Turning on the Lytes in Dialysis
advertisement

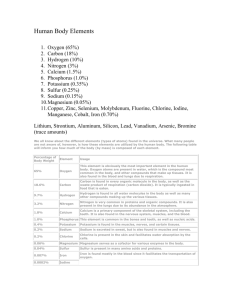
Turning on the Lytes in Dialysis DEBRA CASTNER RN, MSN, APRN, CNN JERSEY COAST NEPHROLOGY & HYPERTENSION BRICK, NJ Objectives List 2 electrolytes that are adjusted during dialysis Describe common signs and symptoms of electrolyte shifts in people on dialysis Explain how to reduce recovery time after dialysis So……………. WHAT ARE ELECTROLYTES? “Salts and minerals that can conduct electrical impulses in the body. Common human electrolytes are sodium chloride, potassium, calcium, and sodium bicarbonate. Electrolytes control the fluid balance of the body and are important in muscle contraction, energy generation, and almost every major biochemical reaction in the body.” http://medical-dictionary.thefreedictionary.com/electrolytes Why Electrolytes ? Electrolytes are controlled by the kidneys and hormonally Provide “electricity” within the body for transport of chemicals and fluids All higher forms of life need electrolytes to survive Ions and Charges Cations are positively charged ions ++++++ Anions are negatively charged ions - - - - - - How Do We Apply Them in Dialysis Hemodialysis Peritoneal Uses osmosis as main transport for fluid and solutes Glu c Glu c Glu c Glu c Glu c Glu c AQP1 Glu c peritoneal Glu c Glu c small Glu c large blood Slide courtesy of Anjali Bahatt Saxena, M.D., Santa Clara Valley Medical Center. What Lytes Do We Consider in Dialysis ? Potassium Sodium Calcium Magnesium Bicarbonate/Lactate Glucose Urea What Lytes Will We Focus On Today? Potassium Sodium Calcium Magnesium Bicarbonate/Lactate Glucose Urea Potassium Major intracellular cation in the body Associated with cardiac and muscle conduction, acid-base balance, and enzyme reactions Rapidly reducing potassium can effect the QT interval when dialyzing a patient against a zero or 1mEq potassium bath Low dialysate potassium concentration has been associated with cardiac dysrhythmias, especially in patients receiving digitalis preparations. Low post potassiums may cause muscle cramping and fatigue Higher pre potassium levels of 4.6-5.3 mEq/L have been associated with better survival Patients with predialysis potassium levels of less than 4.0 or greater than 5.6mEq/L were associated with increased mortality (Palmer, 2009) Potassium Homeostasis 2 Mechanisms: Excretion via kidney 90-95% over 6 to 12 hrs and intestine 5 – 10% Extracellular to Intracellular compartment shifts Hypokalemia Causes Potassium Removal During Dialysis Hypokalemia vs Potassium Deficiency/Depletion Potassium deficiency cause by negative potassium balance, intake is lower than excretion Hypokalemia is induced from potassium deficiency or from ECF to ICF shifts (ketoacidosis, catecholamine release during AMI, hyperthyroidism) Can have deficiency without hypokalemia ( low plasma measured potassium level) Primer on Kidney Diseases, 2009, Allon,M. Hypokalemia S & S Muscle weakness can lead to paralysis Ileus Urinary Retention Inability to concentrate urine Can lead to AV Block Hypokalemia Treatment Multiple small doses of potassium Oral is safer than IV, not to exceed 40mEq/dose IV dosing more likely to overcorrect, for levels <3.0meq IV infusion not greater than 10mmol/hr if not on cardiac monitor, check levels Q 2 to 3 hrs. Higher potassium dialysate 3 or 4mEq Diet instruction CORRECT Cause Primer on Kidney Diseases, 2009, Allon,M. Hyperkalemia Causes Pseudohypekalemia caused by in vitro release of potassium from blood cells ( hemolysis, severe leukocytosis or thrombocytosis, “fist clenching”) True hyperkalemia caused by high intake, low excretion, or shift from ECF to ICF ( ACE drugs in moderate CKD, potassium sparing diuretics, acidosis ) Can occur from prolonged fasting in dialysis patients due to increased insulin levels Primer on Kidney Diseases, 2009, Allon,M. Hyperkalemia S & S Bradycardia then Ventricular arrhythmias Muscle weakness as in hypokalemia Tingling of lips and fingers Intestinal cramping, diarrhea LIFE Threatening Risk Factors for Hyperkalemia Dialysis dependent Chronic Kidney Disease Stages 4 & 5 (CKD, eGFR < 30 ml/min/1.73m2) Nephrotoxic medications (e.g. renin-angiotensin agents, nonsteroidal anti-inflammatory drugs) Cardiac failure (e.g. renin-angiotensin agents) Diabetes mellitus (e.g. renin-angiotensin agents, diabetic ketoacidosis) Liver disease (e.g. spironolactone, hepato-renal failure) Adrenal insufficiency http://www.renal.org/guidelines/modules/treatment-of-acute-hyperkalaemia-in-adults#sthash.1D3sBbnO.dpuf Step Wise Approach Hyperkalemia Treatment Recipe for Emergency Treament 1. Calcium gluconate IV 10ml over 1 minute repeat in 3-5min. If no improvement in EKG to stabilize the heart does not decrease K+ 2. IV Insulin 10 units in 50 ml of 50% dextrose bolus first then infusion of 5% dextrose at 100cc/hr NEVER dextrose without insulin, potassium will decrease within 15 minutes 3. 20mg of Albuterol inhaled over 10 minutes, take 30 minutes to see effect 4. Sodium Bicarbonate in patients with residual kidney function only, takes 3 – 4hrs for potassium to decline 5. Then consider diuretics, kayexalate, hemodialysis Progression of EKG Changes in Hyperkalemia http://www.renal.org/guidelines/modules/treatment-of-acute-hyperkalaemia-in-adults#sthash.1D3sBbnO.dpuf EKG Changes Other Treatment Dialysate 1 or 2K Diet instruction Education for patient to understand risks Careful interviewing to establish cause Sodium Major cation of dialysate and the extracellular compartment of total body water Associated with cardiac, neuro, muscle conduction, acid-base and fluid balance Dialysate sodium concentration lower than plasma sodium concentration may induce intracellular movement of water and plasma volume depletion. Dialysate sodium concentration higher than plasma sodium concentration may induce extracellular movement of water, intracellular dehydration, and stimulation of thirst (Daugirdas, 2007) NKF-KDOQI Clinical Practice Guidelines for Adequacy,(2006) recommend that high dialysate sodium concentrations and sodium profiling be avoided. Hyponatremia Occurs in 15 – 20% of hospitalized patients Elderly are most susceptible Acute cases impact negatively on M&M Rapid correction can lead to severe neuro deficits High glucose levels will give false low sodium CORRECTION: 1.6 meq per each 100 mg/dL glucose above 100 add that number to serum sodium So if glucose is 300 and sodium was 130 it actually 133.2 Primer on Kidney Diseases, Verbalis, 2009 Hyponatremia Evaluation Hypernatremia Ability to excrete sodium loads can be impaired in kidney disease Defined as serum sodium over 146mEq/L Mostly seen in patients who have been restricted access to fluids or impaired thirst signals Sodium cannot freely cross into cells Always a “water problem” Hypernatremia = Hyperosmolar Associated with insulin resistance Primer on Kidney Diseases, Dennen & Linas, 2009 Contemporary Nephrology Nursing Principles and Practice, Molzahn, 2006 Hypernatemia Causes Hypovolemia/Euvolemic: GI, kidney, or skin, no access to water Hypervolemia: Intravenous solutions or tube feedings, hypoaldosterism Contemporary Nephrology Nursing Principles and Practice, Molzahn, 2006 Hypernatremia S&S Thirst Dry mucous membranes, N/V Flushed skin, fever, oliguria Irritability, lethargy, altered LOC, seizures OR No Signs Sodium Correction Cannot be done quickly Too fast a correction can lead to more issues than the disorder Abnormally high or low sodiums are associated with M&M in CKD patients (Kovesdy, 2012 Circulation) Low Sodium 0.5 – 2mEq/L per hour no more than 12mEq/l in frst 24 hours 18mEq/l over first 48hours of correction High Sodium 0.5mEq/l per hour, or a decrease of 10 – 12mEq/l in a 24 hour period Primer on Kidney Diseases, Verbalis,;, Dennen & Linas,, 2009 Sodium Variation: Is it the Right Approach? Calcium Cation associated with bone formation, neuromuscular transmission, enzyme and intracellular reactions Bound to plasma proteins (50%) 99% found in bone, 0.9% ICF, 0.1% ECF Kept in range by GI tract, skeleton, and kidneys Calcium level is a poor reflection of “true” body calcium 40% available as ionized, the active form Hypocalcemia Causes Decreased intake or poor absorption, malabsorption states Urinary losses Decreased availability: alkalosis, multi-transfusions, low albumin Medications: biphosphates, calcitonin, citrated blood, mithramycin Vitamin D deficiency, hypoparathyroidism Sepsis CORRECTION: Add 0.8mg/dL to the ionized calcium for every 1mg decrease in albumin below 4 So, if albumin is 3, a calcium of 7.8 would be 8.8 Hypocalcemia S&S Peri-oral numbness or tingling (parasthesias) Spasms of hands and feet Intestinal cramping, increased bowel sounds Tetany, seizure, laryngospasm Chvostek’s Sign (tap TMJ watch for grimace) Trousseau’s Sign ( BP cuff x 3 min. watch for hand spasm) Treatment of Hypocalcemia Hypercalcemia Evaluation/Causes Medications: Vitamin D or A lithium, thiazides Hypercalcemia S&S Severity depends on degree and rate of increase GI: N/V, constipation, abdominal pain Neuro: altered mentation, fatigue, muscle weakness Renal: sodium wasting due to increased urine output Most Common Causes (80%) are HYPERPARATHRYOIDISM OR MALIGNANCY Hypercalcemia Treatment Remove cause Fluids & diuretics IV Biphosphonates (Aredia, Reclast) Calcitonin Glucocorticoids Cinacalcet EKG Changes Magnesium An abundant intracellular cation, 60- 64% is stored in bone Bound to ATP, ADP, mitochondria, proteins, nucleic acids and doesn’t move freely to ECF Absorbed through the small intestine 95% excreted via kidney Hypomagnesemia S & S/Causes How It Happens Medications: amphotericin B, aminoglycosides, cisplastin, CSA, Prograf, PPI’s, diuretics. Associated with low K/CA GI Losses, malnutrition, alcoholism, gastric bypass, pancreatitis, ketoacidosis. Hypomagnesemia treatment EKG Changes Hypermagnesemia S & S Hypermagnesemia Treatment Remove cause magnesium containing medications Laxatives Antacids Herbal Remedies Dialysis IV calcium can temporarily shift Mg Bicarbonate/Lactate/Acetate Polyatomic anion A buffer that helps maintains pH of the ECF Normal pH is 7.35-7.45 Kidney produces and regulates it in the proximal tubule by excretion or reabsorption. Also produced in the pancreas. 70-75% of CO2 in the body is converted into carbonic acid (H2CO3), which is turned into bicarbonate We add it to dialysate based on CO2 levels of patient Goal is pre dialysis CO2 of 22-24 Use caution with bicarbonate dialysate >35mEq (Handbook of Dialysis 2007) Metabolic Acidosis Acids are extracted from dietary carbohydrates and fats which yields carbon dioxide and water The lower the pH the worse the acidosis In renal failure patients become acidotic because hydrogen ions cannot be excreted and bicarbonate production / reabsorption is impaired High pre CO2 levels can indicate inadequate dialysis Other causes of acidosis: sepsis, starvation, diarrhea, overdoses of salicylates, ethylene glycol, or methanol Metabolic Acidosis S & S Metabolic Alkalosis Rare in renal disease Alkalosis is more dangerous to renal patients than acidosis, can lead to soft tissue calcification, nausea, lethargy and H/A Mild alkalosis can lead to hypoventilation (Handbook of Dialysis, 2007) Relative Risks Associated with K and Bicarbonate levels – FMC Study 2011 http://graphic8.nytimes.com/packages/pdf/business/fresenius-memo.pdf Metabolic Alkalosis Treatment of Metabolic Acid – Base Disorders Identify cause Adjust dialysate May need to add oral medication Trend out CO2 levels every month and call for adjustments Correct severe imbalances gradually Glucose In dialysate not used to adjust serum glucose but to avoid hypoglycemia Urea A marker solute for clearance of toxins Not of itself toxic Serum levels depend on rate of removal and generation rate Low levels associated with malnutrition Post dialysis rebound for urea is highest for smaller patients Rapid removal associated with Disequilibrium Syndrome (urea >125) (Daugirdas, 2007) Fluid Removal Changes occur in microcirculation before you see hypotension or other S&S Dialysis in general is an inflammatory procedure with release of bradykinins and nitric oxide Ultrafiltration Rates & Mortality High UF rates are associated with higher mortality and hospitalization rates UF Rates of 10-13ml/kg/hr have statistical significance in pts with HF N = 1846 Hemodialysis Study: 7 year trial All pts had risk increase (all-cause and CV) when compared from lowest group to highest group Flythe et al, 2011 Recovery Time How Long Does It Take You To Recover From A Dialysis Session ? Recovery Time & Quality of Life N = 6,040 DOPPS data 32% less than 2hrs 41% 2 – 6hrs 17% 7 – 12hrs 10% Longer than 12hrs There is a correlation of improved QOL with lower recovery time. Longer recovery time associated with admissions, mortality and poor QOL Rayner et al, 2013, AJKD published online February 2013 Adverse Effects of Intradialytic Hypotension Life-threatening consequences Impaired tissue perfusion can lead to inaccurate adequacy Contributes to loss of residual renal function Can cause cerebral ischemia Core Curriculum for Nephrology Nursing, 5th ed. 2008 Cerebral Ischemia Cerebral blood flow is reduced during dialysis It gets lower with increased UF Cerebral compensation is less effective with advanced age, hypertension, inflammation, vascular injury Rapid increase in bicarbonate can reduce CBF and increase cerebral edema Neuroimaging confirms brain changes in renal patients occurring within months of starting dialysis Davenport, 2014 There is a link with higher pre dialysis BP and survival Robinson et al 2012 130-159 Cardiac Stunning ‘delayed recovery of regional myocardial contractile function after reperfusion despite the absence of irreversible damage and despite restoration of normal flow’. Braunwald and Kloner , 1982 HD-induced myocardial stunning is common and could be the predisposing element leading to the increased prevalence of heart failure and increased mortality in CKD patients with ESRD. Breidthard, 2011 Mechanism of Cardiac Stunning Loss of high-energy phosphates, impaired microvascular perfusion, impaired sympathetic neural responses, reactive oxygen species, leukocyte activation, and disturbances in calcium homeostasis At the cellular level reactive oxygen species, thrombosis, ischemia/reperfusion injury, microvascular dysfunction, and channelopathies may contribute to myocardial stunning Two main metabolic pathways leading to myocardial stunning include calcium overload and reactive oxygen species (ROS) generation. Cardiac stunning = Sudden Death Myocardial Stunning with Hemodialysis: Clinical Challenges of the Cardiorenal Patient, Zuidema et al, 2012 Cardiorenal Med. May 2012; 2(2): 125–133. Published online Mar 30, 2012. doi: 10.1159/000337476 ANNA Scope and Standards for Care: Hemodialysis Treatment and Equipment Related Complications The patient will: Receive appropriate and safe HD treatment Be free of treatment/equipment-induced complications……….. Gomez, N. 2011 Practice Pearls Always LOOK at the patient Scan your environment Communicate Compare historical measures when “numbers” or “readings” don’t fit the patient Your patient chart is your friend Always “error” on the side of patient safety Case Study Joe is an active HD patient enjoying family parties and frequent travel. He reports feeling “lousy” after dialysis lately and it is taking a whole day to recover. He is on: 1K, 138mEq, bicarb 38, sodium 142, glucose 100, Mg 0.8, Dialysate His labs are: K 5.5, CO2 27, sodium 137, Mg 2.5 What could be causing issues for this patient? What would you review to help plan a strategy? So What Have We Learned? Fast is not always better Using lab results and patient trending can help make dialysis more comfortable for our patients Recovery Time is linked to QOL Questions, Comments?