Pediatrics review - Dr. Zucker 2011 compress
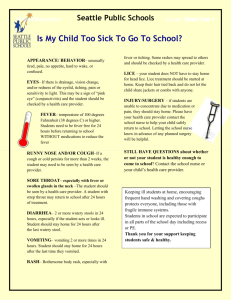
advertisement
GENERAL PEDIATRICS LMCC Review April 14, 2011 Feeding & Growth Breastfeeding CPS recommends exclusive breastfeeding for babies up to 6 months (when possible) Breast milk has a caloric content of ~20 Kcal/oz (0.67 Kcal/ml) Babies need 100-130 Kcal/Kg/day in 1st 3 months Feeding/growth spurts occur at 8-12 days, 3-4 wks, 3 mo, variably after that When comparing human breastmilk and cow’s milk the following is correct A. B. C. D. E. The ratio of whey:casein is higher in human milk Cow’s milk has a lower solute load Human milk has higher iron content Cow’s milk has lactose, human milk does not Human milk has sufficient vit D Nutritionally, how does breast milk compare to cow’s milk? Lower protein content - decreased solute load Greater whey:casein (70/30 vs 18/82, formula 60/40) CHO - both are lactose based (6.5% vs 4.5%) Fat - 30-50% vs 3.5-4% Vitamins - richer in A,C,E, lower in D & K Minerals - lower Fe but better absorbed Breast Feeding Benefits for Baby Immunological benefit secretory IgA, lactoferrin, lysozyme as GI defence Lower rate OM, LRTI, gastro, possibly UTIs, Hib Less allergenic Less constipating Better jaw/mandible development Attachment and ?Improved cognitive functioning Breast Feeding Benefits for Mother Postpartum weight loss & uterine involution Delayed return of fertility Bonding Pre-menopausal breast & ovarian Ca reduced Economical benefit Breast Feeding Issues Takes 3-7 days for milk supply to come in Jaundice is more common ineffective latch/sore nipples/engorgement Infections Breastmilk jaundice “Mom/baby team” risk of dehydration/ “breastfeeding jaundice” thrush , mastitis/abscess Reduced levels vitamin D & K Vitamin D Supplementation Rickets is still a problem in Canada! 400 IU per day All Breastfed infants Pregnant and nursing mothers in northern Canada Formula Fed infants living in northern Canada 800 IU per day - < 2 yrs breastfed babies with a risk factor Home above 55 degree latitude, darker skin, sun avoidance Community with high prevalence Vit D deficiency Vitamin D is found in milk, margarine, salmon, tuna, liver, kidney & from the sun Contraindications to Breast Feeding Maternal infections HIV, AIDS, active TB, malaria, herpes on breast, hepatitis Maternal sepsis Psychotropic meds or others crossing Chemo/radiation Alcohol/drug abuse Infant Galactosemia (lactose) *May breastfeed even with VZV Cow’s Milk Formula Always Fe fortified Many choices! Specialty formulas soy, lactose free, increased calories Protein hydrolysate formulas (eg.Alimentum, Nutramigen, Progestemil) Amino-acid based formulas (Neocate) Introduction of Solids cereals 4-6 months vegetables fruits meats Rest gradually in this order cow’s milk should be postponed until at least 10-12 months of age (renal load) 2% or 1% milk should be postponed until after second birthday (inadequate fat content) Infant Growth: Rules of Thumb Weight gain: Regain birth weight by 10-14 days (max 10% loss) Double birth weight by 5 months Triple birth weight by 1 year Quadruple birth weight by 2 years Increase by 5 lbs/year for rest of childhood Growth - Height Average length at birth 50 cm (20 inches) Increases by 50% by 1 yr Doubles by 4 yrs Triples by 13 yrs Ave growth 5-6 cm / yr (4 yrs-puberty) Growth- Body Mass Index (BMI) BMI helps to quantify the weight to height relationship BMI = weight(kg)/height (m)2 BMI of 20-25 is acceptable BMI > 30 indicates obesity BMI < 18 suggest severe anorexia or Failure to thrive Growth- Head Circumference 2 cm/month 1-3 months 1cm/month 3-6 months 0.5cm/month 6-12 months Most of growth is in first yr! 12 cm in first yr, 2 cm in 2nd yr, 6-8 cm rest of life Growth Monitoring Routinely recommended Height, weight, head circumference Plot on appropriate chart considering ethnicity, genetic syndromes (eg. Tri 21, Turner’s), and prematurity Prematurity, correct hc (18 mo), wt (24 mo), ht (40 mo) Only way to detect FTT Also detects chronic illness, feeding difficulties What is Failure to Thrive? US National Center for Health Statistics defines FTT for children < 2 yrs of age as: Weight <3rd-5th centile for age on more than one occasion Weight <80% of ideal body weight for age Weight crosses 2 major centile curves downwards on a standardized growth curve Exceptions: genetic/familial short stature, constitutional growth delay, SGA infants & preterm infants Caloric needs 0-10 kg: 100 kcal/kg/day 10-20 kg: 1000 + 50 kcal/kg/day >20 kg: 1500 + 20 kcal/kg/day Which growth curve demonstrates a growth pattern of FTT? A. B. C. A B C Which growth curve demonstrates a pattern of genetic short stature? A. B. C. A B C FTT- Infant Growth Caveats to normal growth velocity: >50% of babies shift their growth parameters upwards between birth and 3 months Nearly 30% of well babies shift their parameters downwards between 3 and 18 months Exclusively breastfed babies plot higher for wt at 0-6 months and lower at 6-12 months5 Growth Velocity Average age to “settle” on a growth curve is 13 months6 Downward shift seen with constitutional growth delay downward shift between 6 & 24 months may have decreased weight for height re-establish normal growth velocities by 3 yrs *Genetically Programmed curve is established by 18-24 months FTT- Assessment Grading of malnutrition: Grade Wt for Age (%) 0-Normal >90 1-Mild 75-90 2-Moderate 60-74 3-Severe <60 Wt for Ht (%) >90 81-90 70-80 <70 FTT- Assessment “Organic” vs. “non-organic” Historical way of viewing FTT Refers to presence/absence of diagnosis of major disease process or organ dysfunction “Non-organic” accounts for >80% Now felt to be more of a continuum Multifactorial process FTT- Assessment Under-nutrition results from: 1) 2) 3) 4) Decreased caloric intake Inadequate caloric absorption Increased caloric losses Increased caloric requirements FTT- Differential Diagnosis Decreased caloric intake: Inadvertent (decreased breast milk, improper formula preparation) Neglect or abuse Behavioural (ex. Food refusal) Pain (GERD, injury to mouth or esophagus) Fatigue /anorexia (anemia, cardiac dz, resp dz, RTA) Impaired swallowing (neurologic dz) Craniofacial abnormalities (cleft lip/palate, choanal atresia) Toxin (lead) FTT- Differential Diagnosis Inadequate Caloric Absorption & Increased Caloric Losses GI Pancreatic insufficiency (CF) Liver disease (biliary atresia, chronic cholestasis) Generalized malabsorption (CF, Celiac, short gut) Diarrheal state (infectious, post-infectious) Persistent vomiting (pyloric stenosis, GERD) Inflammatory disorders (IBD) Allergic gastroenteropathy Protein-losing enteropathy FTT- Differential Diagnosis Increased Caloric Losses cont’d Renal Protein loss Carbohydrate loss Inability to use nutrients Diabetes Mellitus Metabolic dz FTT- Investigations Careful and complete history taking and physical examination are ESSENTIAL Unless an illness other than primary undernutrition is suspected on Hx or P/E the yield of lab investigations is almost nil! Lab testing helps with diagnosis in 1.4% FTT- Investigations Non-specific “screening” Markers of nutritional status CBCD, ESR, lytes, BUN, Cr, venous gas Urine R&M, C&S Total protein, albumin, glu, Ca, PO4, Iron studies Zinc, vitamin levels Dependent on specific aspects of Hx & P/E Liver function tests Thyroid studies Stool OB, reducing substances, culture, O&P, trypsin Sweat test, immunoglobulins & celiac screen, viral serology (incl HIV), TB testing, immune w/up, metabolic w/up, CXR, ECG, milk scan FTT- Management Admit if : Suspect enviro. deprivation/neglect/abuse Suspect chronic dz which needs stabilizing Severe under-nutrition (consider if moderate) ie. <60% of median weight for age Failed out-patient management With hospitalization: greater likelihood of catch-up growth no change in developmental outcomes FTT- Management Inter-disciplinary approach!! Treat any underlying illness and provide nutritional support: Increase caloric intake 1.5-2 X RDA (120 kcal/kg/day x ideal wt)/current wt Estimate 150-200 kcal/kg/day FTT- Management Mild under-nutrition Ensure frequent feedings (q 3 hrs) Increase formula concentration (eg. 24 kcal/oz) Add calorie-rich foods to diet (butter, PB, oils) Provide dietary counseling Prescribe multivitamin with zinc and iron Follow-up frequently (?public health nurse) Expect catch-up growth at 2-3x regular rate in first month FTT- Management Moderate under-nutrition Determine caloric intake Consider whether investigations are necessary Increase caloric intake (150-200 kcal/kg/day) Ensure adequate protein (3-4 g/kg/day) Consider meal supplements (eg. Pediasure) Add Multivitamin Consider therapeutic doses of iron Monitor weight gain FTT- Management Severe under-nutrition Admit Initiate re-feeding slowly Consider using elemental formula Consider diluting formula May need ng continuous feeds or tpn Follow fluid and lytes status closely FTT- Long-term implications Persistent growth deficits Cognitive impairment Behaviour problems IMMUNIZATIONS Immunization Schedule (Recommended by the Canadian Immunization Guide) Age 2 mos 4 mos 6 mos 12 mos 18 mos 4-6 year q10 years Vaccine DaPTP-HIB, Pneum, Men DaPTP-HIB, Pneum,Men DaPTP-HIB, Pneum,Men MMR, Varicella, Pneum DaPTP-HIB, MMR DaPTP dTaP/dT Contraindications to Vaccines Strict - anaphylaxic or anaphylactic shock - encephalopathy Precautions - febrile reaction > 40.5 - shock collapse or hypotonia - hyporesponsive collapse - seizures Contraindications to vaccines Anaphylaxis to eggs: Severe immune deficiency: All live vaccines (MMR, VZV, OPV, BCG, Yellow fever, Oral cholera, Oral typhoid) Pregnancy: Influenza and yellow fever MMR and Varicella Anaphylaxis to neomycin: MMR and IPV Immunization Reactions DaPTP/Hib reactions occur within 72 hrs MMR reactions occur 5-12 days Delayed Immunization Age 1-6 years 0 mos:DPTP-Hib, MMR,HepB, P,V,MC 2 mos: Pentacel,MMR,HepB, Prevnar 4 mos: DPTP 12 mos:DPTP 4-6 yrs: DPTP 14-16 yrs: dTaP > 7 Years Old 0 mos: TdaP,Polio, MMR,V,Menj,HepB 2 mos: TdaP, Polio, HepB,MMR, V 6-12 mos: TdaP+Polio,HepB TdaP (no polio) q10 yrs thereafter Other Immunizations Hepatitis A & B Influenza HPV Rotavirus INFECTIOUS DISEASE Fever Temp > 38.3 Celsius rectal 0-1 mos: FSWU 1-3 mos: toxic = FSWU non-toxic and low risk (WBC 5-15, bands <5%, urine neg, well-looking, reliable family): investigate and follow Otitis Media Incidence: Peak: 15% to 20% 6 to 36 months 4 to 6 years decreases > 6 years old Etiology: S. pneumoniae, M. catarrhalis, non-type H. Flu, GAS & viral Otitis Media Risk Factors mid-face hypoplasia (Down Syndrome) daycare attendance Inuit/Aboriginal low SES 2nd hand smoke Otitis Media Treatment: 1st line: Amoxil 2nd line: High dose Amoxil, Clavulin, Macrolides, Cephalosporin T-Tubes if recurrent or persistent effusion Complications: hearing loss chronic effusion mastoiditis meningitis Sinusitis Mainly ethmoid sinus Predisposed by viral URTI, allergy, asthma, periodontal disease Same bugs as OM +/- anaerobes Presents with fever, purulent nasal discharge (> 10 days), periorbital tenderness, halitosis Treat with same Abx as OM, may need longer course (3 weeks) Meningitis Newborn period (LEG) Listeria E. Coli Group B strep 2 months - 12 years (SHIN) Strep pneumonia, N. meningitides Less common Hib with immunization Meningitis in abnormal hosts or anatomic defects: increased Pseudomonas, Staph, Salmonella, Serratia Complications SIADH seizures subdural effusions transient joint effusions (Ag-Ab reaction) hearing loss Urinary Tract Infection Newborn M › F (2) Children F › M (10) Schoolgirls - 5% Recurrence - 80% Vesicoureteral reflux - 35% Renal scarring - 50% All children ‹ 3 yrs U/S VCUG Urinary Tract Infections UTI Pyelonephritis KEEPPSS Klebsiella, E. Coli, Enterococcus, Proteus, Pseudomonas, Staph, Strep ampicillin + gentamycin IV initially then Amoxil or Septra po VUR prophylactic Septra or nitrofurantoin (or Amoxil) Higher grades may require surgery Osteomyelitis Organism neonate: Staph, GBS, E.Coli > 3mos.: Staph, Hib, Strep,Pseudomonas SS disease: Salmonella Diagnosis bone scan x-ray 10-12 days Septic Arthritis Monoarticular (trauma) Organism neonate group B strep, staph, E.Coli >3 mos Staph aureus Strep, Hib most common site is knee (40%) Fever and Rash A 14 year old male comes to you with a fever and rash for 2 days. He states that before the fever and rash he had started with red eyes, coryza, and cough. He has now developed a maculopapular rash starting at the head and moving to his toes. You look in his mouth and see little white ‘spots’. You are most concerned he has: A. B. C. D. E. Kawasaki disease Measles Rubella Scarlet Fever Erythema Infectiosum A 1 year old presents to your office with a new rash. Mum reports the baby had a high fever for two days with no associated symptoms. The fever has now disappeared as the rash appeared. The most likely organism causing the illness is: A. B. C. D. E. HHV-1 HHV-2 HHV-6 Group A Strep Mycoplasma Measles (First Disease) Paramyxovirus Stages incubation: 8-13 days prodrome: 4 C’s then fever with rash skin rash (erythematous, maculopapular, starts at hairline and spreads to face, trunk and extremities) Complications pneumonia encephalitis SSPE Scarlet Fever (Second Disease) Fever, pharyngitis, exanthem (starts in axilla, groin, neck, blanches,circumoral pallor, Pastias lines) Age › 3 yrs; recurrence Group A strep: erythrogenic toxin (2-5 days postStrep throat or GN) Treatment with Penicillin Complications cellulitis Rheumatic fever Rubella (Third Disease) Togavirus Congenital Postnatal mild disease suboccipital nodes maculopapular pink rash, starts on face, neck to extremities, spreads quicker than measles Roseola Infantum (Fourth Disease) HHV6 High fever rash maculopapular with cessation of fever High WBC low WBC Febrile convulsions Erythema Infectiosum (Fifth Disease) Parvovirus B19 No prodrome: red flushed face/slapped cheek, maculopapular rash with lacelike appearance Complications miscarriage/SA aplastic crises The number one cause of death in children between 1 month and 1 year of age is: A. B. C. D. E. Child abuse Sudden infant death syndrome Apparent life threatening events Drowning Sepsis ALTE/SIDS Apparent Life Threatening Event: Definition Clinical symptoms frightening to caregiver Combo of apnea, colour change, tone change, choking, gagging Apnea: 20 seconds of breathing cessation or shorter if associated with tone change, colour change, CV change ALTE Detailed Hx and Px Talk to person witnessing event Significant event? ALTE Differential Neuro- seizure GI- reflux Pulmonary- aspiration, apnea CV- arrhythmia Infection- sepsis, pertussis, RSV Metabolic Abuse ALTE Investigations Labwork +/- infectious workup EEG ECG/Echo UGI/pH probe CT head Monitor SIDS Unexpected death by Hx and Postmortem most common cause of death 1mo-1yr peak 2-4 months, 95% <6 months old SIDS Infant Risk Factors: prematurity age, sex prone sleeping bottle fed smoke environ. Thermal stress ethnicity prior illness winter months low birthweight Maternal Risk Factors low age low SES low education smoker drug use poor nutrition Gastroenterology/ Pediatric Surgery Colic Unexplained irritability/crying 2-3 wks to 3 mos At least 3 hrs/day > 3 days/week > 3 weeks duration ? Secondary to immature gut development Colic ++Gas/legs drawn up; otherwise well No proven treatment - rhythmic motion/sounds Ovol/Tylenol- no proven benefit Parental support and reassurance Abdominal Pain Acute: Ddx includes gastro, hernia, UTI, appendicitis, intussusception, malrotation, volvulus, HSP, SC Crisis, pneumonia, mesenteric adenitis, Chronic: > 3 episodes affecting activities > 3 months Organic (<10%): constipation, IBD, mass, PUD, GU, lactose intolerance Functional (90%): 8-10 yo peak, girls predominate, vague crampy periumbilical pain with no awakening, ppting or alleviating factors. Normal growth. Gastroesophageal Reflux Incompetence of lower esophageal sphincter improves by one year of age in most infants Complications apnea in infants aspiration pneumonia chronic cough/wheeze esophagitis- dysphagia,hemetemesis, Fe deficiency anemia Gastroesophageal Reflux Diagnosis pH probe Ba swallow nuclear scan endoscopy Gastroesophageal Reflux Treatment chalasia routine - attention to burping, small frequent feeds, 300 prone thickening feeds Medications: H2 blockers or PPI if esophagitis or gastritis present Domperidone for decreased gastric emptying A 6 week old male infant presents with a one day history of increasing severity of vomiting. Mum notes he is very hungry but appears to forcefully vomit all that he has eaten in a ‘projectile’ fashion. She now worries he is becoming more lethargic and dehydrated. The typical abnormality on laboratory investigations would be: A. Anemia B. Eosinophilia C. Hyperchloremic metabolic acidosis D. Hypochloremic metabolic alkalosis E. Respiratory alkalosis Pyloric Stenosis boy > girl 3 weeks - 3 months projectile vomiting (nonbilious) hungry infant feeds vigorously Pyloric Stenosis O/E:- dehydration, lethargy, weight loss, peristaltic waves L R, palpable “olive” Lab- hypochloremic alkalosis Investigation- U/S, UGI Rx: rehydrate and restore electrolyte balance - myotomy of pyloric muscle Intussusception 3 months - 3 years (up to 6 years) 5% anatomic abnormality found Meckel’s polyp duplication more frequent ileocolic or ileoileocolic Intussusception Clinical severe paroxysmal pain lethargy shock sausage shaped mass RUQ vomiting currant jelly stool Intussusception Lab x-ray barium enema density or gasless right side coil-spring sign Treatment reduction by barium enema surgical reduction Meckel Diverticulum 2% population year peak incidence 2 feet from ileocecal junction 35% ectopic gastric or pancreatic tissue painless rectal bleeding (typically bright red) 99Tc scan confirms diagnosis treatment: excision A 4 year old girl presents with longstanding constipation. The mother reports her daughter has always been constipated and has been challenging to treat with many different therapeutic interventions being tried. They describe her stools as long and thin. She is noted to not be growing well when plotted on a growth curve. He neurological exam is normal. She appears to have good anal tone with the absence of stool in the rectum. The best test to pursue for confirmation of the diagnosis is: A. MRI of the spine B. Contrast enema C. Colonoscopy with proximal large bowel biopsy D. Rectal biopsy E. No investigation required Constipation Def’n: passage of bulky or hard stool at infrequent intervals Retention of stool in rectum leads to encopresis in up to 60% Most causes are not organic but due to voluntary or involuntary retentive behavior Constipation DDx Dietary Behavioral Obstruction Dehydration Structural defects (fissures) Metabolic (hypothyroid,hypoparaT, hyperCa) Neuromuscular ( MMC, MD, spinal cord) Hirshsprungs Constipation- Treatment Dietary: increased fluid/fibre Stool softeners or laxatives Lactulose Lansoyl PEG powder Bowel evacuation (enemas) Bowel/toileting regimen Hirshsprung’s Disease Absence of ganglion cells in the bowel wall Most common cause of neonatal GI obstruction Aganglionic segment NB: failure to pass meconium within 48 hrs Hirshsprung’s Disease Constipation onset after 2 yr encopresis large caliber stool normal growth normal nutrition normal anal tone stool in ampulla Hirshsprung’s onset at birth no encopresis small stools assoc. FTT/poor nutrition abdominal distension normal anal tone ampulla empty Hirshsprung’s Disease Diagnosis: rectal biopsy shows absence of ganglion cells rectal manometry barium enema ->transition zone Treatment: resection aganglionic bowel colostomy, then pull through at 6 to 12 months of age Umbilical hernia Defect of central fascia beneath umbilicus Most common condition of abdominal wall Almost never incarcerate Strong family history and racial propensity Medical risk factors: Congenital hypothyroidism Prematurity Umbilical hernia DDx: Small omphalocele (looks like fixed hernia) Supra-umbilical hernia Refer to surgery if: Ring defect > 1.5 - 2 cm in diameter “elephant’s trunk” appearance Incarceration Not closing by 2 years of age UROLOGY / NEPHROLOGY Cryptorchidism 3.4% of NB, 0.7% of children > 1 year of age Bilateral in 20% Consequences- tumour, infertility, torsion,hernia Differential diagnosis Ectopic testes Retractile testes Absent testes surgical correction <2 year of age Hypospadius Sibling risk - 10% Undescended testes - 10-15% Not associated with UT anomalies Do not circumcise Enuresis Nocturnal , Diurnal, both Primary vs. Secondary 10% 5yr old, 5% 10 yr old, 1% 18 yr old Male > Female Familial maturational defect in bladder control Enuresis Treatment Rule out underlying cause (UTI, constipation, IDDM) Motivational maneuvers- star charts Alarm Medication- DDAVP, TCA The typical features of nephrotic syndrome include: A. B. C. D. Hypoalbuminemia, proteinuria, edema, hyperlipidemia Proteinuria, hematuria, hypertension, edema hyperglycemia, glucosuria, ketonuria, weight loss Proteinuria, hematuria, arthritis, purpura Proteinuria Def”n: >150mg/24 hr (>4mg/m2/hr) Nonpathologic: Postural- incr. in upright position 10x Collection done in supine and upright positions Febrile Exercise Proteinuria Tubular: Hereditary- cystinosis, Wilson dis., RTA Acquired- antibiotics, ATN, cystic diseases, heavy metal Glomerular: Nephrotic syndrome Glomerulonephritis, tumour, drug, congenital Nephrotic Syndrome Minimal change disease the most common (76%) Membranous (8%), Focal Segmental (7%) Diagnosis proteinuria(>40 mg/m2/hr) hypoalbuminemia hyperlipidemia edema Nephrotic Syndrome Treatment Renal biopsy prednisone Unusual age (<1yr, adol.) Steroid resistant/ frequent relapse HTN, decreased renal function Complications hypercoagulability infections Drug side effect- steroids, immunosuppressants Marked eyelid edema in a 2-year-old boy with minimal change disease and nephrotic syndrome. Eyelid edema in any child should prompt the performance of urinalysis, rather than the presumption of allergy. Severe scrotal edema in a 6-year-old boy with nephrotic syndrome. Hematuria Microscopic (> 5 rbc/hpf) vs. Macroscopic Approach based on anatomy: Kidney Ureter Bladder Urethra Hematuria Glomerular Tubulointerstitial Hematologic causes platelets, SS disease, renal vein thombosis Anatomic abnormalities ATN Infections Hypercalciuria Drugs Tumour, trauma, cysts, vascular Exercise Hematuria: Work-up STEP 1: STEP 2: CBC, urine culture, Cr, C3, U/S 24 hr urine- Cr, protein, calcium ASOT/antiDNase-B, T/S, ANA, coags, urine RBC morphology, SS screen, VCUG (if infection/lower tract suspect) STEP 3: biopsy Glomerulonephritis Proteinuria, hematuria, hypertension, edema Etiology: Acute post Strep GN, IgA Nephropathy, HSP, SLE Nephritis, RPGN, MPGN Acute Post Strep GN: school-aged, mean age 7, 2:1(M:F), 1-2 wks between infection and presentation, dark urine, edema Dx: UA, ASOT, anti DNAase B, low C3 (and in 6-8 wks) Management: fluid/Na restriction, diuretics +/- antiHTN 98% recover completely, sx resolve in 3-4 wks Hemolytic Uremic Syndrome Diarrheal and non-diarrheal causes E. Coli 0157:H7 verotoxin Present with diarrhea followed by bloody diarrhea 5-7 days later- Triad microangiopathic hemolytic anemia thrombocytopenia renal failure Hemolytic Uremic Syndrome Treatment supportive lasix infusion Dialysis No role for antibiotics, steroids Prognosis: 10-30% morbidity 5-10% mortality RHEUMATOLOGY A 5 year old female is admitted with acute abdominal for the past week. It is intermittent and severe. You are called to her bedside the next day for an evolving rash that is mainly on the lower limbs and appears to be raised bruising. At the same time she passes what appears to be a bloody stool. You note on review of the investigations from last night that she has 10-20 RBC/hpf on urinalysis. What is the best treatment option you can offer to provide her with the best long term prognosis? A. B. C. D. E. Supportive care IVIG Aspirin Antibiotics to cover Group A strep IV steroids With this condition, what will you tell the family with regards to necessary followup? A. B. C. D. She will need an echocardiogram as there is a risk of coronary aneurysms She will need regular renal monitoring as there is a risk of long term renal impairment There is no need for regular monitoring after the illness resolves as there are no long term sequelae She will need long term antibiotic prophylaxis A 2 year old male was seen three days ago for a three day history of fever and neck swelling. He was sent home with antibiotics to treat a cervical adenitis that measures 2x2cm. He now returns 3 days into the antibiotics with persistent fever and no improvement in his neck swelling. You note he has red conjunctiva and his lips are red and cracked. The mother is worried he is reacting to the medication as he has a new rash. What would be the next best step in managing this child’s situation? Admit for IV antibiotics Change his oral antibiotics and follow up in 2 days to ensure good response Send off serology for EBV infection and discontinue the antibiotics Admit for IVIG Perform an echo and if abnormal initiate IVIG Henoch Schonlein Purpura Immune-mediated systemic vasculitis of small vessels Often preceding URTI Ages 4-10yr; recurs in 1/3 Classically involves, skin GI joints (75% have arthralgias) kidney (20% develop gross hematuria) HSP - Skin Palpable nonthrombocytopenic purpura May be presenting sign in only 50% of patients. Purpura involves dependent areas of the body. Edema of the hands, feet, and scalp often an early finding (20-40%) Slide 1 HSP - Gastrointestinal 45 to 85% of children with HSP major hemorrhage (5%) intussusception (2%) occult bleeding (33%) HSP Treatment Steroids used if severe/life-threatening GI involvement Doesn’t affect renal outcome Must monitor for renal involvement- may occur late Watch for recurrence education Kawasaki Disease Criteria F ever for 5 days Plus 4 of 5: E xanthem E xtremities L ymph nodes (>1.5 cm) M ucosal changes C onjunctivits “feel my conjunctivitis” Kawasaki Disease CVS coronary aneurysms- 20% of cases Risk < 5% if treated Phases Acute- febrile 1-10 days Subacute (peeling, afebrile, high platelets/ESR) 10-21 days Convalescent (normalize plt/ESR) >21 days Kawasaki Disease Associated Features Uveitis Hydropic gallbladder Carditis Pancreatitis arthritis Sterile pyuria (urethritis) Diarrhea Aseptic meningitis Kawasaki Disease Treatment IVIG Aspirin- high followed by low dose Echo at baseline and at 6-8 weeks for coronary aneurysms ONCOLOGY Acute Lymphocytic Leukemia Most prevalent malignancy under 15 yoimmature lymphoid cells accumulate in the BM (lymphoblasts) 80% of all cases of acute leukemias : peak 2-6yo Poor prognosis if < 2yrs or > 10yrs, WBC > 50,000, CNS or testicular involvement at diagnosis, T-Cell or B-Cell, Pseudodiploidy (presence of translocations within leukemic cells), and hypodiploidy (< 46 chr. in leukemic cells), L3 morphology of blasts ALL- Clinical Features Bone marrow failure: anemia, low plts, neutropenia Lymphadenopathy Hepatosplenomegaly Bone pain Acute Lymphocytic Leukemia Relapse 30 - 40% bone marrow CNS testes Long term problems secondary tumours infertility learning disability Neuroblastoma Malignancy of neural crest cells Most common neoplasm in infants Most in first 4 yrs (mean=2yo) Most common site of primary tumor is abdomen (abd. mass ,abd. pain ,HTN ) Thoracic tumors: resp. distress H & N-Horner syn. Constitutional s/sx Metastases common to bone, BM, liver lung (50%) High catecholamines in 90% Wilms’ Tumor 5-6% of childhood Ca: 75% before 5yo Palpable abdominal mass, HTN, hematuria Bilateral in 5% Association with aniridia, hemihypertrophy, and Beckwith Wiedmann Syndrome in 12-15% Retinoblastoma Bilateral (40%) hereditary - AD osteogeneic carcinoma Unilateral (60%) sporadic Slide 3 Brain Tumors Second most common tumor-most common solid tumor cerebellum 40%, brainstem and 4th ventricle 15%, suprasellar 15% Presentation depends on location Common signs: vomiting, papilledema, lethargy, headache, personality change, ataxia, loss of vision, seizures, focal neurologic signs, nystagmus HEMATOLOGY This child is at risk for: A. B. C. D. E. Overwhelming sepsis Bone pain Hypersplenism Stroke Growth failure With this blood smear, you would expect the CBC to show: A. B. C. D. Low Hgb, low MCV, high retics, high RDW Low Hgb, low MCV, low retics, high RDW Low Hgb, high MCV, low retics, normal RDW Low Hgb, normal MCV, normal retics With this blood smear, which statement is most accurate A. B. C. D. E. This condition is autosomal recessive Hemolysis is not a feature of this disease Bony crises are a common sequelae The osmotic fragility test is a diagnostic test Hemoglobin electrophoresis is a diagnostic test Anemia Low Retics (underproduction) MCV- Low- iron, thal,lead, chronic - Normal- renal, thyroid, infection - High- B12, folate, fanconi High Retics (increased loss) Blood Loss Hemolysis- intrinsic - extrinsic Iron Deficiency Anemia Decrease in RBC Hb due to inadequate Fe stores Etiology: poor dietary intake, early transition to cow’s milk, high requirements with growth spurts, cow’s milk intolerance, chronic GI blood loss Diagnosis: microcytic anemia, low serum iron, ferritin, S/sx: irritability, anorexia, lethargy, pale, tachycardia, systolic murmur Slide 1 . Spherocytosis Autosomal Dominant, northern European abnormal membrane protein- Spectrin leads to hemolysis- less flexible newborn- jaundice < 24 hr disease can be mild, moderate or severe mild- mod. Anemia, reticulocytosis and splenomegaly Dx- osmotic fragility test Rx.- support, splenectomy From CD Atlas, MCCQE Toronto Notes, 2003 G6PD Most common RBC enzyme defect X-linked, African, Mediterranean susceptible to oxidation stress--> Hgb precip.--> membrane damage Precipitating agents infection, vit. C, fava bean, benzene, Medications (nitrofurantoin, antimalarial, sulfa, nalidixic acid, vit. K analog) intermittent hemolysis, chronic hemolysis, incidental with anemia and retics smear- bite cells Sickle Cell Disease Newborn asymptomatic first sign (6 mos) - hand-foot syndrome Crises sequestration vaso-occlusive aplastic(Parvovirus) hyperhemolytic infections Prevent infections (considered asplenic) From CD Atlas, MCCQE Toronto Notes, 2003 Slide 2 Classic Hemophilia Factor VIII deficiency: X-linked ie asymptomatic female carriers transmit to sons Symptoms: excessive bruising with ambulation intramuscular hematomas from minor trauma hemarthrosis: often spontaneous hematuria risk for intracranial hemorrhage & bleeding into the neck Classic Hemophilia Severity depends on level FVIII in plasma mild 6% to 30% moderate 1% to 5% severe < 1% Pts with mild FVIII deficiency experience only prolonged bleeding following tooth extraction, surgery or bleeding Lab: PT normal, PTT greatly prolonged Classic Hemophilia Treatment: - prevention of trauma - FVIII concentrates - strict avoidance of drugs that affect platelet function Immune Thrombocytopenic Purpura (ITP) Thrombocytopenia mediated by auto antibodies causing destruction Peak age 2-6yo: associated with antecedent viral infection Most resolve in 4-6wks: 20% duration > 6mos Clinical Features: purpura, petechiae, bleeding from mouth, gums, kidney, GIT, no hepatosplenomegaly Treatment- IVIG, steroids Slide 5 CHILD ABUSE Child Abuse Physical - 80% Sexual - 15% Physical and emotional neglect Munchausen by proxy 2nd cause of death in 1-6mos 1/3:1/3:1/3- <1yo:1-6yo:>6yo Premature and developmentally impaired have 3x risk Red Flags Recurrent injury/ingestion Injury poorly explained/ out of proportion High risk injuries: scald, cigarette,spiral fracture, retinal hemorrhage Injury pattern/site High risk environment preterm, neurologic impairment single parent family stress psychiatric illness Slide 4 Slide 1 Slide 2 Slide 6 Slide 7 Slide 3 ADOLESCENCE Adolescence- HEEADSS Home Education Eating Activities Drugs Sexuality Suicide Adolescent Suicide Warning Signs Depression Psychosomatic complaints Acting out Previous attempt Family history ORTHOPEDICS Growing Pains 3 - 6 years Night time: poorly localized Pain in shins, calves, thighs Heat, massage, Tylenol Normal physical exam Congenital Dislocation Hip (Developmental Dislocation Hip) Age: 2 months to 2 years Signs: limitation of abduction tight adductors shortening of leg asymmetric skin folds + Galeazzi sign (one knee lower than other) Congenital Dislocation Hip Assess stability: Ortolani(reduce) & Barlow(dislocate) signs Treatment: triple diaper first for mild cases of subluxation (x 6 to 8 weeks) < 6 to 8 months, Pavlik harness > 8 months, traction closed reduction spica cast Slide 2 Metatarsus Adductus Forefoot faces in rather than lining up with 2nd metatarsal May be secondary to intrauterine positioning Early treatment is stretching If rigid may require casting to correct An 8 year old male comes to clinic with a 5 day history of limp together with pain in the right hip and upper thigh. He is otherwise healthy and has been on no medications. Exam demonstrates limited ROM in the hip and a normal knee exam. An xray has been taken . The most likely diagnosis is. A. B. C. D. E. Avascular necrosis of the head of the femur Slipped Capital Femoral Epiphysis Fractured femoral neck Septic arthritis Growing pains Legg Calve Perthes Disease Avascular necrosis femoral head males > females 5 to 9 year old:sx: painful hip, limp, referred pain X-ray: lucency, widening of the distance and eventual distortion of the femoral head Treatment: casts to keep hip in abduction & medial rotation surgery This 12 year old child comes with a 2 week history of increasing pain in the right leg and limping. He has a hard time flexing his hip and prefers to keep it externally rotated when examined. He gives no history of trauma. There has been no illness. The best management of this child would be A. B. C. D. E. Urgent consult with orthopedics Semi-urgent referral to the ortho clinic Routine referral to the ortho clinic Expectant management, return if symptoms do not resolve in 2-4 weeks Follow-up xrays in 2 weeks Slipped Capital Femoral Epiphysis Most common in obese boys in adolescence femoral epiphysis slips posteromedially off the metaphysis unilateral or bilateral gradual or sudden causes pain & limitation of motion abduction & internal rotation are limited Klein’s line on xray Treatment: pinning to prevent further slipping Osgood-Schlatter’s Disease Common cause of knee pain Mostly in athletic or overweight kids Pain arises in tibial tuberosity (at site of attachment of patellar tendon)after exercise or kneeling Treatment mainly supportive: includes reduced physical activity +/- bracing DERMATOLOGY Slide 3 Pityriasis rosea Prodrome rare: fever, malaise, arthralgia, pharyngitis Herald patch: solitary 1-10cm annular papular lesion anywhere on body 5-10 days later, widespread symmetrical eruption involving trunk & proximal limbs < 1cm slightly raised pink/brown papules eruption, fine scale, especially at periphery Pityriasis Rosea Christmas tree pattern on back Duration: 2 to 12 weeks Mild to severe pruritus ? Viral trigger Treatment: antipruritic/antihistamine lubricating lotion or topical cortosteroid if moderate to severe pruritus Impetigo + Prevalent during hot, humid months + Common in infants & children Initiated by infection with Grp.A hem.strep Bullous impetigo 2o to Staph Aureus Grp.2 phase type Erythematous macule...vesicles & pustules Impetigo Bullae with erythematous halo...honey coloured crusts (non bullous form), superficial & rupture easily (bullous type Spread by contact to other parts of body Treatment: local measures...personal hygiene compresses to remove crusts systemic antibiotic Atopic Dermatitis Inflammatory skin disorder erythema...edema...intense pruritus... exudation, crusting & scaling > risk to develop allergies & asthma Atopic Dermatitis Infancy: 1st 2 to 3 months weepy patches on cheeks, neck, wrists, hands & extensor aspect extremities Childhood: involvement of flexural areas, especially popliteal & antecubital fossae also, neck, wrist, behind ears, > with age; > drying & thickening of skin Atopic Dermatitis Other signs: “Mask of atopic dermatitis” Hyperpigmentation of skin Lichenification Atopic Dermatitis Itch - scratch - itch cycle Rx: antihistamines topical corticosteroids topical immune modulators (Protopic) hydrating lotions Slide 2 Slide 1 Seborrheic Dermatitis Begins on scalp as “cradle cap” Involvement behind ears, sides of nose & eyebrows Greasy, brownish scales Shorter course than atopic dermatitis Responds more rapidly to treatment than atopic dermatitis Treatment: General Guidelines Keep bathing at minimum Use of non-soap cleansers Cotton garments/avoid wool Keep nails cut short Avoid environmental triggers Treat superinfections with systemic antibiotics Staphylococcal diaper dermatitis. There are numerous thin-walled pustules surrounded by erythematous halos, as well as multiple areas in which pustules have ruptured, leaving a collarette of scale around a denuded erythematous base. Irritant or ammoniacal diaper dermatitis. Note the involvement of the convex surfaces and the sparing of the intertriginous creases. Candidal diaper dermatitis. The eruption is bright red with numerous pinpoint satellite papules and pustules. Intertriginous areas are prominently involved. Psoriatic diaper dermatitis. This child had a persistent diaper rash that did not respond to routine therapy. Note that scaling is not as intense as in psoriatic lesions seen elsewhere on the body. Erythema Multiforme Erythema multiforme (EM minor). A, The characteristic target lesions are symmetrically distributed. B, In these typical target lesions with central dusky areas, the peripheral rims are beginning to vesiculate. C, In this case, the peripheral rims have become frankly bullous. (C, Courtesy of Michael Sherlock, MD, Lutherville, Md.) Stevens-Johnson Syndrome Stevens-Johnson syndrome (EM major). A, Severe bullous and erosive lesions cover the face, neck, upper trunk, and proximal extremities. Note the ocular and oral involvement. B, Typical bullae, target lesions, and erosions of the lips are seen in this boy. C, This child has numerous vesicles and bullae of the oral mucosa along with formation of a shaggy white membrane consisting of sloughed debris. (C, Courtesy of Michael Sherlock, MD, Lutherville, Md.) Milia White-yellow papules Epidermal inclusion cysts Face, gingivae, palate Ebstein pearls Neonates: Occur spontaneously Resolve spontaneously (weeks-months) Older children: Occur at site of trauma (blisters, abrasions) May not resolve spontaneously Erythema Toxicum Neonatorum White papule/pustule (1-2mm) surrounded by red wheal Localized or generalized Palms and soles spared Usually starts ~ day 2 New lesions continue to appear as rash waxes and wanes up to 10 days Less common & delayed presentation in prems Eosinophils on scraping BENIGN & SELF-LIMITING CLASS OF 2011 FACULTY OF MEDICINE UNIVERSITY OF OTTAWA GOOD LUCK!