Snímek 1
advertisement

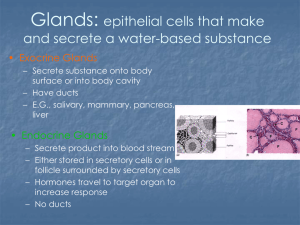
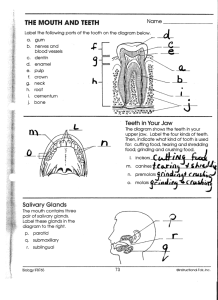
Pathophysiology of salivary glands Zuzana Humlová Salivary glands - Anatomy Minor salivary glands Hundreds throughout mouth Major salivary glands (3 on each side of face) Parotid Gland (cheek) Submandibular gland (under angle of the jaw) Sublingual gland (under tongue) Minor salivary glands The minor salivary glands are shown to be organs whose function is decisively involved in symptoms such as xerostomia, stomatodynia, and what is known as "denture intolerance". Moreover, proper secretion of the palatine glands is of crucial importance for the physical retention of maxillary full dentures. There are no connections between secretory rates of major and minor salivary glands. The effect of certain drugs on salivary production and thus on the symptoms of hyposalivation seems to be considerable. Parotid Gland Largest salivary gland Most prone to bacterial sialadenitis Facial nerve bisects gland Superficial lobe Deep lobe Lies over maxillary bone Neonatal sialadenitis Acute bacterial sialadenitis Chronic sialadenitis Superior to mandible Anterior to angle of jaw and auricle Stensen's Duct (Parotid Papilla) Opens out adjacent to maxillary second molar Milking parotid gland will expel drop at duct Gl. parotis Submandibular gland Second largest salivary gland Located within submandibular triangle Recessed immediately below mandible Overlies hypoglossus muscle Hypoglossal and lingual nerves overly gland Wharton's Duct Opens adjacent to lingual frenulum Gl. submandibularis Physiology and Function Saliva function Controls oral pH Assists with food intake Lubricates food bolus Contains amylase for carbohydrate digestion Mouth cleansing and oral hygiene Saliva limits oral pathogen growth Reduces oral odor (halitosis) Saliva content Water 99,4% Organic compounds – mucin, amylase, lysozym, immunoglobulin A Anorganic compounds – HCO3-, I, K, Cl, Na, Ca, phosphates and others. Saliva production Differential saliva production by glands Unstimulated salivation (Salivary gland at rest) 1.5 Liters produced per day (basal rate) Major salivary glands: 90% of saliva produced Submandibular and sublingual glands: 70% of saliva Stimulated salivation Saliva production increases 5 fold Parotid gland produces majority of saliva Regulation of secretion Innervation Parasympathetic innervation to major salivary glands Otic ganglion fibers supply Parotid Gland Submandibular ganglion supplies other major glands Sympathetic innervation promotes saliva flow Stimulates muscle contractions at salivary ducts Testing of saliva production The Škach test Unstimulated production – collection of saliva into container during 15 min Stimulated production – collection of saliva during 15 min of chewing parafine gum Measuring of both amounts during 2x15 min Normal levels: greater than 8-10 ml Pathologic levels: under 8 ml Xerostomia Definition Decreased saliva production Physiology: Saliva plays vital role in dental health Re-mineralizes enamel Buffers cariogenic acids Removes food residue Inhibits bacterial growth Causes of Xerostomia Medications (anticholinergic affect) Tricyclic Antidepressants Antispasmodics Neuroleptics MAO inhibitors Antiparkinsonian agents Lithium Central Adrenergic Agonists (antihypertensives) Diuretics Decongestants Antihistamines Bronchodilators Other causes Radiation therapy to head and neck Salivary Gland surgery Sjogren's Syndrome Amyloidosis Human Immunodeficiency Virus (HIV Infection) Diabetes Mellitus Major Depression Granulomatous Disease Sarcoidosis Tuberculosis Leprosy Other diseases Sjögren's sy Felty's sy Diabetes, hyperthyreosis, anemia, avitaminosis B, hepatopatia Sjögren's sy Sjögren's syndrome (SS) is a relatively common autoimmune connective tissue disorder. It is most frequent in middle-aged women. About 30% of patients with autoimmune disorders such as RA, SLE, scleroderma, vasculitis, mixed connective tissue disease, Hashimoto's thyroiditis, primary biliary cirrhosis, or chronic autoimmune hepatitis develop SS. Genetic associations have been found (eg, HLA-DR3 antigens in whites with primary SS). Pathophysiology Salivary, lacrimal, and other exocrine glands become infiltrated with CD4+ T cells and with some B cells. The T cells produce inflammatory cytokines (eg, IL-2, γ-interferon). Salivary duct cells also produce cytokines, eventually damaging the secretory ducts. Atrophy of the secretory epithelium of the lacrimal glands causes desiccation of the cornea and conjunctiva (keratoconjunctivitis sicca). Lymphocytic infiltration and intraductal cellular proliferation in the parotid gland cause luminal narrowing and in some cases formation of compact cellular structures termed myoepithelial islands; atrophy of the gland can result. Dryness and GI mucosal or submucosal atrophy and diffuse infiltration by plasma cells and lymphocytes may cause symptoms (eg, dysphagia). Symptoms and Signs SS often affects the eyes or mouth initially and sometimes exclusively. Dry eyes can produce irritation and photosensitivity. In advanced cases, the cornea is severely damaged, epithelial strands hang from the corneal surface (keratitis filiformis), and vision can be impaired. Diminished saliva (xerostomia) results in difficulty chewing, swallowing, secondary Candida infection, tooth decay, and calculi in the salivary ducts. Taste and smell may be diminished. Dryness may also develop in the skin and in mucous membranes of the nose, throat, larynx, bronchi, vulva, and vagina. Dryness of the respiratory tract may produce cough or lung infections. Alopecia may occur. Parotid glands enlarge in 1⁄3 of patients and are usually firm, smooth, and mildly tender. Chronic salivary gland enlargement is rarely painful. Arthritis occurs in about 1⁄3 of patients and is similar in distribution and character to RA. Other common extraglandular manifestations include generalized lymphadenopathy, Raynaud's phenomenon, parenchymal lung involvement (which is common but infrequently serious), and vasculitis that can occasionally affect the peripheral nerves or CNS or cause skin rashes (including purpura), glomerulonephritis, or mononeuritis multiplex. Kidney involvement can produce renal tubular acidosis, impaired concentrating ability, kidney stones, or interstitial nephritis. Pseudolymphoma, malignant lymphoma, or Waldenström's macroglobulinemia can develop; patients develop non-Hodgkin lymphoma at 40 times the normal rate and require careful follow-up. Chronic hepatobiliary disease, pancreatitis (exocrine pancreatic tissue is similar to that of salivary glands), and fibrinous pericarditis may also occur. Diagnosis SS should be suspected in patients with scratchy or dry eyes or dry mouth, enlarged salivary glands, purpura, or renal tubular acidosis. Such patients should receive diagnostic tests that can include evaluation of the eyes and salivary glands and serologic tests. Diagnosis is based on 6 criteria: eye symptoms, oral symptoms, eye tests, salivary gland involvement, autoantibodies, and histopathology. SS is probable if ≥ 3 criteria (including objective criteria) are positive and definite if ≥ 4 criteria are positive. Eye symptoms consist of ≥ 3 mo of either dry eyes or use of tear substitutes ≥ 3 times/day; slit-lamp examination may also confirm dry eyes. Oral symptoms consist of > 3 mo of daily dry mouth sensation, daily use of liquids to aid in swallowing, or swollen salivary glands. Ceratoconjunctivitis sicca Candidasis oralis The Schirmer test measures the quantity of tears secreted in 5 min after irritation from a filter paper strip placed under each lower eyelid. A young person normally moistens 15 mm of each paper strip. Most people with SS moisten < 5 mm, although about 15% of test results are false-positive and 15% are false-negative. Ocular staining with an eyedrop of rose bengal or lissamine green solution is highly specific. Slit-lamp examination showing a fluorescein tear breakup in < 10 sec is also suggestive. Salivary gland involvement can be confirmed by abnormally low saliva production (≤ 1.5 mL/15 min) as measured by salivary flow, sialography, or salivary scintiscanning, although these tests are less often used. Serologic criteria have limited sensitivity and specificity. They include antibodies to Ro (SS-A) or to nuclear antigens (termed La or SS-B autoantibodies), antinuclear antibodies, or an elevated level of antibodies against γ-globulin. Rheumatoid factor is present in > 70% of patients. ESR is elevated in 70%, 33% have anemia, and up to 25% have leukopenia. Biopsy of minor salivary glands in the buccal mucosa should be performed if diagnosis is not clear. Histopathologic involvement is confirmed if labial minor salivary glands show multiple large foci of lymphocytes with atrophy of acinar tissue. Haematoxylin and eosin stained section of a labial gland from a patient with Sjogren's syndrome showing (A) a periductal focus and (B) an area of more extensive lymphocytic infiltration associated with a proliferating duct. Mason, G I et al. Mol Pathol 2003;56:52-59 Copyright ©2003 BMJ Publishing Group Ltd. Prognosis and Treatment The disease is chronic, and death may occasionally result from pulmonary infection and, rarely, from renal failure or lymphoma. Other connective tissue disorders usually worsen prognosis. There is no specific treatment for the basic process. Dry eyes should be treated with OTC lubricating eyedrops qid and prn. Skin and vaginal dryness can be treated with lubricants. Mouth dryness may be avoided by sipping fluids throughout the day, chewing sugarless gum, and using a saliva substitute containing carboxymethylcellulose as a mouthwash. Drugs that decrease salivary secretion (eg, antihistamines, antidepressants, other anticholinergics) should be avoided. Fastidious oral hygiene and regular dental visits are essential. Stones must be promptly removed, preserving viable salivary tissue. The pain of suddenly enlarged salivary glands is generally best treated with warm compresses and analgesics. Pilocarpine, 5 mg po tid to qid, or cevimeline HCl, 30 mg po tid, can stimulate salivary production but should be avoided in patients with bronchospasm and closed-angle glaucoma. Felty sy Young people RA Splenomegaly Lymphadenopathy Anemia Thrombocytopenia Neutropenia Fever, loos of weight, tiredness Gramm/positive infections Management of xerostomia Management Consider stopping offending medication Commercial Saliva substitute Fluoride Supplementation Use 1.1% Fluoride gel daily Fluoride toothpaste Scrupulous dental care is essential Ptyalism Pathophysiology Normal Submandibular Saliva production 0.100.15 ml/min Ptyalism may result in 1-2 L/day of Saliva loss Mechanisms of excessive Saliva Decreased Saliva swallowing and clearance Excessive Saliva production Neuromuscular disease Anatomic abnormalities Causes Saliva Overproduction Pregnancy (Ptyalism Gravidarum) Hyperemesis Gravidarum Excessive starch intake Gastrointestinal causes Gastric distention or irritation Gastroesophageal Reflux Acute Gastritis or Gastric Ulcer Pancreatitis Liver disease Medications and toxins Clozapine (Clozaril) Potassium Chlorate Pilocarpine Mercury Poisoning Copper Arsenic poisoning Antimony (used to treat parasitic infections) Iodide Bromide Aconite (derived from Aconitum napellus root) Cantharides Stomatitis and localized oral lesions Aphthous Ulcers Oral chemical burns Oral suppurative lesions Alveolar abscess Epulis Oral infectious Lesions Dental Caries Diphtheria Syphilis Tuberculosis Small Pox Difficulty Swallowing Saliva Infections Tonsillitis Retropharyngeal Abscess Peritonsillar Abscess Epiglottitis Mumps Chancre Actinomycosis Bone Lesions Jaw fracture or dislocation Ankylosis of the temporomandibular joint Sarcoma of the jaw Neuromuscular disorders Cerebral Palsy Mental retardation Bulbar Paralysis Pseudobulbar paralysis Bilateral Facial Nerve Palsy Cerebrovascular Accident Myasthenia Gravis Hypoglossal Nerve palsy Rabies Botulism Miscellaneous Causes Radiation therapy Macroglossia Dental malocclusion Management Non-specific Treat specific causes as below General measures to reduce Saliva Tooth brushing and mouthwash has drying effect Reduce starch intake from diet Orthodontic appliances that aid swallowing Upper plate to cover palate with movable beads Aids lip closure Directs Saliva toward pharynx Anticholinergic Medications (if refractory to above) Glycopyrrolate Adults: 0.5 to 2 mg PO qd to tid prn Children: 0.04 mg/kg PO qd to tid prn Scopolamine Patch 1.5 mg applied every 72 hours prn Advanced procedures in severe and refractory cases Botulinum toxin A Salivary Gland injection Radiation therapy Performed under ultrasound guidance Porta (2001) Psychiatry 70:538-40 Borg (1998) Int J Radiat Oncol Biol Phys 41:11139 Surgery Submandibular Gland excision or duct relocation Parotid duct relocation or ligation Salivary denervation (transtympanic neurectomy) Specific measures Treat Nausea with Antiemetics Treat Gastroesophageal Reflux Neuromuscular causes Speech pathology (e.g. swallowing mechanism) Occupational therapy (e.g. head-back wheelchair) Neurology consultation Biofeedback Oral diseases including dental malocclusion Dentist or orthodontist Macroglossia or Tonsillar Hypertrophy Otolaryngology Sialadenitis Acute – viral and bacterial infection Chronic – bacterial, fibroproductive, post-actnic, specific (actinomycosis, syfylis, TBC), immunosialadenitis Acute viral sialadenitis Parotitis acuta Paramyxovirus Neurotrophic effect – n.VIII Affection of gonadal tissues, pancreas, central nervous systém Incubation: 18 days Whole life immunity Acute bacterial sialadenitis Ascendent ductal infection Dehydratation, diabetes, renal diseases, wrong dental hygiene, inflammation in mouth and pharynx Chronic bacterial parotitis Predisposition – ectasy of salivary ducts – congenital, postinfectious, obstructive, immunopatological Sialography Chronic fibroproductive sialoadenitis of submandibulary gland Known as Küttner tumor Periductal sclerosis Extirpation of submandibular gland and histological verification Sialolithiasis Stones composed of Ca salts often obstruct salivary glands, causing pain, swelling, and sometimes infection. Diagnosis is made clinically or with CT, ultrasound, or sialogram. Treatment involves stone expression with saliva stimulants, manual manipulation, a probe, or surgery. Eighty percent of stones originate in the submandibular glands and obstruct Wharton's duct. Most of the rest originate in the parotid glands and block Stensen's duct. Only about 1% originate in the sublingual glands. Multiple stones occur in about 25% of cases. Most salivary stones are composed of Ca phosphate with small amounts of Mg and carbonate. Patients with gout may have uric acid stones. Stone formation requires a nidus on which salts can precipitate plus salivary stasis. Stasis occurs in patients who are debilitated, dehydrated, have reduced food intake, or take anticholinergics. Persisting or recurrent stones predispose to infection of the involved gland (sialadenitis). Symptoms, Signs, and Diagnosis Stones cause glandular swelling and pain, particularly after eating, which stimulates saliva flow. Symptoms may subside after a few hours. Relief may coincide with a gush of saliva. Some stones cause intermittent or no symptoms. If a stone is lodged distally, it may be visible or palpable at the duct's outlet. If a stone is not apparent on examination, the patient can be given a sialagogue (eg, lemon juice, hard candy, or some other substance that triggers saliva flow). Reproduction of symptoms is almost always diagnostic of a stone. CT, ultrasound, and sialography are highly sensitive and are used if clinical diagnosis is equivocal. Contrast sialography may be performed through a catheter inserted into the duct and can differentiate between stone, stenosis, and tumor. This technique is occasionally therapeutic. Because 90% of submandibular calculi are radiopaque and 90% of parotid calculi are radiolucent, plain x-rays are not always accurate. MRI is not indicated. Treatment Analgesics, hydration, and massage can relieve symptoms. Antistaphylococcal antibiotics can be used to prevent acute sialadenitis if started early. Stones may pass spontaneously or when salivary flow is stimulated by sialagogues; patients are encouraged to suck a lemon wedge or sour candy every 2 to 3 h. Stones right at the duct orifice can sometimes be expressed manually by squeezing with the fingertips. Dilation of the duct with a small probe may facilitate expulsion. Surgical removal of stones succeeds if other methods fail. Stones at or near the orifice of the duct may be removed transorally, whereas those in the hilum of the gland often require complete excision of the salivary gland Enlargement of salivary glands Causes Unilateral Salivary enlargement Salivary Gland Tumor Bacterial Sialadenitis Chronic Sialadenitis Sialolithiasis Bilateral Salivary enlargement with hypofunction Viral Sialadenitis Sjogren's Syndrome Human Immunodeficiency Virus (HIV Infection or AIDS) Chronic granulomatous disease Sarcoidosis Tuberculosis Leprosy Sialadenosis (asymptomatic parotid enlargement) Eating disorder (Anorexia, Bulimia) Cirrhosis Chronic Pancreatitis Endocrine Disorder Acromegaly Diabetes Mellitus Gonadal hypofunction Case report – Bulimia nervosa (BN) case of a 22-year-old woman with BN who had bilateral parotid gland swelling, serum electrolyte alteration and no dental stigmata. Her principal concern was the associated cosmetic deformity. From the time of onset, the parotid gland swelling was persistent, painless and did not fluctuate in size. Palpation confirmed that the enlarged parotid glands were painless and normal in tone. We did not see any cervical lymphadenopathy. Intraorally, the mucosa was normally moist. All salivary ducts were patent with a clear and adequate salivary flow exiting from each parotid orifice when the gland was manually milked. The patient was caries-free, and no restorations were present. There were no signs of enamel erosion or periodontal abnormalities. The patient was excellent at following an oral hygiene regimen. Because she became increasingly alarmed about the parotid gland swellings, she sought medical care in June 2002, without admitting to the emetic problem. A computerized tomography, or CT, scan was performed, and she was told that the parotid glands were enlarged and denser for unknown reasons but that no pathology was present. She was not offered any medical treatment. Figure 1. A. Right parotid gland swelling (arrow). B. Left parotid gland swelling (arrow). Figure 2. Computerized tomography scan with contrast of moderately enlarged parotid glands (arrows). In December 2002, she visited another physician, who performed a serology evaluation. The patient’s serum potassium level was abnormally low (3.2 millimolar per liter; normal = 3.5–5.5 mmol/L). Hypokalemia was the only abnormality uncovered by the physician. At this point, the patient told her physician that she had BN. After potassium replacement therapy, she was referred to a psychiatrist and prescribed the antidepressant paroxetine hydrochloride. Bilateral—and occasionally unilateral—parotid gland swelling is not unusual in people with BN; the incidence of parotid gland swelling has been reported to occur in 10 to 15 percent of people with BN.The submandibular salivary gland is involved infrequently. The exact pathogenesis has not been determined. However, it generally is accepted that multiple emetic episodes cause an autonomic neuropathy. With sympathetic nerve impairment, individual acinar cells enlarge because of zymogen granule engorgement. One explanation is that the sympathetic nerve supply to the secreting acinar cell is concerned with the production and secretion of zymogen, the precursor of amylase. Because of sympathetic nerve dysfunction, there may be an increase in zymogen storage in the cell, owing to increased production, decreased secretion of the granules or both Benign tumors Benign Mixed Tumor (Pleomorphic adenoma) Most Common benign Salivary Gland tumor May affect major Salivary Glands May also affect minor Salivary Glands (esp. palate) Slow growing, nonulcerated painless tumor Occurs most commonly in women aged 30 to 60 years Monomorphic Adenoma Warthin's Tumor Malignant tumors Malignant Mucoepidermoid carcinoma (ages 20 to 50 years) Adenoid cystic carcinoma (age over 50 years) Locations: May affect any of Salivary Glands Parotid Gland Sublingual Gland Submandibular Gland Minor Salivary Glands Especially on posterolateral Hard Palate Buccal mucosa and lips may also be affected Diagnosis Slow growing, painless mass Palpation reveals enlargement CT or MRI scan diagnostic Management Surgical biopsy Prognosis Mucoepidermoid carcinoma Five year survival dependent on grading: 50-90% Adenoid cystic carcinoma Five year survival: 65% Twenty year survival: 15%