Presentation

D.H.
Clinical Pathology Conference
August 24, 2015
Stella Lai MD
Ronald Hamilton MD
HPI
29 yo M w/ h/o ulcerative colitis, basal cell carcinoma and metastatic melanoma who presented to ED for diffuse HA, nausea, transient visual disturbance
(flashing lights in L upper visual field), transient L hand numbness + tingling, speech difficulty and acute onset confusion.
Other History
PMHx/PSHx
HTN
Nephrolithiasis
Ulcerative Colitis
Basal Cell Carcinoma s/p resection
Metastatic Melanoma w/ known brain, lung, chest wall, lymph node, thigh and gluteus involvement s/p numerous biopsies + resections and treatment w/ IL2, aflibercept, dendritic cell vaccine +/- interferon booster and pembrolizumab
Allergies
Ativan (parodoxical agitation)
Meds
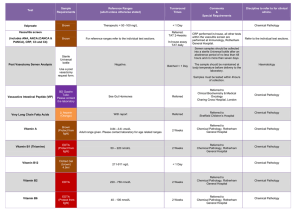
Vitamin B6, Vitamin B12, Vitamin D, Vitamin E, MV,
Dexamethasone Taper, Keppra 1000mg BID,
Mesalamine 4800mg QHS, Zofran PRN, oxycodone PRN
Social Hx
Lives w/ wife. No smoking, alcohol or illicits.
Family Hx
Mother: Prothrombin Gene Variant w/ h/o DVT/PE
Maternal GM: Breast Cancer @ 55
Exam
VS: 37.2, BP 143/90, HR 98, RR 17, O2 Sat 97% RA
MS: Alert and oriented x 3, Agitated, Repetitive/slow/ labored speech, Follows simple commands
CN: VFs intact, PERRL, EOMI, No facial asymmetry
MOTOR: 5/5 strength throughout
SENSORY: Intact to light touch throughout
REFLEXES: 2+ biceps/triceps/patella/achilles, No ankle clonus, No Hoffmans
COORDINATION: ?
GAIT: ?
Clinical Localization
….of confusion, diffuse headache, nausea, speech difficulty (sounded like it was mostly expressive), L hand numbness/tingling and L upper VF flashing lights.
Hospital Course
Received 10mg IV Decadron and 25g IV mannitol in ED, and was admitted for further management. He was continued on Decadron 4mg IV 6 hours and returned back to baseline 24 hours after admission. He was d/ced on dexamethasone slow taper w/ instructions for repeat brain
MRI in 1 month.
Hospital Course
2 months later, he presents w/ acute abdominal pain. It was initially tolerable but progressed to stabbing, 10/10 pain that was not responsive to oxycodone. CT abdomen revealed L renal vein thrombosis and diffuse metastatic disease. He was initially placed on heparin gtt which was stopped b/c of his known hemorrhagic metastatic brain lesions. He underwent repeat neuroimaging.
• MRI ETC:
Hospital Course
3 days after admission, abdominal pain acutely worsened. CT abdomen revealed free air and small bowl perforation. Not a surgical candidate b/c of hemodynamic status. The next day, he arrested (?2/2
PE) requiring 30 minutes of CPR for ROSC. He was intubated and maxed out on 3 pressors. Given poor prognosis, he was made CMO and expired.
Pathology
Gross Pathology
Well-demarcated lesions
Variable amount of pigmentation
Could be hemorrhagic and necrotic
Micro Pathology
Pleomorphic Melanocytes
Mitosis
Necrosis
Staining + for S-100, HMB-45, Melan-A