Transport Description • Synthesized in small intestine, liver • Liver is important in LDL metabolism – Removes LDL via LDL receptors – Place where the HDLs bring the lipids back • Lipids are transported all over the body • Chylomicrons in the liver are changed into VLDLs and then into LDLs • Circulating to body tissues • HDLs are bringing the lipids back to the liver 381 Lipoprotein Synthesis and Transport 382 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 349. HDL 383 HDL • “Good cholesterol” • Carries cholesterol FROM tissues back TO the liver – This is why there are good • Prevent atherosclerosis • High HDL prevents atherosclerosis – HDLs are scavengers, picking up cholesterol from deposits in the arteries and bringing it back to the liver for disposal • HDL inhibits uptake of LDLs into cells • Heredity, exercise, moderate ETOH (1-2 drinks per day for women) HDLs • Smoking, diabetes or metabolic syndrome (sort of a diabetic prodrome) HDLs 384 LDL 385 LDL • “bad cholesterol” • Familial defects in LDL receptor – “familial hypercholesterolemia” – Inadequate, or defective hepatic uptake of LDL circulating LDL – Have heart attacks and strokes at very early ages • “Receptor disease” 386 LDL Receptors in Liver Remove LDLs from the Blood 387 LDL Receptors in Liver Remove LDLs from the Blood Robbins & Cotran Pathologic Basis of Disease (7th ed), 2005, Elsevier, p.158 388 Hypercholesterolemia 389 Hypercholesterolemia Xanthomas (deposits of cholesterol) develop in certain areas, including the knuckles. - Not very common Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 350. 390 Hypercholesterolemia Primary 391 Hypercholesterolemia Primary • • • • • Develops independent of other causes Defective synthesis of apoproteins Lack of receptors Defective receptors Defects in handling of cholesterol in cell that are genetically determined • Familial hypercholesteremia 392 Hypercholesterolemia Secondary 393 Hypercholesterolemia Secondary • Associated with other health problems and behaviors (high fat diet, obesity, diabetes mellitus) 394 Diagnosis Screening 395 Diagnosis Screening • All adults 20 years of age and older should have a fasting lipoprotein profile done every 5 years – Total cholesterol, LDL, HDL, TG See Porth, text on page 350-351 for specific recommendations Also Table 49.4 in Lehne 396 Classification of LDL, Total, and HDL Cholesterol 397 Classification of LDL, Total, and HDL Cholesterol Cholesterol Level (mg/dL) Total <200 200-239 >240 Classification Optimal Borderline high High Cholesterol Classification Level (mg/dL) HDL cholesterol <40 Low >60 High LDL cholesterol <100 100-129 130-159 Optimal Above optimal Borderline high 160-189 >190 High Very high Adapted from Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 350. 398 Why are Increased Blood Lipids so Bad? 399 Why are Increased Blood Lipids so Bad? • Increased blood lipids, particularly cholesterol, increase the risk of a vascular disease called atherosclerosis. – Fatty deposits form in arterial walls • This increases the risk of clot formation and occlusion of an artery. – Occluded arteries cause myocardial infarctions, stroke, and peripheral vascular disease, which may lead to necrosis of part of the extremity. • Atherosclerosis leads to arteriosclerosis (hardening of the arteries) caused by calcium deposits in the walls of the arteries – Increases the risk of aneurysms and other vessel wall problems. 400 Atherosclerosis 401 Atherosclerosis • Atheros (glue/paste) • Sclerosis (hardening) • Formation of fibrofatty lesions (atheromas) in the intimal lining of large and medium sized arteries (aorta, coronaries, carotids, and many others) – Not present in the veins 402 Atherosclerotic Lesions 403 Atherosclerotic Lesions • Fatty streak – Thin, flat, yellow discolorations that progressively enlarge by becoming thicker and more elevated. Present in children. Precursors to atheromata • Atheroma • Fibrous plaque – Increases in smooth muscle and collagen • Complicated lesions – A complicated lesion has a lot of smooth muscle vessels that have proliferated – Macrophages eat up the lipids – This type of lesion can serve as the focus of a clot and represents a weakness in the artery that may cause problems – Characterized by thrombosis, fissure, and hematoma formation 404 Atheromatous Plaque 405 Atheromatous Plaque Plaque Complicated Lesion Porth, 2007, Essential of Pathophysiology, 2nd ed., Lippincott, p. 353 406 Definitions Thrombus, Embolus, Stenosis, Mural 407 Definitions Thrombus, Embolus, Stenosis, Mural • Thrombus = clot • Embolus = a clot that breaks off from its initial location and travels through the vascular system. • Stenosis = narrowing or closing off of a vessel (or a heart valve). • Mural = wall (a mural thrombus is a clot in the wall of a vessel or a chamber of the heart) 408 Atherosclerosis Timeline 409 410 410 Progression of Atherosclerosis 411 Robbins & Cotran Pathologic Basis of Disease (7th ed), Elsevier, 2005, p.517 412 Atheromatous Lesion Diagram 413 414 Atheromas 415 •Atheromas tend to develop at sites of turbulent flow – near branch points and arteries •As the artheroma develops, it creates more of a constriction, which produces more turbulent flow and more atheromas. •See Figure 17.8 in Porth! Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 352. 416 Laminar and Turbulent Flow 417 Laminar and Turbulent Flow Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 323. 418 Lifestyle Risk Factors for Atherosclerosis 419 Lifestyle Risk Factors for Atherosclerosis • Many people have more than one of these risk factors • Age – Men > 45 y.o.; women > 55 y.o. (or premature menopause) • Removing ovaries at an earlier age, will accelerate women’s risk of atherosclerosis • Family History – MI before 55 y.o. in father or before 65 y.o. mother • Current cigarette smoking – If you stop smoking, the risk decreases quickly • Hypertension (BP > 140/90) • Hyperlipidemia – Low HDL (< 40 mg/dL) – High LDL • Diabetes mellitus 420 Risk Factors Markers 421 Risk Factors Markers • C-reactive protein (CRP) – Marker of inflammation; may be a better than LDL? – Not very specific because you can have inflammation for many different reasons • Homocysteine – Inhibits coagulation, causes endothelial damage, important in initial phases? – It is good to be elevated and bad to be low – Not a great predictor of athlerosclerosis • Serum lipoprotein (a) – Part of the LDL; promotes foam cells – If it is elevated, it is a risk factor • Infectious agents – Chlamydia pneumoniae 422 Clinical Manifestations of Vascular Disease 423 Clinical Manifestations of Vascular Disease Cotran (1999) pg. 499 424 Management of Hyperlipidemia 425 Management of Hyperlipidemia • Reduction in LDL is primary target for cholesterol-lowering therapy, particularly for people at risk for CHD* – It is not as easy to raise the HDL as it is to lower the LDL – Age, family history of premature CHD, cigarette smoker, hypertension, low HDL, diabetes mellitus • Some evidence that when lipids are lowered, at least with statin drugs, that atheromatous changes regress. – This is a very good thing • Dietary changes* • Lifestyle changes • Pharmacologic treatment – calories, saturated fats, cholesterol – physical activity, smoking cessation, weight loss *See Porth, Table 17-1, page 351 and Lehne, Table 49-4, p. 551 * See Lehne, Table 49-6, pg. 556 426 Lipid-Lowering Drugs Diagram 427 Lipid-Lowering Drugs Diagrams 428 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 349. Mechanisms of Lipid-Lowering Drugs 429 Mechanisms of Lipid-Lowering Drugs • 1. 2. 3. 4. 5. Mechanisms: Affect cholesterol production by the liver Remove cholesterol from bloodstream LDL receptors Cholesterol absorption from intestine intravascular conversion of VLDL and IDL to LDL 430 Classes of Drugs Used in Treatment of Hypercholesterolemia 431 Classes of Drugs Used in Treatment of Hypercholesterolemia • • • • • HMG-CoA reductase inhibitors (statins) Bile acid-binding resins Cholesterol absorption inhibitor agents Niacin and its congeners Fibric acid derivatives 432 Types of Statins 433 Types of Statins • • • • • • • All end in -statin Atorvastatin [Lipitor] Fluvastatin [Lescol] Lovastatin [Mevacor] - generic Provastatin [Pravachol] Rosuvastatin [Crestor] Simvastatin [Zocor] - generic 434 Statins Beneficial Actions 435 Statins Beneficial Actions • Reduce cholesterol synthesis in liver • LDL receptors (most important) – LDLs from the circulation, which is desirable • HDLs • TG 436 Statins Timing 437 Statins Timing • Results within 2 weeks; maximal 4-6 weeks • If drug is stopped, serum cholesterol returns to pretreatment levels (lifelong treatment), unless the person has lost substantial weight 438 Statins LDL Receptors in Liver -> LDLs 439 Statins LDL Receptors in Liver -> LDLs Robbins & Cotran Pathologic Basis of Disease (7th ed), 2005, Elsevier, p.158 440 Statins Actions 441 Statins Actions • Cardiovascular actions – Reduce inflammation at plaque sites – Improve endothelial cell function – Enhance blood vessel dilation – Reduce the risk of thrombosis • Increased bone formation – Enhance osteoblast activity risk of osteoporosis and fractures 442 Statins Therapeutic Uses 443 Statins Therapeutic Uses • Hypercholesterolemia • Prevention of cardiovascular events – MI, stroke, angina • Diabetes – ADA: Pts > 40 y.o. with total cholesterol > 135 mg/dLregardless of LDL – ACP: All pts with type 2 diabetes with coronary artery disease, even if they don’t have high cholesterol; all adults with type 2 diabetes plus one CV risk factor - even if they don’t have high cholesterol 444 Statins Side Effects 445 Statins Side Effects • Myopathy (inflammation of the muscle)/rhabdomyolysis (total muscle breakdown) – Report unexplained muscle weakness, tenderness – Rhabdomyolysis can be fatal – Rosuvastatin higher risk • Hepatotoxicity – Monitor liver enzymes every 6-12 months – Avoid use for patients with viral or alcoholic hepatitis 446 Statins Drug Interactions 447 Statins Drug Interactions • Fibrates and ezetimibe – Also cholesterol, so their activity might be additive to statins – Can also cause myopathy, so the danger from that would also be increased • Inhibitors of cytochrome P450 like ketoconazole, erythromycin, HIV protease inhibitors, etc., inhibit the metabolism of statins and raise blood levels risk of adverse effect 448 Bile Acid Sequestrants 449 Bile Acid Sequestrants • Cholestyramine, colestipol, and colesevelam • Biologically inert, insoluble in water, cannot be absorbed from GI tract, simply pass through intestine, excreted in feces 450 Bile Acid Sequestrants Actions 451 Bile Acid Sequestrants Actions • Absorb bile acids in the intestine and keep them from being reabsorbed into the bloodstream. – New bile acids must be synthesized, which requires cholesterol. – LDLs are internalized into liver cells as a source of cholesterol. – This lowers LDLs. • Reduce LDL cholesterol – Maximal reduction within one month (20%) – LDL levels return to pre-treatment levels when drug is discontinued 452 Bile Acid Sequestrants Diagram 453 Bile Acid Sequestrants Diagram Prevent the absorption of cholesterol in the intestine 454 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 349. Bile acid reabsorption (GI) synthesis in liver need for cholesterol LDL receptors 455 Bile acid reabsorption (GI) synthesis in liver need for cholesterol LDL receptors 456 Robbins & Cotran Pathologic Basis of Disease (7th ed), 2005, Elsevier, p.158 Bile Acid Sequestrants Therapeutic Use 457 Bile Acid Sequestrants Therapeutic Use • Reduce LDL cholesterol – Drug plus diet -> LDL by 15-30% • Usually combined with statin – LDL by 50% 458 Bile Acid Sequestrants Adverse Effects 459 Bile Acid Sequestrants Adverse Effects • Devoid of systemic effects because they are not absorbed • GI symptoms (except colesevelam) because it swells up in the GI tract (drink it) – Constipation – Bloating – Indigestion – Nausea 460 Bile Acid Sequestrants Drug Interactions 461 Bile Acid Sequestrants Drug Interactions • Cannot take a lot of medications because it will absorb medications and keep them from being absorbed • Decreased absorption of: – – – – – Warfarin -Acetaminophen Thiazides -Beta blockers Digoxin -Corticosteroids Iron -Thyroid hormones Fat-soluble vitamins A, D, E, and K (except colesevelam) – Take oral medications 1 hour before or 4 hours after the bile acid sequestrant. 462 Cholesterol Absorption Inhibitors Ezetimibe (Zetia®) 463 Ezetimibe (Zetia®) Mechanism of Action 464 Ezetimibe (Zetia®) Mechanism of Action • Mechanism of action • Acts on cells in the brush border of the intestine and inhibits cholesterol absorption – Does not actually absorb the cholesterol like the previous drug • Blocks absorption of dietary cholesterol and cholesterol secreted in bile • Lowers total cholesterol, LDLs, TG and raises HDLs 465 Ezetimibe (Zetia®) Use 466 Ezetimibe (Zetia®) Use • Used as adjunct to diet modification • Can be used as monotherapy or with a statin – Recent evidence that the combo of ezetimibe and simvastin (Vytorin) actually worsened plaques rather than making them better. 467 Ezetimibe (Zetia) Drug Interactions 468 Ezetimibe (Zetia) Drug Interactions • Statins - risk of liver damage • Fibrates – both the concentration of cholesterol in the bile the risk of gallstones, which is precipitated solid cholesterol • Bile-acid sequestrants- impair the absorption of ezetimibe • Cyclosporine- inhibits metabolism of ezetimibe its concentration. 469 Nicotinic Acid (Niacin) [Niacor, Niaspan] 470 Nicotinic Acid (Niacin) [Niacor, Niaspan] Decreases production of VLDLs by inhibiting lipolysis in adipose tissue LDL 471 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 349. Nicotinic Acid (Niacin) 472 Nicotinic Acid (Niacin) • Effect on plasma lipoproteins: – Reduces triglycerides (20 – 50%) and LDLs (5-25%) – Raises HDLs (15-35%) – Drug of choice to lower triglyceride levels in patients at risk for pancreatitis. – More effective when combined with statin – Triple therapy (nicotinic acid, statin, bile-acid sequestrant) LDL 70% • Nicotinic acid is also a B-vitamin, but doses as a vitamin are much smaller than as a lipid-lowering drug. 473 Nicotinic Acid Adverse Effects 474 Nicotinic Acid Adverse Effects • Intense flushing of the head and neck in nearly all patients– diminishes in several weeks, attenuated with aspirin • GI upset – take with food • Hepatotoxic – follow liver enzymes • Raises blood levels of homocysteine, a substance thought to increase cardiovascular risk. To counteract this, add folic acid supplements. • Hyperglycemia – use with caution in diabetics 475 Fibric Acid Derivatives (Fibrates) 476 Fibric Acid Derivatives (Fibrates) - Gemfibrozil [Lopid] - Fenofibrate [Tricor] 1. Increase lipoprotein lipase → VLDLs and TG storage in adipose tissue ( serum TG) 2. Also HDL 3. No effect on LDL 477 Porth, 2007, Essentials of Pathophysiology, 2nd ed., Lippincott, p. 349. Fibric Acid Derivatives Adverse Effects 478 Fibric Acid Derivatives Adverse Effects • Gallstones – Increase biliary cholesterol saturation → increase risk of gallstones • Myopathy – like the statins, can cause myopathy • Hepatotoxicity – like the statins, fibric acid derivatives are hepatotoxic; Monitor liver enzymes • Because of overlapping adverse effects, the combo of a statin and a fibric acid derivative should be used with great caution. • Pregnancy category C 479 Fibric Acid Derivatives Drug Interactions 480 Fibric Acid Derivatives Drug Interactions • Warfarin – Gemfibrozil increases the efficacy of warfarin by displacing it from protein binding sites. – Follow INR closely • Use with caution in statins because of the increase in risk of myopathy 481 Which of the following drugs are insoluble in water, cannot be absorbed from the GI tract and pass through the intestine? 482 Which of the following drugs are insoluble in water, cannot be absorbed from the GI tract and pass through the intestine? id N ic o tin ac ic id ac .. br ic Fi C M G H B ile ac oA id re d se q uc . u. .. 1. Bile acid sequestrants 2. HMG Co-A reductase inhibitors 3. Fibric acid derivatives 4. Nicotinic acid de ... 25% 25% 25% 25% 483 Which of the following drug classes has been shown to reverse atherosclerotic changes? 484 Which of the following drug classes has been shown to reverse athrosclerotic changes? 25% 25% 25% 25% in ia c N u. .. se q id ac ile B Fi br ic ac id St at in s de ... 1. Statins 2. Fibric acid derivatives 3. Bile acid sequestrants 4. Niacin 485 Questions? 486