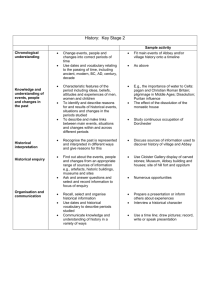
APC Update for CY2009
advertisement

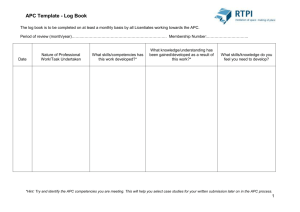
APCs: Issues and Answers Sponsored By: APCNow Web Site www.APCNow.com Presented By: Duane C. Abbey, Ph.D., CFP Abbey & Abbey, Consultants, Inc. Duane@aaciweb.com http://www.aaciweb.com http://www.APCNow.com http://www.HIPAAMaster.com Version 10.0 - Generic Notes © 1994-2009, Abbey & Abbey, Consultants, Inc. CPT® Codes – © 2008-2009 AMA © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 1 Presentation Faculty Duane C. Abbey, Ph.D., CFP – Dr. Abbey is a healthcare consultant and educator with over 20 years of experience. He has worked with hospitals, clinics, physicians in various specialties, home health agencies and other health care providers. His primary work is with optimizing reimbursement under various Prospective Payment Systems. He also works extensively with various compliance issues and performs chargemaster reviews along with coding and billing audits. Dr. Abbey is the President of Abbey & Abbey, Consultants, Inc. and his firm provides a wide range of consulting services across the country including chargemaster reviews, APC compliance reviews, in-service training, physician training, and coding and billing reviews. Dr. Abbey is the author of nine books on health care including: •“Non-Physician Providers: Guide to Coding, Billing, and Reimbursement” •“Emergency Department: Coding, Billing and Reimbursement”, •“Chargemasters: Strategies to Ensure Accurate Reimbursement and Compliance”, •“Chargemaster Coordinators Handbook”, and •“Compliance for Coding, Billing and Reimbursement”. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 2 Disclaimer This workshop and other material provided are designed to provide accurate and authoritative information. The authors, presenters and sponsors have made every reasonable effort to ensure the accuracy of the information provided in this workshop material. However, all appropriate sources should be verified for the correct ICD-9-CM Codes, ICD-10-CM Diagnosis Codes, ICD-10-PCS Procedure Codes, CPT/HCPCS Codes and Revenue Center Codes. The user is ultimately responsible for correct coding and billing. The author and presenters are not liable and make no guarantee or warranty; either expressed or implied, that the information compiled or presented is errorfree. All users need to verify information with the Fiscal Intermediary, Carriers, other third party payers, and the various directives and memorandums issued by CMS, DOJ, OIG and associated state and federal governmental agencies. The user assumes all risk and liability with the use and/or misuse of this information. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 3 APCs: Issues & Answers Objectives To review the changes for the Medicare APC payment system for CY2009 with attention to anticipated changes based on trends. To review various APC weight changes and updates. To understand key issues within APCs and the final changes. To discuss increased packaging and bundling within APCs. To appreciate the need for hospitals to assess changes and make suggestions and comments to CMS. To review the various data files that CMS provides with APCs. To appreciate technical component E/M coding for the ED and providerbased clinics. To discuss the different CMS changes including supplies, drugs and devices. To briefly review changes for ASCs relative to APCs and other APC related issues. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 4 APCs: Issues & Answers Acronyms/Terminology APCs – Ambulatory Payment Classifications APGs – Ambulatory Patient Groups ASC – Ambulatory Surgical Center CAH – Critical Access Hospital CCRs – Cost-to-Charge Ratios CPT – Current Procedural Terminology E/M – Evaluation and Management FFS – Fee-for-Service HCPCS – Healthcare Common Procedure Coding System ICD-9-CM – International Classification of Diseases, Ninth Edition, Clinical MAC – Medicare Administrative Contractor MedPAC – Medicare Advisory Commission MPFS – Medicare Physician Fee Schedule NCCI – National Correct Coding Initiative © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 5 APCs: Issues & Answers Acronyms/Terminology NCD/LCD – National/Local Coverage Decision NTIOL –New Technology Intraocular Lens OCE – Outpatient Code Editor OPD – [Hospital] Outpatient Department OPPS – [Hospital] Outpatient Prospective Payment System PHP – Partial Hospitalization Program PM – Program Memorandum PPS – Prospective Payment System QIO – Quality Improvement Organization SI – Status Indicator ASC – Ambulatory Surgical Center RBRVS – Resource Based Relative Value System MPFS – Medicare Physician Fee Schedule Developed through RBRVS © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 6 APCs: Issues & Answers General Comments APCs are becoming increasingly complex and more difficult to understand. Enormous Federal Register entries are now the norm. APCs represent a payment system that is out of control. Significantly increased bundling through packaging is being added. APCs appear to be moving more toward APGs. There are wide variations in payments from year to year. Significant compliance concerns exist within the overall APC payment system. In some cases these compliance concerns result because of lack of explicit guidance from CMS. At some point the RAC auditors will become more involved in APCs. APCs and the underlying coding systems (i.e., CPT and HCPCS) generate constant change and the need to update. Tracking and verifying that correct payment is received is difficult. It is critical to track adjudication and overall payment. Major issues with hospital charges, CCRs and the cost report are present. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 7 APCs: Issues & Answers APC Background Information APC Fundamentals Encounter Driven System • Some Exceptions – Example: Two separate blood transfusions on the same day or two imaging services at different times on the same day. CPT/HCPCS Code Driven • If the service is not coded with a CPT or HCPCS (and/or proper modifiers), then there will be absolutely no payment! APC Grouper Multiple APCs from Given Claim Inpatient-Only Procedures • Surgery, if performed outpatient, will not be paid at all! (Patient Liability?) • How is this list determined? Covered, Non-Covered and Payment System Interfaces • Example: Self-Administrable Drugs Pass-Through Payments – Directly Based on Charges Made – Covert Charges to Costs How? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 8 APCs: Issues & Answers APC Background Information APC Weight, and Thus Payment, Determination Hospital Charges Converted to Costs • How is this done? • Do we charge for everything? • Do we charge correctly for everything? Statistical Process Using the Costs • Geometric Mean • Mean Cost for Given APC/Mean Cost for All APCs = the APC Weight Variation of Costs Within a Given APC Category • 2 Times Rule – If highest cost is more than twice the lowest cost then violation. • 2 Times Rule Exception List Examples: o APC=0080 Diagnostic Cardiac Catheterization o APC=0604 Level 1 Hospital Clinic Visits © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 9 APCs: Issues & Answers APC Background Information Use of Claims to Statistically Develop the APC Weights Because outpatient encounters often involve multiple services, the APC grouping process often (if not a majority of the time) generates multiple APCs. CMS can use only pure claims, that is, claims that group to a single APC. These are called ‘singleton’ claims. CMS is trying very hard to get around this situation because most of the claims filed by hospitals never get considered when the actual APC weights are determined. • Small Example: CPT=86891 – Intra- or Post-Operative Blood Salvage A device is used to save blood, reprocess the blood and generally re-infuse. Is it possible to have ONLY 86891 on a claim? What kind of payment do we have for 86891? What are the costs involved? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 10 APCs: Issues & Answers APC Background Information APC Cost Outliers Complicated Two-Tiered Formula Cost Threshold to $1,800.00 Based on Excessive Costs - How are costs determined? Nationally, does CMS make full outlier payments? Provider-Based Rule (42 CFR §413.65) Provider-Based Clinics Provider-Based Clinical Services Potentially, two claim forms filed – CMS-1450 (UB-04) for technical component and CMS-1500 (1500) for professional component. Reduction in payment for professional component • Site-of-Service Differential in RBRVS (MPFS) • Place-of-Service (POS) driven on CMS-1500 Series of Criteria to Meet If to be Provider-Based • On-Campus versus Off-Campus • See Physician Supervision Developments Important © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 11 APCs: Issues & Answers APC Background Information ASCs – Ambulatory Surgical Centers In CY2008 Started a Hybrid of APCs and RBRVS FR entries for APCs will now also be for ASCs ASC Surgery List • Regular ASC Surgeries • Office-Based Surgeries New Additions • Conditions for Coverage (CfCs) New Acronym • Additions and Deletions to Lists Payment Formula • ASC Surgery 65% of APC • Office-Based Surgeries – Lesser of: 65% of APC or Non-Facility PE RVU from MPFS • Physician Paid Facility MPFS (As With Hospitals) Separate Payment for Certain Ancillary Services Did all the features of APCs translate over? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 12 APCs: Issues & Answers CPT/HCPCS Changes For CY2009 As usual there are hundreds of changes for both CPT and HCPCS. Also, there was an unusually large number of changes for ICD-9-CM. Injections/Infusions • These have all been renumbered!! • Coding guidance has, in theory, been revised. Need to carefully compare 2008 guidance versus 2009 guidance. Laparoscopy • Six New Codes – Hernias Radionuclide Brachytherapy ESRD – Twenty New Codes – Applicability? Cardiovascular Device Monitoring – • Twenty-One New Codes – Extensive Coding Guidance © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 13 APCs: Issues & Answers Increased Bundling CMS - Significantly Increased Bundling Long Federal Register Discussion • From Page 42667, August 2, 2007 – “Packaging costs into a single aggregate payment for a service, encounter, or episode of care is a fundamental principle that distinguishes a prospective payment system from a fee schedule. In general, packaging the costs of supportive items and services into the payment for the independent procedure or service with which they are associated encourage hospital efficiencies and also enables hospitals to manage their resources with maximum flexibility.” From a hospital’s perspective, is the above statement at all true? What are “supportive” items/services? What are “independent” procedures? How does this relate to ‘Separate Procedure Consolidation’ under APGs? Slide # 14 © 1999-2009 Abbey & Abbey, Consultants, Inc. APCs: Issues & Answers Increased Bundling CMS - Significantly Increased Bundling More detail on the bundling approach • From page 283 – Examination Copy CMS-1404-FC 2008 We use the term “dependent service” to refer to the HCPCS codes that represent services that are typically ancillary and supportive to a primary diagnostic or therapeutic modality. We use the term “independent service” to refer to the HCPCS codes that represent the primary therapeutic or diagnostic modality into which we package payment for the dependent service. We note that, in future years as we consider the development of larger payment groups that more broadly reflect services provided in an encounter or episode-of-care, it is possible that we might propose to bundle payment for a service that we now refer to as “independent.” Exercise: Compare and contrast the above concept with the APG (Ambulatory Patient Group) ‘significant procedure consolidation’. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 15 APCs: Issues & Answers Increased Bundling CMS Proposed Significantly Increased Bundling CMS want to increase bundling to have APCs be more of a Prospective Payment System (PPS) • Look more like DRGs? • Look less than RBRVS? Comment: For those familiar with APGs, Ambulatory Patient Groups, CMS purposefully moved APCs away from all the bundling in APGs. Now CMS is moving back toward the bundling in APGs. Why the change? (Hint: Think money!) o See APG concept of significant procedure consolidation. For the past several years, new interventional radiology codes have bundled the radiological component into the surgical component even at the CPT level. This is a major change. The discussions in the current APC Federal Register appear to be only the beginning. Also, movement from SI=“S” to SI=“T”. Why? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 16 APCs: Issues & Answers APC Category Changes New Composite APCs 8004 – Ultrasound Composite 8005 – CT and CTA w/o Contrast Composite 8006 – CT and CTA w Contrast Composite 8007 – MRI and MRA w/o Contrast Composite 8008 – MRI and MRA w Contrast Composite • See Imaging Families from 2006 for MPFS • CMS has now brought this packaging to the hospital outpatient setting as well as to physicians and IDTFS. • Financial Impact? 0034 – Mental Health Services Composite See Also PHPs © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 17 APCs: Issues & Answers APC Category Changes New APCs Closed Fracture Treatment Long-Term Problem Area • 0129 – Level I Closed Tx Fx Finger/Toe/Trunk $105.54 • 0138 – Level II Closed Tx Fx Finger/Toe/Trunk $406.12 • 0139 – Level III Closed Tx Fx Finger/Toe/Trunk $1,312.75 CMS has finally addressed the closed fracture treatment Strangely, CMS did not change the wording of the APCs to reflect coverage of more than fingers, toes, ribs, etc. Emergency Department • 0609-0615 – Type A ED Levels 1-4 • 0616 – ED Level 5 Common for Type A or Type B • 0626-0629 – Type B ED Levels 1-4 © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 18 APCs: Issues & Answers APC Category Changes Injections and Infusions (CPT Codes Have Changed Also) 6 APC Categories to 5 APC Categories For Drug Administration CY2008 CY2009 APC 0436 – Level I $ 16.21 $ 24.89 APC 0437 – Level II $ 25.13 $ 36.13 APC 0438 – Level III $ 51.22 $ 73.67 APC 0439 – Level IV $ 105.38 $ 128.62 APC 0440 – Level V $ 114.64 $ 187.96 APC 0441 – Level VI $ 149.34 Deleted OK, what does this mean? Did all the mappings change? Six Hour Infusion–96365+5*96366–CY2008 $114.64+$150.78=$265.42 CY2009$128.62+$124.45=$253.07 © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 19 APCs: Issues & Answers Status Indicator Codes Status Indicators (SIs) Have Become Increasingly Complex Increased use in APC logic for packaging including conditional packaging. “Q1” - STVX-Packaged Codes Paid under OPPS; Addendum B displays APC assignments when services are separately payable. • (1) Packaged APC payment if billed on the same date of service as a HCPCS code assigned status indicator “S,” “T,” “V,” or “X.” • (2) In all other circumstances, payment is made through a separate APC payment. “Q2” - T-Packaged Codes Paid under OPPS; Addendum B displays APC assignments when services are separately payable. • (1) Packaged APC payment if billed on the same date of service as a HCPCS code assigned status indicator “T.” • (2) In all other circumstances, payment is made through a separate APC payment. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 20 APCs: Issues & Answers Status Indicator Codes “Q3” - Codes That May Be Paid Through a Composite APC Paid under OPPS; Addendum B displays APC assignments when services are separately payable. Addendum M displays composite APC assignments when codes are paid through a composite APC. • (1) Composite APC payment based on OPPS composite-specific payment criteria. Payment is packaged into a single payment for specific combinations of service. • (2) In all other circumstances, payment is made through a separate APC payment or packaged into payment for other services. “R” – Blood and Blood Products – Paid Under OPPS, Separate Payment “U” – Brachytherapy Sources – Paid Under OPPS, Separate Payment Actually a Mini-APC System © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 21 APCs: Issues & Answers APC Policy Issues Blood and Blood Products Blood and Blood Products – An on-going problem area Coding for Blood and Transfusion Medicine Hospitals have been, and continue to be underpaid for blood and blood products. • Problems with cost reporting and CCRs • CMS is using a somewhat adjusted formula Here is an interesting and confusing statement from CMS: • “We continue to believe that using blood-specific CCRs applied to hospital claims data results in payments that appropriately reflect hospitals’ relative costs of providing blood and blood products as reported to us by hospitals. We do not believe it is necessary or appropriate to incorporate external survey data into our rate setting process for blood and blood products because, in a relative weight system, it is the relativity of the costs to one another, rather than absolute cost, that is most important for setting payment rates.” Page 168 CMS-1404-FC © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 22 APCs: Issues & Answers APC Policy Issues The 2-Times Rule APC=0060 - Manipulation Therapy APC=0080 - Diagnostic Cardiac Catheterization APC=0093 - Vascular Reconstruction/Fistula Repair without Device APC=0105 - Repair/Revision/Removal of Pacemakers, AICDs, or VDs APC=0141 - Level I Upper GI Procedures APC=0245 - Level I Cataract Procedures without IOL Insert APC=0303 - Treatment Device Construction APC=0330 - Dental Procedures APC=0341 - Skin Tests APC=0367 - Level I Pulmonary Test APC=0409 - Red Blood Cell Tests APC=0426 - Level II Strapping and Cast Application APC=0432 - Health and Behavior Services APC=0604 - Level 1 Hospital Clinic Visits © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 23 APCs: Issues & Answers APC Policy Issues Home Sleep Testing G0398, G0399, G0400 APC=0213 $153.05 Is it possible for anyone to send personnel, conduct the tests and not exceed costs of $153.05?? Variations and Changes in APCs Payment from Year-to-Year Ever since APCs were implemented there have been rather wild variations in payments from year-to-year, sometimes as much as a 60%-70% move up or down. CMS is aware of these variations, but CMS is adamant about using their approach of rate setting based on costs as reported by hospitals through the charges on claims and then converting the charges to costs via cost report information. The bottom-line answer from CMS is, “That’s just the way it turns out!” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 24 APCs: Issues & Answers APC Policy Issues Stereotactic Radiosurgery (SRS) “After consideration of the public comments received, we are finalizing our CY 2009 proposal, without modification, to continue to recognize Level II HCPCS codes G0251 and G0340, instead of CPT codes 77372 and 77373, for the reporting of SRS treatment delivery services under the OPPS in CY 2009. For CY 2009, HCPCS code G0251 is assigned to APC 0065 with a final APC median cost of approximately $931, and HCPCS code G0340 is assigned to APC 0066 with a final APC median cost of approximately $2,522. We also are finalizing our CY 2009 proposal to continue to recognize HCPCS codes G0173 and G0339, assigned to APC 0067 with a final median cost of approximately $3,718, for certain SRS services reported in accordance with the codes descriptors of these two HCPCS G-codes.” Page 493-CMS-14104-FC Replacement Codes for 6179361796-61800+63620+634621 © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 25 APCs: Issues & Answers APC Policy Issues Negative Pressure Wound Therapy – APC=0013 CPT=97605 – Negative pressure wound therapy, including topical application(s), wound assessment, and instruction(s) for ongoing car, per session; total wound(s) surface area less than 50 sq cm CPT=97606 - ; total wound(s) surface area greater than 50 sq cm • “After consideration of the public comments received, we are finalizing our CY 2009 proposal, without modification, to assign CPT codes 97605 and 97606 to APC 0013, with a final CY 2009 APC median cost of approximately $53.” Page 496 CMS-1404-FC APC-0013 - $54.70 HBOT – Hyperbaric Oxygen Therapy See C1300 Providers have claimed that CMS is underpaying CCR and Cost Reporting Problems “-CA” Modifier – Patient Expires, Inpatient-Only Procedure APC=0375 $5,672.92 (CY2008- $5,006.13) Keeps Going Up – Why? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 26 APCs: Issues & Answers APC Policy Issues Mental Health Services – APCs 0322, 0323, 0324, 0325 Partial Hospitalization Codes Versus Outpatient Codes • PHP – 90816-90829 • Outpatient – 90804-90815 • Outpatient Codes Status Indicator “Q3” – May be paid through a composite APC (APC=0034) “These codes are conditionally packaged when the sum of the payment rates for the single code APCs to which they are assigned exceeds the per diem payment rate for partial hospitalization.” Pages 507-508 CMS1404-FC • In other words, the outpatient codes 90804 through 90815 can be used an recognized, but there is a payment cap based on the composite APC=0034 $204.78 © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 27 APCs: Issues & Answers APC Policy Issues Trauma Response Associated with Critical Care (CPT=99291) APC=0617 Critical Care $485.39 APC=0618 Trauma Response with Critical Care $935.12 • “After consideration of the public comments received, we are finalizing our CY 2009 proposal, without modification, to pay separately for HCPCS code G0390 when billed with CPT code 99291, and to provide payment for HCPCS code G0390 through APC 0618, with a final CY 2009 APC median cost of approximately $914. We are also finalizing, without modification, our CY 2009 proposal to calculate the median cost for HCPCS code G0390 using our standard methodology that excludes those single claims for critical care services that are eligible for payment through the Level II extended assessment and management composite APC 8003.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 28 APCs: Issues & Answers APC Policy Issues Drugs, Biologicals and Radiopharmaceuticals Packaging drugs with daily cost less than $60.00. Following to be paid. • J0630 Calcitonin salmon injection • J1212 Dimethyl sulfoxide 50% 50 ML • J2513 Pentastarch 10% solution • J2515 Pentobarbital sodium inj • J2805 Sincalide injection • J2940 Somatrem injection • J2995 Inj streptokinase /250000 IU • J3350 Urea injection • J3473 Hyaluronidase recombinant • Q4102 Oasis wound matrix skin sub • Q4103 Oasis burn matrix skin sub • J8650 Nabilone oral • J9270 Plicamycin (mithramycin) inj • J9280 Mitomycin 5 MG inj • J9290 Mitomycin 20 MG inj • J9291 Mitomycin 40 MG inj • J9357 Valrubicin injection © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 29 APCs: Issues & Answers APC Policy Issues Drugs, Biologicals and Radiopharmaceuticals CMS is very interested in drug overhead costs For CY2008 – Consideration of three Drug Overhead Codes • “…, we did not finalize the proposal to instruct hospitals to separately report pharmacy overhead charges for CY 2008. Instead, in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66763), we finalized a policy of providing payment for separately payable drugs and biologicals and their pharmacy overhead at ASP+5 percent as a transition from their CY 2007 payment of ASP+6 percent to payment based on the equivalent average ASP-based payment rate calculated from hospital claims, which was ASP+3 percent for the CY 2008 OPPS/ASC final rule with comment period. Hospitals continued to include charges for pharmacy overhead costs in the line-item charges for the associated drugs reported on claims.” Page 605 CMS-1404-FC © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 30 APCs: Issues & Answers APC Policy Issues Drugs, Biologicals and Radiopharmaceuticals For CY2009, continue a transition to claims-based payment methodology. • “While payment at ASP+4 percent is slightly higher than the equivalent average ASP-based payment amount for all hospitals that we calculated from hospital costs according to the methodology we have used since CY 2006, we believe that another transitional payment year appropriately allows for a gradual change in hospital payment from the CY 2008 drug payment rate to a refined claims-based payment methodology. This CY 2009 transitional payment should help to ensure continued access to separately payable drugs and biologicals in the HOPD, while also providing us with another year to explore the complex issues surrounding hospital allocation of pharmacy overhead costs to drug charges and differential hospital drug costs based on hospital participation in the 340B program, in order to determine if a refined methodology could improve payment accuracy, while also ensuring equitable payments.” Page 635 CMS-1404-FC © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 31 APCs: Issues & Answers APC Policy Issues Drugs, Biologicals and Radiopharmaceuticals Radiopharmaceuticals • Continue with statutorily required APC categories • Look for ASP methodology for 2010. Other CPT to APC Grouping Issues Many limited issues involving certain areas – routine changes • Endovenous Ablations – APC=0091 and 0092 • Proton Beam Therapy – APC=0664 and 667 • Intercarpal or Carpometacarpal Arthroplasty – APC=0047 • Surgical Wrist Procedures – APC=0053 and 0054 • Arthroscopic and Other Orthopedic Procedures – APC=0041 and 0042 © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 32 APCs: Issues & Answers APC Policy Issues Devices On-going problem of Device Dependent APCs • Hospital must carefully assess charging methodologies to make certain CMS is receiving correct data. See Charge Compression. Example: Drug-Eluting Stents Removing Devices from Pass-Through List (i.e., start packaging) No Cost/Full Credit and Partial Credit Devices • See “FG” and “FC” Modifiers • See Table 21 for APCs and Percentages • Example – APC=0039, Level I Implantation ofNeurostimulator Device Offset No Cost/Full Credit – 84% Device Office Partial Credit – 42% © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 33 APCs: Issues & Answers APC Policy Issues Drug Administration Codes See Update Slides Nice synopsis from Page 694, CMS-1404-FC • During the development of new drug administration codes implemented by CPT in CY 2006, the AMA, the creators and maintainers of the Level I HCPCS codes (CPT codes), determined that the required resources and clinical characteristics of hydration services and therapeutic, prophylactic, and diagnostic drug administration services were sufficiently distinct to warrant different codes for the first hour of infusion and additional hours of infusion for these two types of services. Further, the AMA implemented a hierarchy for reporting drug administration services in the facility setting where chemotherapy services are primary to therapeutic, prophylactic, and diagnostic services, which are primary to hydration services. In addition, the hierarchy specifies that infusions are considered primary to pushes, which are considered primary to injections. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 34 APCs: Issues & Answers APC Policy Issues Drug Administration Codes See Update Slides Nice synopsis from Page 694, CMS-1404-FC - Continued • Just as the CPT codes are under the authority of the AMA, so are these instructions that preface the affected CPT codes and, in general, we adopt CPT instructions for reporting services under the OPPS. As discussed earlier, although reporting according to the hierarchy will first be specifically reflected in the CY 2008 OPPS claims data available for the CY 2010 OPPS update, we believe that the hierarchy detailed reporting practices that were already commonly being used by the majority of hospitals. We do not believe that the hierarchy implemented in CY 2008 for drug administration services substantially changed hospital billing practices in most cases, and we believe that our final CY 2009 payment rates for these services is appropriate for drug administration CPT codes reported in accordance with the specified hierarchy for CY 2009. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 35 APCs: Issues & Answers APC Policy Issues Emergency Department See Update Slides From Page 220, CMS-1404-FC • “The CY 2008 criteria and payment methodology finalized for composites APCs 8002 and 8003 will continue, consistent with the APC Panel’s August 2008 recommendation in support of our CY 2009 proposals for payment of extended assessment and management composite APCs. As discussed in section IX.B. of this final rule with comment period, we are also finalizing our proposal to reassign HCPCS code G0384 from APC 0608 (Level 5 Hospital Clinic Visits) to APC 0616 (Level 5 Emergency Visits). Moreover, we are finalizing our CY 2009 proposal, without modification, to include HCPCS code G0384 in the criteria that determine eligibility for payment of composite APC 8003, consistent with the APC Panel’s August 2008 recommendation that we should adopt this proposal.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 36 APCs: Issues & Answers APC Policy Issues Emergency Department See Update Slides From Page 221, CMS-1404-FC • “Finally, as discussed in section XIII.A.1, of this final rule with comment period, we are finalizing our CY 2009 proposal to replace current status indicator “Q” with three new separate status indicators: “Q1,” “Q2,” and “Q3.” Therefore, each of the direct admission, clinic, and emergency department visit codes that may be paid through composite APCs 8002 and 8003 are assigned status indicator “Q3” (Codes that May be Paid Through a Composite APC) for CY 2009 in Addendum B to this final rule with comment period.” See also, Status Indicator Slides © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 37 APCs: Issues & Answers APC Policy Issues Emergency Department See Update Slides From Page 222, CMS-1404-FC • “In the CY 2009 OPPS/ASC proposed rule (73 FR 41444), we also proposed that the payment policy for separate payment of HCPCS code G0379 that was finalized for the CY 2008 OPPS (72 FR 66814 through 66815) would continue to apply for CY 2009 when the criteria for payment of this service through composite APC 8002 are not met. The criteria for payment of HCPCS code G0379 under either composite APC 8002, as part of the extended assessment and management composite service, or APC 0604, as a separately payable individual service are: (1) both HCPCS codes G0378 and G0379 are reported with the same date of service; and (2) no service with a status indicator of “T” or “V” or Critical Care (APC 0617) is provided on the same date of service as HCPCS code G0379. If either of the above criteria is not met, HCPCS code G0379 is assigned status indicator “N” and its payment is packaged into the payment for other separately payable services provided in the same encounter.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 38 APCs: Issues & Answers APC Policy Issues Electrophysiological Studies Concern has been expressed about the EP APC Composite 8000 Continue to use APC 0085 and 0086 using single procedure claims. SI=“Q” moved to SI=“Q3” From Page 231, CMS-1404-FC • “We continue to believe that the composite APC for cardiac electrophysiologic evaluation and ablation services is the most efficient and effective way to use the claims data for the majority of these services and best represents the hospital resources associated with performing the common combinations of these services that are clinically typical. Furthermore, this approach creates incentives for efficiency by providing a single payment for a larger bundle of major procedures when they are performed together, in contrast to continued separate payment for each of the individual procedures.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 39 APCs: Issues & Answers APC Policy Issues Mental Health Composite APC 0034 $204.78 From Page 235, CMS-1404-FC • “For CY 2009, as discussed further in section X.B. of this final rule with comment period, we proposed to create two new APCs, 0172 (Level I Partial Hospitalization (3 services)) and 0173 (Level II Partial Hospitalization (4 or more services)), to replace APC 0033 (Partial Hospitalization), which we proposed to delete for CY 2009 (73 FR 41446). In summary, when a community mental health center (CMHC) or hospital provides three units of partial hospitalization services and meets all other partial hospitalization payment criteria, the CMHC or hospital would be paid through APC 0172. When the CMHC or hospital provides four or more units of partial hospitalization services and meets all other partial hospitalization payment criteria, the hospital would be paid through APC 0173. In the CY 2009 OPPS/ASC proposed rule (73 FR 41446 through 41447), we proposed to set the CY 2009 payment rate for mental health composite APC 0034 at the same rate as APC 0173, which is the maximum partial hospitalization per diem payment.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 40 APCs: Issues & Answers APC Policy Issues Mental Health Composite APC 0034 $204.78 From Pages 239-240, CMS-1404-FC • “After consideration of the public comments received, we are finalizing our CY 2009 proposal, without modification, to limit the aggregate payment for specified less intensive outpatient mental health services furnished on the same date by a hospital to the payment for a day of partial hospitalization, specifically APC 0173. For CY 2009, we are also finalizing, without modification, our proposal to change the status indicator from “Q” to “Q3” for those HCPCS codes that describe the specified mental health services to which APC 0034 applies. For CY 2009, we also are finalizing the proposal to change the status indicator for APC 0034 from “P” to “S.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 41 APCs: Issues & Answers APC Policy Issues Technical Component E/M Coding Hospitals should not anticipate any technical component E/M guidelines in the near future! • This places hospitals at significant compliance risk. • Auditors can easily claim that hospital-developed mappings encourage upcoding and overpayments. • MAC’s using their own guidelines and not the hospital-developed guidelines? • From Page 738 CMS-1404-FC “In addition, we note our continued expectation that hospitals’ internal guidelines will comport with the principles listed in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66805). We encourage hospitals with more specific questions related to the creation of internal guidelines to contact their local fiscal intermediary or Medicare Administrative Contractor (MAC).” o Get your mapping ‘approved’?? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 42 APCs: Issues & Answers APC Policy Issues Technical Component E/M Coding New versus Established Patient • This is a surprising long discussion of this topic – • “Specifically, the meanings of “new” and “established” patients would pertain to whether or not the patient has been registered as an inpatient or outpatient of the hospital within the past 3 years. Under this proposed modification, hospitals would not need to determine the specific clinic where the patient was previously treated because the modified definition would not rely upon when the medical record was initially created but rather, would depend upon whether the individual has been registered as a hospital inpatient or outpatient within the previous 3 years.” Page 710 CMS1404-FC. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 43 APCs: Issues & Answers APC Policy Issues Inpatient-Only Listing Well, virtually every commenter over the last several years has suggested elimination of the Inpatient-Only list. • ‘We appreciate the comments and understand the commenters’ reasons for advocating the elimination of the inpatient list. However, we continue to believe that the inpatient list serves an important purpose in identifying procedures that cannot be safely and effectively provided to Medicare beneficiaries in the HOPD. We are concerned that elimination of the inpatient list could result in unsafe or uncomfortable care for Medicare beneficiaries. Therefore, we are not discontinuing our use of the inpatient list at this time. In addition to the above concerns about differences in physician and hospital outpatient payment policy, hospitals have expressed ongoing concerns related to inpatient procedures being performed inappropriately for beneficiaries who are not inpatients and that, as a result, beneficiaries may be liable for the charges for the services. We believe that it is the responsibility of physicians and hospitals to know which procedures are on the inpatient list.” Page 803 CMS1404-FC. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 44 APCs: Issues & Answers APC Policy Issues Quality Reporting – Now and In The Future CY2009 Increase – 3.9% Except for those that don’t meet the requirements of HOP QDRP – 1.9% • Separately Payable Items (Drugs, Devices, New Technology, Radiopharmaceutical and Brachytherapy Sources) Not Affected New Quality Measures – 2008-2009-2010 • 11 Measures in 2009 • New Imaging Efficiency Measures • 18 Potential Quality Measures – Cancer Care, ED Throughput, Screening for Fall Risk, Management of Clinical Conditions (Depression, Stroke, Osteoporosis, Asthma, Pneumonia) Validation of Quality Reporting – Voluntary Hospitals Healthcare-Associated Conditions – Analog to IPPS Payment Reduction © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 45 APCs: Issues & Answers Ambulatory Surgical Centers ASCs Payment is a combination of APCs and RBRVS Payment Rates Still in a 4-year phase-in process Covered Surgical Procedures Must know what can be performed: • In a physician’s office, • The ASC, • Only in the hospital. ASC Conditions for Coverage (CfCs) Not exceed 24 hours Physician financial interests Governing Body Infection Control Pre-Surgery Assessment © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 46 APCs: Issues & Answers Special Issues Charges, Cost-to-Charge Ratios (CCRs) and Cost Reporting CMS had RTI conduct studies of the Charge Compression issue. Both APC and DRG weight calculations are affected. From Page 89 CMS-1404-FC – • “RTI’s first set of recommendations for accounting changes addressed improved use of existing cost report and claims data. RTI recommended: (1) immediately using text searches of providers’ line descriptions to identify provider-specific cost centers and ultimately to more appropriately classify nonstandard cost centers in current hospital cost report data; (2) changing cost report preparation software to impose fixed descriptions on nonstandard cost centers; (3) slightly revising CMS’ cost center aggregation table to eliminate duplicative or misplaced nonstandard cost centers and to add nonstandard cost centers for common services without one; and (4) adopting RTI’s recommended changes to the revenue code-to-cost center crosswalk.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 47 APCs: Issues & Answers Special Issues Charges, Cost-to-Charge Ratios (CCRs) and Cost Reporting From Page 101, CMS-1404-FC • “Numerous commenters expressed support for the use of regression-adjusted CCRs for devices in order to improve shortterm accuracy in the OPPS relative payment weights by addressing charge compression arising from use of a single CCR for supplies and devices. These commenters viewed regression-adjusted CCRs as a suitable temporary adjustment for charge compression until CCRs for the new Implantable Devices Charged to Patients cost center, finalized in the FY 2009 IPPS final rule (73 FR 48458 through 48469), become available in CY 2012 or CY 2013. Many commenters saw regression-adjusted CCRs for devices as a necessary solution that would be immediately available and appropriate, especially because they believed that other options, such as provider education, could not address the issue of highly variable markup rates compressed by a single CCR during cost estimation.” © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 48 APCs: Issues & Answers Special Issues Device Dependent APCs – Examples 0039 - Level I Implantation of Neurostimulator 0040 - Percutaneous Implantation of Neurostimulator Electrodes 0061 - Laminectomy, Laparoscopy, or Incision for Implantation of Neurostimulator Electrodes 0082 - Coronary or Non Coronary Atherectomy 0083 - Coronary or Non Coronary Angioplasty and Percutaneous Valvuloplasty 0089 - Insertion/Replacement of Permanent Pacemaker and Electrodes 0090 - Insertion/Replacement of Pacemaker Pulse Generator 0104 - Transcatheter Placement of Intracoronary Stents 0106 - Insertion/Replacement of Pacemaker Leads and/or Electrodes 0107 - Insertion of Cardioverter-Defibrillator 0108 - Insertion/Replacement/Repair of Cardioverter-Defibrillator Leads © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 49 APCs: Issues & Answers Special Issues Classifying Claims Note: Generally, only singleton claims (i.e., claims that group to only one APC) can be included in the calculations for APC weights. Using the newer Status Indicator codes, CMS can increase the number of claims going into the calculations. • Single Major Claims • Multiple Major Claims • Single Minor Claims • Multiple Minor Claims • Non-OPPS Claims Packaged Revenue Codes This listing, which is only partially used, hasn’t really changed over time. For instance, RC=0390 is on the list, but services are not packaged. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 50 APCs: Issues & Answers Special Issues Direct Physician Supervisions – Provider-Based Clinics Strangely, the topic of direct physician supervision for provider-based clinic has become a topic. April 7, 2000 CMS (then HCFA) created the Provider-Based Rule found at 42 CFR §413.65 • For off-campus provider-based clinics, direct physician supervision was a special obligation • For in-hospital or on-campus clinics, physician supervision was assumed (i.e., there would be a qualified practitioner close by in case of problems). Now CMS is maintaining that the direct physician supervision also applies to on-campus and in-hospital situations. • CMS is indicating that this is not new!? • WHAT does this really mean? © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 51 APCs: Issues & Answers Summary and Conclusions APCs Represent CMS’s Most Complex Prospective Payment System We are into the Tenth Year (Depending on how you count) of APCs – The variation in payments continues to be a roller coaster Significant policy changes continue to be developed, specifically increased packaging and more composite APCs Hospital charging structures and CCRs are now in the limelight both from the public as well as how they impact APC weight development Proper chargemaster construction along with proper coding interfaces and charge capture are of great importance Correct CPT/HCPCS coding along with proper use of modifiers continues to paramount While there continue to be areas of difficulty (e.g., technical component E/M levels), CMS is whittling away as issues Hospitals should anticipate that APCs will continue to change at a rapid pace during the coming years. © 1999-2009 Abbey & Abbey, Consultants, Inc. Slide # 52