Food-induced Anaphylaxis-Dignosis and Treatment
advertisement

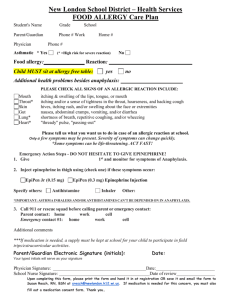
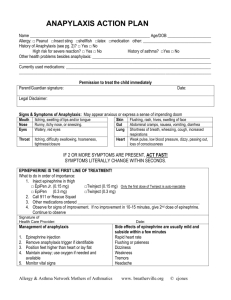
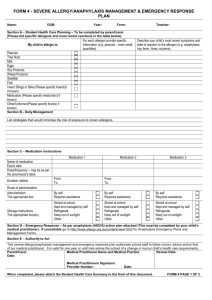
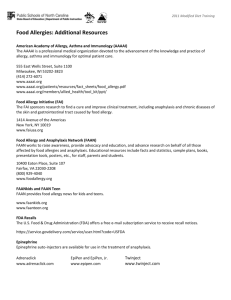
Dana V. Wallace, MD ACAAI Immediate Past President FACAAI, FAAAAI Associate Clinical Professor Nova Southeastern University Fort Lauderdale, Florida www.drdanawallace.com drdanawallace@gmail.com The Causes of Anaphylaxis: Select Cases (1002) Venom ?? 11-21% (up to 65%) Webb et al:J Allergy Clin Immunol 113:s241,2004 Anaphylaxis Incidence & Fatality Incidence (lifetime) risk 1 to 3%1 Incidence rate of anaphylaxis 1-2% Case-fatality rate is 0.65% to 1%1-2 Prevalence of food anaphylaxis unknown Highest rate in children and adolescents Best data for incidence is from outpatient Rx for epinephrine auto-injectors 1Kemp SF. JACI 2002; 110:341-348. 2. Yocum, Michael et al: J Allergy Clin Immunol ,104:452-6. 1999 Variable Incidence of Foodinduced Anaphylaxis Related Factors Age Regional diets Food preparation Amount of exposure Timing of first exposure Boyce, J. A., A. Assa'ad, et al. "Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report. " J Allergy Clin Immunol 126(6): 1105-18. [referred to as “NIAID Food Allergy Guidelines 2010” ] Foods Allergy Prevalence NIAID 2010 Guidelines Children Adults Cow’s milk (1-2 %) Egg (1-2%) Peanut (0.6%) Shellfish (0.5%) Fish (.2%) Soybean Wheat Shellfish (2.8%) Vegetables (0.01-13.7% Fruits (0.02-8.5%) Peanuts (0.6%) Tree nuts (0.4-0.5%) Fish (0.5%) Gupta 2011 Pediatric Survey Peanut Gupta, R. S. Pediatrics 128(1): e9-17. Major class 1 food allergens Cow's milk: Caseins (, ,), -lactoalbumin, -lactoglobulin, serum albumin Chicken egg: Ovomucoid, ovalbumin, ovotransferrin Peanut: Vicillin, conglutin, glycinin Soybean: Glycinin, profilin, trypsin inhibitor Shrimp: Tropomyosin ** Lipid transfer proteins (LTPs): ** Apple, apricot, peach, plum, corn POLLEN FOOD ALLERGY SYNDROME Gastrointestinal food hypersensitivities: Pollen food allergy syndrome or oral allergy syndrome (OAS) Oral mucosal itching, swelling, tingling Elicited by a variety of plant proteins that cross-react with airborne allergens Pollen allergic patients may develop symptoms following the ingestion of vegetables foods: - Ragweed allergic patients: Fresh melons and bananas - Birch pollen allergic patients: Carrots, celery, apples, pears, hazelnuts and kiwi Immunotherapy for treating the pollen-induced rhinitis may or may not reduce oral allergy symptoms J Allergy Clin Immunol. 2004; 113:808-809 Components of Pollen Food Allergy Syndrome (PFAS) A history of symptoms consistent with PFAS Allergic sensitization to pollen Allergic sensitization to a plant food A known correlation between the plant food and the pollen Pollen Food Allergy Syndrome (PFAS) Oral Allergy Syndrome + systemic reactions PFAS emphasizes that one may have not only oropharyngeal symptoms but systemic symptoms 2-10% of the time While usually associated only with raw foods, cooked plant foods may provoke the PFAS Prick-by-prick testing to fresh food is preferred for most fruits and vegetables Stable allergens, e.g. peanut, hazelnut, and pea may be best detected with commercial extracts Consider duplicate testing when extracts are available Food allergy: Exercise-induced anaphylaxis Exercise Food Temperature Gastrin Mediator release - Histamine - Others (LTD4,PAF, etc) ANAPHYLAXIS Exercise Anaphylaxis Foods associated Shellfish 16% Alcohol 11% Tomatoes 8% Cheese 8% Celery 7% Strawberries, milk, wheat & or Omega- 5 gliadin, other grains, peaches – each 5% Advise early AM exercise before eating or > 4 hrs. after eating Chong s-u, 35 al. Int Arch Allergy Immunol. 2002;120:19-26. Exercise Anaphylaxis (EA) Food-dependant Exercise leads to increased gut permeability which thereby increases food allergen intake Patients with low levels of sIgE food antibodies are tolerant until stressed by exercise In wheat-dependent AE, exercises activates tissue transglutaminase, which results in high molecular-weight omega-5 gliadin complexes that bind IgE with increased intensity leading to anaphylaxis Lemon-Mule H. Current Allergy and Asthma Reports 2008. 8(3): 201-208. New causes of Anaphylaxis Cetuximab Antibodies to oligosaccharide galactose-alpha-1,3 galactose present prior to Tx Felt possibly to x-react with same oligosaccharides in beef or pork; +/- parasites or histoplasmosis (not established) 1 Cat allergic patients may have IgE to the cat IGA galactose-α 1,3 galactose Testing for IgE to cat has been suggested 2 Desensitization protocol has been used 3 1. Chung, NEJM 2008; 358-1109 2. Gronlund H et al. JACI 1009, 123:1189. 2. 3. Jerath MR at al. JACI 2009, 123: 260 Radiocontrast Anaphylactoid Rx Not related to shellfish allergy Seafood Allergy is NOT a risk factor: Possible origin of the myth: – In 1975 Shehadi et. al noted the following regarding patients reactions: • 15% of patients gave an unconfirmed history of shellfish allergy • They surmised iodine in shellfish was responsible for the allergy. [FALSE] • They surmised iodine in shellfish cross-reacted to iodine in RCM. [FALSE] Shehadi WH. Am J Roentgenol. 1975; 124: 145-152. Beaty AD. American Journal of Medicine. 2008; 121 (2): 158e. Subsequent Reactions May Increase in Severity with Time 1st Reaction 60 2nd Reaction 3rd Reaction % of reactions 50 * * 40 30 20 10 0 Peanut allergen Tree nut allergen Proportion of reactions rated severe Simons et al, J Allergy Clin Immunol, 2004 Fatal Food-induced Anaphylaxis Highest Risk Factors Peanuts and tree nuts account for up to 92% of fatalities1,2 Adolescents (14-17) and young adults highest risk group1 Asthma as a concurrent disease (>90% some studies), esp. poorly controlled asthma2,3 Cardiovascular disease in middle-aged & older patients Delay between time of symptom onset and administration of treatment (OR up to 7.3)2,4 Improper epinephrine dosing, usually underdosing5 1. Bock, SA, et ak, JACI 2004; 107 (1) 191-3. 2. Sampson HA,et al., NEJM. 1992; 237:380384.3. Pumphrey R. Curr Opin Allergy Clin Immunol. 2004;4:285-290. 4. Amin HS, et al. JACI 2006; 117:169-75.5. NIAID Food Allergy Guidelines 2010 ANAPHYLAXIS DX & TX Clinical Criteria for Anaphylaxis Anaphylaxis is likely if 1 or 3 set of criteria are fulfilled Acute onset (min to hrs) 1– Skin/mucosal symptoms AND – Airway compromise OR – ↓ BP or Associated symptoms 3 Hypotension within min. to hrs. after exposure to known allergen 2 Exposure to known allergen + at least 2 items below within min to hrs – – – – Hx of severe reaction (2005) Skin/mucosal symptoms Airway compromise ↓ BP or Associated symptoms – GI symptoms with food allergy Symposium on the Definition and Management of Anaphylaxis: Summary report. Sampson HA, et al. JACI 2005; 115:584-59. Second symposium on the definition and management of anaphylaxis: summary report. Sampson HA, et al. JACI 2006; 117(2): p. 391-7. Symposium on the Definition & Management of Anaphylaxis: Summary Report “Caution: These criteria describe so called classic cases of anaphylaxis. Other presentations may also indicate anaphylaxis (e.g. early presentation, generalized flushing; isolated presentation, sudden hypotension only in a patient without evidence of allergen exposure; classic presentation but with a nonallergenic cause, such as exercise)” Sampson HA et al. J Allergy Clin Immunol 2005;115:584-91. “ANAPHYLAXIS” FUNCTIONAL DEFINITION An acute allergic reaction for which it is known that there is potential for fatality – Regardless of the severity of the presenting symptoms – For which immediate treatment has been shown to prevent progression of the disease process Can Anaphylaxis occur on first ingestion of a food? Usually, but not always, there is a history of food allergy, with or without anaphylaxis First-time food ingestion can occur at any age, more common in young children 20% first time anaphylaxis events (to a specific food exposure) occur in the school setting NIAID Food Allergy Guidelines 2010 Characteristics of Food-induced Anaphylaxis Increasing in incidence in industrialized countries Food-induced anaphylaxis is not easily recognized, delaying diagnosis Dx heavily dependent on – Early recognition of specific signs and symptoms – Timing of the reaction – Concomitant factors and disease processes No tests, including prick, sIgE, challenge studies, can predict the severity of IgE mediated reactions to foods NIAID Food Allergy Guidelines 2010 Most Frequent Signs and Symptoms of Anaphylaxis: Regardless of cause Manifestation Percent Urticaria/angioedema 87 Flush 50 Dyspnea/wheeze 46 Hypotension 30 Gastrointestinal 30 1. Lieberman P. Immunol Allergy Clin North Am. 2001;21:813-825. 25 Less Frequent Signs and Symptoms of Anaphylaxis Manifestation Percent Rhinitis 16 Headache 15 Substernal pain 6 Itch without rash 4.5 Seizure 1.5 1. Lieberman P. Immunol Allergy Clin North Am. 2001;21:813-825. 26 Signs and Symptoms of Foodinduced Anaphylaxis Are they different? Up to 20% have no cutaneous symptoms Up to 70% of cases have respiratory involvement (upper or lower airway) Up to 40% have GI Symptoms Up to 35% have cardiovascular symptoms Other symptoms: anxiety, mental confusion, lethargy, and seizures NIAID Food Allergy Guidelines 2010 Cardiovascular co-morbidity Increased heart mast cells present with ischemic heart dx & cardiomyopathy Mast cells accumulate at sites of coronary atherosclerotic plaques IgE antibodies bound to heart mast cells can trigger degranulation Anaphylaxis may trigger myocardial ischemia due to plaque rupture 15% of severe anaphylaxis present with chest pain 7% severe anaphylaxis present with an arrhythmia 1. Kemp SF et al. Allergy 2008. 63(8): 1061-70. 2. Lieberman P et al. The diagnosis and management of anaphylaxis practice parameter: 2010 Update. J ACI 2010. 126 (3) 477-80, (AKA 2010 JTF Anaphylaxis PP) LABORATORY TESTS IN THE DIAGNOSIS OF ANAPHYLAXIS Plasma histamine Serum tryptase A M O U N T 24-hr Urinary histamine metabolite 0 30 60 90 120 150 180 MINUTES 210 240 270 300 330 Serum Tryptase Total Serum Tryptase in anaphylaxis may remain within nl range, but if > 2 ng/ml above baseline it has 0.73 sensitivity & 0.98 specificity for dx of anaphylaxis1 Usually not ↑ in food-induced anaphylaxis ↑ more likely in hypotensive anaphylaxis * Dr. Larry Schwartz lab, Virginia Commonwealth University 1. Brown SG et al. Emerg Med Austral 2004; 16:120 Time Course of Food-induced Anaphylaxis Onset is usually minutes (e.g. 3-5) to a few hours after exposure to food allergen Biphasic reactions occur in up to 20% of cases (usually < 8 hours in food allergy) NIAID Food Allergy Guidelines 2010 Biphasic Anaphylaxis Treatment Initial Symptoms Treatment 1-8 hours 0 Antigen Exposure SecondPhase Symptoms Classic Model 1-48 hours New Evidence Time BIPHASIC ANAPHYLACTIC REACTIONS Characteristics Etiology not always clear – Immunological, e.g. late-phase response – Pharmacologic-medication effect has ended Usually involves same organ system Cannot be predicted based on severity of initial reaction Ellis AK, Day JH. Ann Allergy Asthma Immunol 2007;98:64-9. Time Course of Food-induced Anaphylaxis Onset is usually minutes (e.g. 3-5) to a few hours after exposure to food allergen Biphasic reactions occur in up to 20% of cases (usually < 8 hours in food allergy) Prolonged reactions occur in up to 20% of cases Deaths reported 30 minutes to 2 hours following exposure to food NIAID Food Allergy Guidelines 2010 Onset of Anaphylaxis to Cardiopulmonary Arrest Pumphrey R. Curr Opin Allergy Clin Immunol. 2004;4:285Y290 Clinical Factors Affecting Anaphylaxis Severity & Fatality Psychiatric disease Substance abuse Beta-blockers COPD PAF acetylhydrolase factor deficiency Subclinical mastocytosis Previous anaphylaxis 1. Bock, SA, et ak, JACI 2004; . Sampson HA,et al., NEJM. 1992; 237:380-384. 3. Pumphrey R. Curr Opin 4. NIAID Food Allergy Guidelines 2010 Simons, E. et al. J Allergy Clin Immunol 2007;120:S2-24.) Additional Risk Factors for FA Anaphylaxis Fatality Multiple food allergens (3x increase) Shellfish (#1 allergen after age 14) Ingestant of allergen (No known report of fatality when only skin contact) If there is no skin manifestations of anaphylaxis (delay in diagnosis) Many Mediators Cause Anaphylactic Symptoms Leukotrienes Prostagandins Kinins • Platelet activating factor • Interleukins • Tumor necrosis factor • Histamine Actions of Epinephrine: Antagonize Effects of All Mediators Epinephrine 1-adrenergic receptor Vasoconstriction Peripheral vascular resistance Mucosal edema 2-adrenergic receptor Insulin release 1-adrenergic receptor Inotropy Chronotropy 2-adrenergic receptor Bronchodilation Vasodilation Glycogenolysis Mediator release Simons KJ, Simons FER. Curr Opin Allergy Clin Immunol. 2010;10:354-361. Epinephrine Cardiovascular Effects Enhances coronary blood flow – Increased duration of diastole (vs. systole) – Vasodilator effects caused by increased myocardial contractility Vasoconstrictor effects on coronary arteries would seem to be undesirable but it is – Felt to be a minor effect compared to above benefit Kemp SF et al. Allergy 2008. 63(8): 1061-70. False Sense of Security Food-induced anaphylaxis can have a mild course and resolve spontaneously – Most likely related to endogenous production of vasoconstrictors • Epinephrine • Endothelin-I • Angiotensin II NIAID Food Allergy Guidelines 2010 Beta Blockers & ACE Inhibitors Exposure to β-adrenergic blocking agents is a risk factor for more serious & Tx resistant anaphylaxis1,2,3 – May reduce the effect of exogenous epinephrine – May reduce the effect of endogenous epinephrine ACE inhibitors (OR 2.7) are a risk for more severe anaphylaxis (e.g. with venom immunotherapy)1,2 ACE inhibitors “may” interfere with endogenous compensatory mechanisms, resulting in more severe or prolonged symptoms of food-induced anaphylaxis3 No evidence of increased risk for ACE receptor blockers 1. 2010 JTF Anaphylaxis PP) 2. Cox L. Allergy Immunotherapy- a practice parameter third update. JACI 127(1 supp) S1-55. 3. NIAID Food Allergy Guidelines 2010 Steps in Treatment of Anaphylaxis #1 Remove Allergen #3 Call for help #2 Administer Epinephrine Supplies and Equipment for Anaphylaxis Treatment in office “NECESSARY” Stethoscope and sphygmomanometer Epinephrine 1:1000 Oxygen IV Fluids Tourniquets, syringes, hypodermic needles, large-bore needles 2010 JTF Anaphylaxis PP “CONSIDER HAVING” One-way valve facemask Diphenhydramine inj. Corticosteroids inj. “MAYBE” Vasopressor (Dopamine) Glucagon Automatic defibrillator Oral airway KEY POINTS ON GENERAL ANAPHYLAXIS DX AND TX Anaphylaxis protocols are based on consensus –not on evidence The more rapid the onset of signs and symptoms following exposure to offending stimulus, the more likely the reaction will be severe and life-threatening. Delayed onset of anaphylaxis, with delayed Tx, also introduces high risk KEY POINT # 1 DRUG F0R ANAPHYLAXIS EPINEPHRINE Adult- 1:1000 0.2-0.5 ml q 5 minutes (or less) PRN Child-0.01 mg/kg , max 0.3 mg q 5 minutes (or less) PRN IM in Lateral thigh (speaker preference) 1” EPINEPHRINE PREVENTS Blocks further mediator release TREATS Reverses the end-organ effects of Anaphylaxis IM vs. SQ Epinephrine in Children 8+ - 2 minutes (EpiPen®) SHORTEST ONSET OF ACTION Vastus Lateralis 34 +14 (5 – 120) minutes p < 0.05 Deltoid Time to Cmax after injection (minutes) Simons: J Allergy Clin Immunol 113:838, 2004 Epinephrine IM: Time to Onset Maximum pharmacodynamic effect occurs before 10 min Adapted from Simons FER, et al. J Allergy Clin Immunol. 1998;101:33-37. Auto injectors Needle Length found on auto injectors • 1.43 cm • May not penetrate vastus lateralis muscle •42% women 1 •2% men1 •12% children2 Twinject Epi-Pen Adrenaclick 1. Song TT et al. Ann Allergy Asthma Immunol 2005;94:539-42. 2. Stecher D et al. Pediatrics 2009; 124 (1): 55-70. Fatal Anaphylactic Reactions Most fatal reactions are unpredictable – Appropriate management after recovery from a severe reaction may be protective against a fatal recurrence2 – Epinephrine used in 62% of fatal reactions • 14% of time before cardiac arrest3 • 86% of time after cardiac arrest 1. Sampson HA, et al. N Engl J Med. 1992;327:380-384. 2. Pumphrey R. Curr Opin Allergy Clin Immunol. 2004;4:285-290. 3. Pumphrey RS. Clin Exp Allergy. 2000;30:1144-1150. 51 Epinephrine: Multiple doses Pt with food-induced anaphylaxis need TWO doses of epinephrine required up to 20% of the time before recovery Repeat dosing may be required after 5-15 minutes (optimal dosing interval unknown) NIAID Food Allergy Guidelines 2010 BIPHASIC ANAPHYLACTIC REACTIONS Treatment An insufficient dose of epinephrine given for the primary response is considered a risk factor Steroids do not prevent, but there seems to be a trend toward lower dose of corticosteroids administered in patients with biphasic rx [Administer adequate doses] Ellis AK, Day JH. Ann Allergy Asthma Immunol 2007;98:64-9. BIPHASIC ANAPHYLACTIC REACTIONS Severity of 2nd event is variable but can be fatal No biphasic response occurred in patients who had complete resolution of anaphylaxis symptoms in < 30 minutes If occurs, consider overnight hospital observation Ellis AK, Day JH. Ann Allergy Asthma Immunol 2007;98:64-9. Lieberman P. Ann Allergy Asthma Immunol 2005;95:217-26 Epinephrine IM: Potential Side Effect [These should not limit appropriate use] Anxiety, fear, restlessness Headache, dizziness, tremor, pallor Palpitations, tachycardia Increased risk with concurrent use of monamine oxidase inhibitors, tricyclic antidepressants, stimulant medications, cocaine abuse Increased risk with pre-existing cardiovascular disease, aortic aneurysm, uncontrolled hypertension, recent intracranial surgery NIAID Food Allergy Guidelines 2010 Epinephrine IM: Potential Side Effect [These should not limit appropriate use] Rare side effects: – – – – – – Angina Ventricular arrhythmias Myocardial infarction Pulmonary edema Sudden sharp increase in BP Intracranial hemorrhage More common with overdose any route More common with IV administration NIAID Food Allergy Guidelines 2010 Severe Anaphylaxis Position * Position Patient Supine Fatal cases associated with posture changes (Pumphrey RSH. JACI 2003;112:451-2.) 4 deaths occurred within seconds of a change to a more upright position 6 deaths occurred in individuals supported sitting up after shock Postulated mechanisms – • With sitting or standing venous return stops – • Vena cava will empty within seconds – • No blood flow to left heart results in pulseless electrical activity – • In this scenario epinephrine would likely not work # 2 DRUG OXYGEN Optimally with all patients with anaphylaxis Any patient with Hypotension or respiratory distress Any patient with 02 sat <95% Any patient requiring more than one Epi injection Face mask recommended over nasal prongs. Start with 6-8 Liter/minute #3 Drug IV FLUIDS For Hypotension (systolic <100) or any one who has not responded to first IM Epinephrine When there is shock in spite of increased vascular resistance 10% severe anaphylaxis not reversible with Epi* Select IV Fluids – .9 NaCl (isotonic crystalloid) – Hydroxyethyl starch (Hespan) (colloid) if saline not effective Bock SA, Munoz-Furlong A, Sampson HA. J Allergy Clin Immunol. 2001;107:191–193. IV FLUIDS Administer rapidly 5-10 mg/kg crystalloid over first 5-10 minutes, and total of 20-30 ml/kg first hour Apply BP cuff to bag of fluid or withdraw fluid and use a stopcock to infuse with a large 50 cc syringe (see picture) You may need to administer up to 50% of the intravascular volume Second line drugs (office setting) Diphenhydramine 1-2 mg/kg parentally Ranitidine 50 mg (1 mg/kg children) • IM same as IV for onset of action • If IV administer over 5 minutes Leukotriene modifiers: no recommendation for or against Atropine Bradycardia Βeta-Blocked anaphylaxis Dopamine Antihistamines: Time to Suppression Time to 50% suppression 101.2 min 79.2 min 51.7 min Fexofenadine Diphenhydramine IM Diphenhydramine PO Jones DH, et al. Ann Allergy Asthma Immunol. 2008;100(5):452-456. Antihistamines [A 2nd, 3rd, or 4th line drug] “The use of antihistamines is the most common reason reported for NOT using epinephrine and may place a patient at significantly increased risk for progression toward a life-threatening reaction.” H1 antihistamines are only useful for itching and urticaria 2nd generation H1 AH may be considered as rapid onset and less sedation (e.g. cetirizine) H2 antihistamine use has minimal support NIAID Food Allergy Guidelines 2010 H2-antihistamines In vitro studies suggest a benefit No adequate randomized and quasi-randomized controlled trials comparing H2-antihistamines with placebo or no intervention1 – No recommendations for clinical practice Avoid with food-induced anaphylaxis as may interfere with food allergen digestion and potentially augment a reaction2-3 1. Sheikh A, et al. Cochrane Database of Systematic Reviews 2007, Issue 1 .2. Untersmavr E, et al. JACI 2003; 112:626-23. 3. Scholl I, et al. AM J Clin Nutr 2005; 81:154-60. Additional Medications to consider Nebulized albuterol or levalbuterol for bronchospasm1 Albuterol does not relieve airways edema! 1. 2010 JTF Anaphylaxis PP. JACI (in publication). 2. Brown SGA et al. Emerg Med J 2004;21:149-54. 3. Kill C et al. Int Arch Allergy Immunol 2004; 134:260-1. 4. Wenzel V et al. N Engl J Med 2004; 350:105-13 CORTICOSTEROIDS Limited data supporting usefulness in anaphylaxis Never a substitute for Epi Minimal benefit for initial treatment 4-6 hours before onset of action Consider when a history of asthma Questionable benefit for severe, prolonged and biphasic reactions No difference in outcomes in severe IT anaphylaxis (37% of non-fatal did not get steroids) Dosage is unknown (recommended dose is usually methylprednisolone 1-2 mg/kg IV, 80-125 mg max or prednisone 1 mg/kg PO, 60-80 mg max) 2010 Anaphylaxis PP. JACI) NIAID Food Allergy Guidelines 2010 Additional Medications to consider Intravenous Epinephrine – Bolus Dosage (1:10,000 dilution)10-20 mcg (0.1-0.2 ml of a 1:10,000 dilution) at initial dose of 0.75-1.5 mcg/kg2 – Repeat as necessary Vasopressors (Dopamine) for unresponsive hypotension – Evidence suggest to use ≥ 10 mcg/kg/min IV2 Vasopressin: esp. for cardiac arrest. It is a potent vasoconstrictor, & inhibits NO and prostaglandin generation 3-4 1. 2010 JTF Anaphylaxis PP. JACI (in publication). 2. Brown SGA et al. Emerg Med J 2004;21:149-54. 3. Kill C et al. Int Arch Allergy Immunol 2004; 134:260-1. 4. Wenzel V et al. N Engl J Med 2004; 350:105-13 Glucagon For refractory hypotension in patients on βBlockers Initial dose of 1 to 5 mg IV followed by infusion of 5-15 mcg/min titrated against blood pressure Glucagon bypasses the β-adrenergic receptors Glucagon increases cAMP via stimulation of its own receptor, producing bronchodilation and helping to reverse hypotension Glucagon may induce nausea and vomiting 2010 JTF Anaphylaxis PP. JACI (in publication). Epinephrine Auto-injections Who needs one? Prescribe two doses of epinephrine for: – Hx of prior systemic allergic reaction – Patient with Food allergy (without hx of anaphylaxis) and concomitant asthma – Known food allergy to peanut, tree nut, fish, and crustacean shellfish (Even if no hx of anaphylaxis) – FPAS (oral allergy) – All food allergic pts (??) NIAID Food Allergy Guidelines 2010 Epinephrine for PFAS: Should one Rx? Up to 10% of patients with PFAS are at risk for a systemic reaction Severe reactions can occur upon the first ingestion of a food with cross-reactive allergens Systemic reactions to previously tolerated foods can occur The natural history of PFAS is unknown Peach, peanut, tree nuts, and mustard are high risk foods for PFAS with systemic symptoms Rx for reactions of any severity to cooked plant foods Discharge Plan for Patients with Food-Induced Anaphylaxis Epinephrine (2 doses) must be available at all times for patients at risk (e.g. school) Anaphylaxis emergency action plan Plan for monitoring auto-injector expiration dates Plan for arranging further evaluation and/or follow-up Printed info about anaphylaxis and its Tx NIAID Food Allergy Guidelines 2010 ACAAI-ACEP GO TO www.acaai.org and search for “SAFE” Death [We Must Prevent] Patient Resources http://www.ncbi.nlm.nih.gov/pubmedhealth http://www.niaid.nih.gov/topics/foodallergy /clinical/documents/faguidelinesexecsumma ry.pdf Physician Resources http://www.jacionline.org/article/S00916749(10)01566-6/fulltext http://allergyparameters.org/file_depot/010000000/3000040000/30326/folder/73825/2005%20Anaphyl Thank You DANA WALLACE, MD drdanawallace@gmail.com www.drdanawallace.com username: medicalprofessional password: allergy