System 2
advertisement

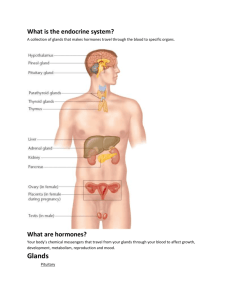
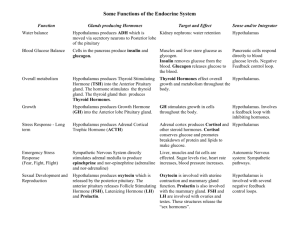
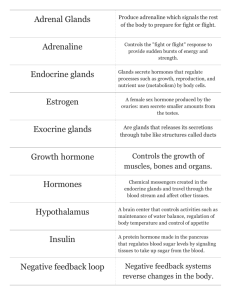
The Human Endocrine System ENDOCRINE SYSTEM Endocrine glands: glands that lack ducts (ductless), secrete hormones directly into the blood that affect target cells. Exocrine glands are the ones that their secretions go via ducts to the lumen of other organs (like salivary glands leading to oral cavity ) or outside the body (sweat glands). Hormones are biologically active molecules, that affect metabolism of their target organs, help regulate total body metabolism, growth, reprodution. Neurohormones are secreted into blood by specialized neurons. Why hormones affect only the target organ? Hormones are regulatory chemicals that work at a distance between organs traveling through the bloodstream from the gland to the target cell. The hormone binds only to cells having its receptor. Signaling can also be paracrine or autocrine. Neural and Endocrine Regulation • Both use chemicals to communicate • Some are used both as hormone and neurotransmitters (NTs). • Differences: • NTs diffuse across a synaptic cleft • Hormones are transported in blood. They have more diverse effects on their targets. • Physiological regulation: • Targets for both NTs and hormones must have specific receptor proteins • Binding must cause a specific sequence of changes in the target cells • Must be a mechanism to turn off the action of the regulator. The endocrine system rely on negative feedback mechanisms. Hormones classes based on their chemistry • Amines: are hormones derived from 2 amino acids (tryptophan and tyrosine) they include hormones secreted from: 1- Thyroid gland : T3 and T4. 2- Pineal gland : melatonine. 3- Adrenal medulla: epinephrine and norepinephrine. • polypeptides: less than 100 aminoacids e.g ADH • Proteins: more than 100 aminoacids e.g Growth hormones. • Glycoproteins: consist of polypeptides with one or more carbohydrate groups e.g: follicle stimulating hormone (FSH), Luteinizing hormone (LH) and thyroid stimulating hormone (TST). • Steroids are lipids derived from cholesterol e.g progesterone, testesterone, estradiol, cortisol, aldosterone. Water-soluble (hydrophilic) Lipid-soluble (hydrophobic) Polypeptides Steroids 0.8 nm Insulin Cortisol Amines Epinephrine Thyroxine Polarity of the hormones • Polar hormones – water-soluble. – Polypeptides, glycoproteins hormones – Exception: melatonin derived from nonpolar amino acid tryptophan can pass through the plasma membrane • Nonpolar or lipophilic hormones – insoluble in water and can pass through plasma membrane of their target cells – Steroid hormones – Thyroid hormones: composed of the amino acid tyrosine with iodine atoms • Steroid and thyroid hormones are active when taken orally e.g contraceptive pills. Melatonine is also taken orally. • Polypeptide and protein hormones are not given orally e.g insulin injections. Prohormones and Prehormones • Prohormones – precursors molecules – e.g. proinsulin is cut and spliced together to form insulin • Prehormones – precursors of hormones – e.g. preinsulin • Some hormones are inactive until activated by target cells • The term prehormone designates the molecules secreted by endocrine glands but are inactive until they are changed into active form in their target cell • e.g. thyroxine (T4) is inactive until converted to T3 in target cells • Prehormone = T4 (inactive) T3 (active) • Prehormone = Vit D3 (2 hydroxylations) 1,25 dihydroxyvit D3 (active). Hormone Interactions • Target tissue usually responds to a number of different hormones 1. Synergistic – two hormones work together – Produce a larger effect together than the added effect – e.g. norepinephrine and epinephrine on heart rate -FSH and testesterone each is important in specific step in spermatogenesis; complimentary action. -Estrogen, cortisol, prolactin, have complimentary effect on mammary glands to produce and secret milk. Hormone Interactions 2. Permissive effect – one hormone enhances the responsiveness of a target organ to a second hormone – e.g. estradiol induces formation of receptors for progesterone. – Low calcium levels in blood stimulates the release of parathyroid hormone (PTH) which has Permissive effect on Vit. D. PTH induces Vit D hydroxylations in liver and kidney 1,25 dihydroxy vit D increases Ca2+ reabsorbtion by intestine thereby rises Ca2+ level in the blood. 3. Antagonistic – action of one inhibits the effect of the other – e.g. lactation during pregnancy (high prolactin) inhibited by estrogen (inhibits secretion and action of prolactin). – pancreatic islets secrete Insulin and Glucagon which has Antagonistic effects. Insulin Body cells take up more glucose. Blood glucose level declines. Beta cells of pancreas release insulin into the blood. Liver takes up glucose and stores it as glycogen. STIMULUS: Blood glucose level rises (for instance, after eating a carbohydrate-rich meal). Homeostasis: Blood glucose level (70–110 mg/m100mL) STIMULUS: Blood glucose level falls (for instance, after skipping a meal). Blood glucose level rises. Liver breaks down glycogen and releases glucose into the blood. Alpha cells of pancreas release glucagon into the blood. Glucagon Hormone Levels and Tissue Responses • Half-life – time required for plasma concentration of a hormone to be reduced by half – Ranges from minutes to hours for most (days for thyroid hormones) • Normal tissue responses produced only when hormones are within normal physiological range • High (pharmacological) doses – cause side effects – Probably by binding to receptors of different but closely related hormones Hormone Levels and Tissue Responses • Priming effect (upregulation) – a hormone induces more of its own receptors in target cells – Results in greater response in target cell – e.g. GnRH secreted by the hypothalamus increases sensitivity of anterior pituitary cells to further stimulation (upregulation of receptors) • Desensitization (downregulation) – occurs after long exposure to high levels of polypeptide hormone (e.g. adipose cells to insulin) – Subsequent exposure to this hormone produces a lesser response (downregulation of receptors) – Most peptide hormones have pulsatile secretion (spurts) which prevents downregulation Mechanisms of Hormone Action • Target cell receptors show – specificity, high affinity (strength of binding), and low capacity (saturation) for a hormone • Lipophilic hormones – have receptors in target's cytoplasm and/or nucleus – diffuse through plasma membrane – target is the nucleus where they affect transcription • Called genomic action and takes at least 30 minutes • Receptors for hydrophilic hormones – are on surface of target cell – These act through 2nd messengers; effects are quick – Some steroids also act on cell surface receptors • Called nongenomic action Mechanism of Steroid Hormones • Lipid hormones travel in blood attached to carrier proteins – dissociate from carriers – pass through plasma membrane to target cell • Bind to receptors in the cytoplasm – nuclear hormone receptor • Hormone-receptor complex translocates to nucleus binds DNA • Genetic transcription and translation produce proteins Nuclear Hormone Receptors • Serve as transcription factors when bound to hormone ligands to activate transcription • “Superfamily" – steroid family and thyroid hormone family – Also Vitamin D and retinoic acid Hormones That Use Second Messengers • Water soluble hormones use cell surface receptors • Actions are mediated by 2nd messengers – Hormone is the extracellular signal – 2nd messenger carries signal from receptor to inside of cell • Adenylate Cyclase-cAMP 2nd Messenger System • cAMP mediates effects of many polypeptide and glycoprotein hormones • Hormone binds to receptor causing dissociation of a G-protein subunit that binds to and activates adenylate cyclase • Inhibitory subunit dissociates, activating protein kinase • Phosphorylates enzymes that produce hormone’s effects • cAMP gets inactivated by phosphodiesteras Adenylate Cyclase-cAMP • Binding converts ATP into cAMP – attaches to inhibitory subunit of protein kinase Table 11.4 Phospholipase-C-Ca2+ 2nd Messenger System • Serves as 2nd messenger system for some hormones • Hormone binds to surface receptor activates G-protein activates phospholipase C Phospholipase-C-Ca2+ • Phospholipase C splits a membrane phospholipid into 2nd messengers IP3 and DAG • IP3 diffuses through cytoplasm to ER causing Ca2+ channels to open • Ca2+ diffuses into cytoplasm and binds to and activates calmodulin • Ca2+-Calmodulin activates protein kinases – phosphorylate enzymes that produce hormone's effects Endocrine Glands Many endocrine glands are organs whose primary function is hormone secretion. Some are mixed glands: e.g the pancreas is an endocrine and exocrine gland. Steroids are secreted by only the adrenal cortex and the gonads (testis & ovary). Pituitary Gland • • Located beneath hypothalamus at base of forebrain Also called hypophysis Pituitary Gland • Structurally & functionally divided into anterior and posterior lobes • Hangs below hypothalamus by infundibulum • Anterior produces own hormones – Controlled by hypothalamus • Posterior stores and releases hormones made in hypothalamus Posterior Pituitary Gland • Stores and releases vasopressin also called antidiuretic hormone (AVP or ADH) and oxytocin – Hormones are made in the hypothalamus • Supraoptic nuclei of hypothalamus produce ADH • Paraventricular nuclei produce oxytocin • Both are transported along hypothalamo-hypophyseal tract to posterior pituitary Hypothalamic Control of Posterior Pituitary Neurons in the hypothalamus called neurosecretory cells produce Antidiuretic hormone (ADH) that promotes reabsorption of water from the collecting ducts in the kidneys. ADH is released upon stimulation of osmoreceptors in the hypothalamus in response to rise in blood osmolality. An increased osmotic pressure increases the frequency of action potentials in the neurons that produce ADH this causes the opening of voltage-gated Ca+ channels which causes the release of ADH by exocytosis. ADH secretion is inhibited by sensory input from stretch receptors in the left atrium which are stimulated by a rise in blood volume. As the blood becomes dilute, ADH is no longer released; this is a case of negative feedback. Oxytocin Oxytocin stimulates uterine muscle contraction during parturition It also stimulates the release of milk from mammary glands. The mechanical stimulus of suckling acts via sensory nerve impulses to the hypothalamus to stimulate the reflex secretion of oxytocin. The Oxytocin causes contraction of myoepithelial cells in mammary glands and milk begins to flow. This mechanism is called milk letdown or milk ejection Anterior Pituitary Gland • Secretes 6 trophic hormones • Maintain size of target organs: 1. High blood levels cause target to hypertrophy 2. Low levels cause atrophy Anterior Pituitary • Releasing and inhibiting hormones from hypothalamus – released from axon endings into capillary bed in median eminence – Carried by hypothalamohypophyseal portal system to another capillary bed – Diffuse into and regulate secretion of anterior pituitary hormones Anterior Pituitary • 1. Stimulation by the hypothalamus controls the release of anterior pituitary hormones through a portal system consisting of two capillary systems connected by a vein. • 2. The hypothalamus produces hypothalamic-releasing and hypothalamic-inhibiting hormones which pass to the anterior pituitary by this portal system. E.G • Thyroid-releasing hormones (TRH) released from the hypothalamus act on cells in the anterior pituitary to stimulate the production and secretion of a specific hormone TSH. • Prolactin – inhibiting hormone ( PIH) it inhibits secretion of prolactin hormone by anterior pituitary gland. Anterior Pituitary 1. Growth hormone (GH) promotes growth, protein synthesis, and movement of amino acids into cells 2. Thyroid stimulating hormone (TSH) stimulates thyroid to produce and secrete T4 and T3 3. Adrenocorticotrophic hormone (ACTH) stimulates adrenal cortex to secrete cortisol, aldosterone 4. Follicle stimulating hormone (FSH) stimulates growth of ovarian follicles and sperm production 5. Luteinizing hormone (LH) causes ovulation and secretion of testosterone in testes 6. Prolactin (PRL) stimulates milk production by mammary glands The anterior pituitary produces six different hormones. a. Four of these anterior pituitary hormones affect other glands. • 1) The thyroid-stimulating hormone (TSH) stimulates the thyroid gland to produce and secrete thyroxin (T4). • 2) Adrenocorticotropic hormone (ACTH) stimulates the adrenal cortex to release cortisol. • 3) Gonadotropic hormones (follicle-stimulating hormone [FSH] and luteinizing hormone • [LH]) act on the gonads (ovaries and testes) to secrete sex hormones. • b. The other two hormones do not affect other glands. • 1) Prolactin (PRL) causes the mammary glands to produce milk. • b) It also plays a role in carbohydrate and fat metabolism. • 2) Growth hormone (GH or somatotropic hormone) • a) GH promotes skeletal and muscular growth. • b) GH acts to stimulate the transport of amino acids into cells and to increase the activity of ribosomes. The hypothalamic-pituitary-gonad axis • The hypothalamic-pituitarygonad axis (control system) • Involves negative feedback by target gland hormones Higher Brain Function and Anterior Pituitary Secretion Hypothalamus receives input from higher brain centers – can affect anterior pituitary secretion – e.g. emotional states and psychological stress can affect circadian rhythms, menstrual cycle, and adrenal hormones Adrenal Glands • Suprarenal glands – sit on top of kidneys • Each consists of outer cortex and inner medulla – arise differently during development Adrenal Glands • Medulla synthesizes and secretes 80% epinephrine and 20% norepinephrine – Controlled by sympathetic division of autonomic nervous system • Cortex is controlled by ACTH and secretes: – Cortisol which inhibits glucose utilization and stimulates gluconeogenesis (generation of glucose from noncarbohydrate carbon substrates hence helps elevate blood glucose levels) – Aldosterone which stimulate kidneys to reabsorb Na+ and secrete K+ regulate the levels of minerals in the blood – And some supplementary sex steroids (the adrenal cortex also secretes a small amount of both male and female sex hormones in both sexes). Adrenal Cortex Glucocorticoids Cortisol promotes the breakdown of muscle protein into amino acids taken up by the liver from the blood. Cortisol breaks down fatty acids rather than carbohydrates; cortisol therefore raises blood glucose levels. Cortisol counteracts the inflammatory response Mineralocorticoids The primary target organ of Aldosterone is the kidney where it promotes the reabsorption of Na+ and the excretion of K +. Atrial natriuretic hormone (ANH) causes the excretion of sodium. 1) When the atria of the heart are stretched due to increased blood volume, cardiac cells release ANH. 2) ANH inhibits the secretion of aldosterone from the adrenal cortex. 3) When sodium is excreted, so is water; the blood volume and pressure then return to normal. Regulation of Blood Pressure and Volume Adrenal Medulla • Hormonal effects of epinephrine last 10X longer than norepinephrine • Innervated by preganglionic Sympathetic fibers • Activated during "fight or flight" response – – – – Increased respiratory rate Increased heart rate and cardiac output General vasoconstriction which increases venous return Glycogenolysis and lipolysis Stress and the Adrenal Gland • Stress induces a nonspecific response: general adaptation syndrome (GAS) • Causes release of ACTH and cortisol CRH : corticotropin releasing hormone Stress and the Adrenal Gland • Chronic stress can induce high levels of cortisol that cause a number of negative effects: – – – – atrophy of hippocampus (involved in memory) reduced sensitivity of tissues to insulin (insulin resistance) inhibition of vagus nerve activity suppression of growth hormone, thyroid hormone, and gonadotropins • Exogenous glucocorticoids used to supress the immune response and inhibit inflammation such as in asthma & rheumatoid arthritis. They have side effects like hyperglycemia and osteoporosis. (b) Long-term stress response and the adrenal cortex Stress Hypothalamus Releasing hormone Anterior pituitary Blood vessel ACTH Adrenal gland Adrenal cortex secretes mineralocorticoids and glucocorticoids. Kidney Effects of mineralocorticoids: Effects of glucocorticoids: • Retention of sodium ions and water by kidneys • Proteins and fats broken down and converted to glucose, leading to increased blood glucose • Increased blood volume and blood pressure • Partial suppression of immune system (a) Short-term stress response and the adrenal medulla Stress Nerve Spinal cord (cross section) signals Hypothalamus Nerve cell Adrenal medulla secretes epinephrine and norepinephrine. Effects of epinephrine and norepinephrine: • Glycogen broken down to glucose; increased blood glucose • Increased blood pressure • Increased breathing rate • Increased metabolic rate • Change in blood flow patterns, leading to increased alertness and decreased digestive, excretory, and reproductive system activity Nerve cell Adrenal gland Kidney Thyroid Gland • Located just below the larynx • Secretes T4 and T3 which set basal metabolic rate (increase the metabolic rate; there is no one target organ—all organs respond) – needed for growth, development – Secrete also calcitonin that lowers the calcium level in the blood and increases deposits of calcium in the bone • Consists of microscopic thyroid follicles – Outer layer follicle cells synthesize T4 – Interior filled with colloid, a protein-rich fluid A scan of the thyroid 24 hrs. after intake of radioactive iodine Figure 11.22 Parathyroid Glands • 4 glands embedded in lateral lobes of posterior side of thyroid gland • Secrete Parathyroid hormone (PTH) – Most important hormone for control of blood Ca2+ levels 11-62 Parathyroid Hormone • • • • • Release is stimulated by decreased blood Ca2+ Acts on bones, kidney, and intestines to increase blood Ca2+ levels Under the influence of PTH, the calcium level in blood increases and the phosphate level decreases. PTH stimulates the retention of Ca2+ (& excretion of phosphate) by the kidney. demineralization of bone by promoting the activity of osteoclasts. Vit D promotes the intestinal absorption of Ca2+. Regulation of Blood Calcium Level Increases Ca2 uptake in intestines Active vitamin D Stimulates Ca2 uptake in kidneys PTH Stimulates Ca2 release from bones Parathyroid gland (behind thyroid) STIMULUS: Falling blood Ca2 level Blood Ca2 level rises. Homeostasis: Blood Ca2 level (about 10 mg/100 mL) Islets of Langerhans • Scattered clusters of endocrine cells in pancreas • Contain alpha and beta cells • Diabetes mellitus is a fairly common disease Islets of Langerhans – Alpha Cells • Alpha cells secrete glucagon in response to low blood glucose – Stimulates glycogenolysis and lipolysis – Increases blood glucose Islets of Langerhans – Beta Cells • Beta cells secrete insulin in response to high blood glucose – Promotes entry of glucose into cells – And conversion of glucose into glycogen and fat – Decreases blood glucose level 11-67 Regulation of Blood Glucose Level Pineal Gland • Located in basal forebrain near thalamus • Secretes melatonin in response to activity of suprachiasmatic nucleus (SCN) of hypothalamus Pineal Gland • SCN – primary timing center for circadian rhythms – Reset by daily light/dark changes • Melatonin – is involved in sleep/awake cycle – Secreted at night and inhibited by light – Implicated in jet-lag The pineal gland may also be involved in human sexual development; children in whom a brain tumor has destroyed the pineal gland experience puberty earlier. Thymus Gland 1. The thymus gland is a lobular gland that lies just beneath the sternum in the upper thoracic cavity. 2. It reaches its largest size and is most active during childhood; with age, it shrinks and becomes fatty. 3. Some lymphocytes that originate in the bone marrow pass through the thymus and change into T lymphocytes. 4. The thymus produces thymosins, which aid in the differentiation of T cells and may stimulate immune cells. Sex Hormones The ovaries, located in the pelvic cavity, produce the female sex hormones estrogens and progesterone. a. Estrogens secreted at puberty stimulate the maturation of ovaries and other sexual organs. b. Estrogen is necessary for oocyte development. c. It is responsible for the development of female secondary sex characteristics: a layer of fat beneath the skin, a larger pelvic girdle, etc. d. Estrogen and progesterone are required for breast development and the regulation of the uterine cycle. • Testosterone normally is the reason men have larger muscles than women. • It is responsible for the development of male secondary sex characteristics. • Anabolic Steroids: are synthetic drugs very similar in structure and action to male hormone testosterone. The Effects of Anabolic Steroid Use Paracrine & Autocrine regulation Local regulators such as prostaglandins (PG) are produced by certain cells and act on neighboring cells. PG functions • They cause the contraction of uterine muscle • They mediate the effects of pyrogens (chemicals believed to affect the temperature regulatory center of the brain). • Certain prostaglandins reduce gastric secretions, others lower blood pressure. d. Aspirin reduces temperature and controls pain because of its effect on prostaglandins (inhibits cyclooxygenase, the enzyme that synthesizes PGs). Endocrine gland Major hormone Target tissue Effect Adipose tissue leptin Hypothalamus Suppresses appetite heart Atrial natriuretic hormone kidneys Promotes secretion of Na+ in urine Small intestine Secretin, CKK Stomach, liver & pancreas Inhibits gastric motility, stimulates secretion of bile & pancreatic juice kidneys Erythropoietin Bone marrow Stimulates RBC production skin 1,25 dihydroxyvit D3 Small intestine Stimulates absorption of Ca 2+ stomach gastrin stomach Stimulates acid secretion Thymus thymopoietin Lymph nodes Stimulates WBC production ( Lymphocyte )